
Does breastfeeding prevent postnatal depression?
Peer reviewed by Dr Sarah Jarvis MBE, FRCGPLast updated by Sara LindbergLast updated 7 Nov 2017
Meets Patient’s editorial guidelines
- DownloadDownload
- Share
- Language
- Discussion
There are numerous benefits breastfeeding offers a new mum, including the ability to bring you closer to your baby. But what about helping in the fight against postnatal depression? Can breastfeeding lessen the severity of symptoms that accompany this debilitating condition?
In this article:
Continue reading below
Baby blues
Postnatal depression is a mood disorder that can affect women after childbirth. Mothers with postnatal depression experience feelings of extreme sadness, anxiety, and exhaustion that may make it difficult for them to complete daily care activities for themselves or for others.
Often, these feelings are attributed to the 'baby blues', which many women experience in the two weeks following childbirth. However, if it is just the baby blues, the anxious, tearful, and feeling down moments will subside and mum will begin to feel like herself again. If the symptoms last longer or start later, you could be dealing with postnatal depression.
Some of the more common symptoms of postnatal depression include:
Persistent sadness.
Feeling hopeless and overwhelmed.
Irritability.
Restlessness.
Crying more often for no apparent reason.
Difficulty bonding with your baby.
Doubting your ability to care for your baby.
Oversleeping and chronic fatigue (beyond what is normal for a new mum).
In more severe cases, thinking about harming yourself or your baby.
According to the World Health Organization (WHO), worldwide about 10% of pregnant women and 13% of women who have just given birth experience a mental disorder, primarily depression. In developing countries this number is even higher: in the USA, the Center for Disease Control reports that about 1 in 9 women experience postpartum (postnatal) depression, and in the UK, the NHS reports that 1 in every 10 women will experience postnatal depression within a year of giving birth.
Unfortunately, many women do not tell their doctor they are experiencing any symptoms, so the numbers could potentially be much higher. But, for the women who are diagnosed, many are desperate for ways to reduce the severity of the symptoms that ail them almost daily.
And while most experts will recommend a combination of psychotherapy, medication, and self-help remedies (exercise, rest, healthy eating, asking for help, etc) to treat postnatal depression, experts have recently begun to look at the role breastfeeding plays in decreasing postnatal depression.
What's the evidence?
It helps
We all know the benefits of breastfeeding for both baby and mum. But could putting baby to breast help lessen the severity of symptoms women experience - or maybe even prevent postnatal depression from happening at all?
A study from 2010 showed that women who breast-fed their babies were at a significantly lower risk of postnatal depression than those who did not. The research was conducted by researchers in the UK and Spain and included over 10,000 mothers.
Specifically, the authors discovered that the majority of mothers who were not depressed during pregnancy, and who planned to breastfeed their babies (and went on to do so), had a decreased risk of developing postnatal depression.
One theory of why breastfeeding may decrease postnatal depression has to do with hormones. Rachel Borton, director of the Family Nurse Practitioner Program at Bradley University explains that:
"The breastfeeding act itself or let-down act of breast milk causes the body to release a hormone called oxytocin and this hormone is also known as the 'feel-good' hormone.
"Postpartum depression is often triggered by the dramatic drop in hormone levels following delivery of an infant and oxytocin acts as an antidepressant and helps to decrease postpartum depression."
Or does it?
Sounds amazing, right? Just put baby to breast, release those 'feel-good' hormones, and fight off depression - all at the same time. Unfortunately, it's not always that easy. While many women will experience a decrease in symptoms or avoid developing postnatal depression altogether, in some cases, breastfeeding may actually worsen the symptoms of postnatal depression.
"If mum is experiencing postnatal depression and the baby is not gaining weight well or having difficulty breastfeeding, it can make the symptoms worse," says Deedee Franke, a lactation consultant at Mercy Medical Center in Baltimore.
"Any problems that mum is encountering while she breastfeeds may enhance the symptoms of postnatal depression and/or anxiety."
And Franke is not alone in her thinking: The same study that reported how breastfeeding can have a protective effect also noted that problems with breastfeeding can increase postnatal depression in some women.
What if you're at high risk of depression?
But what about the extremely vulnerable population of women who are depressed and/or anxious before giving birth?
Researchers have discovered an association between maternal symptoms of anxiety and depression and stopping breastfeeding early. Not only were the women who were depressed and/or anxious during pregnancy more likely to stop breastfeeding early, they were more likely to experience worsening of their symptoms after cessation of breastfeeding.
Continue reading below
What if you can't breastfeed?
Some mums want to breastfeed but can't due to low supply, suckling issues, or medication they're taking which means they shouldn't. And if the overall message these women hear is 'breast is best' then it's no surprise they are at a higher risk of developing postnatal depression.
Yet, other mums who experience postnatal depression have said that breastfeeding is the only thing that helped them feel close to their child - which consequently reduced the severity of their depressive symptoms.
The lowdown
So, with evidence supporting both theories, what conclusions can we draw? Well, one universal result of the research is that new mums who are at risk of developing postnatal depression need expert guidance when it comes to breastfeeding: this includes women who are able to breastfeed and women who plan to breastfeed but later discover they can't. These mums need the continual support and encouragement of their healthcare team to develop the best treatment plan for battling postnatal depression.
Patient picks for Depression

Mental health
Are mental health problems in new mothers being missed?
A UK parenting charity is calling for better support for new mothers who are struggling with mental health problems.
by Milly Evans
Mental health
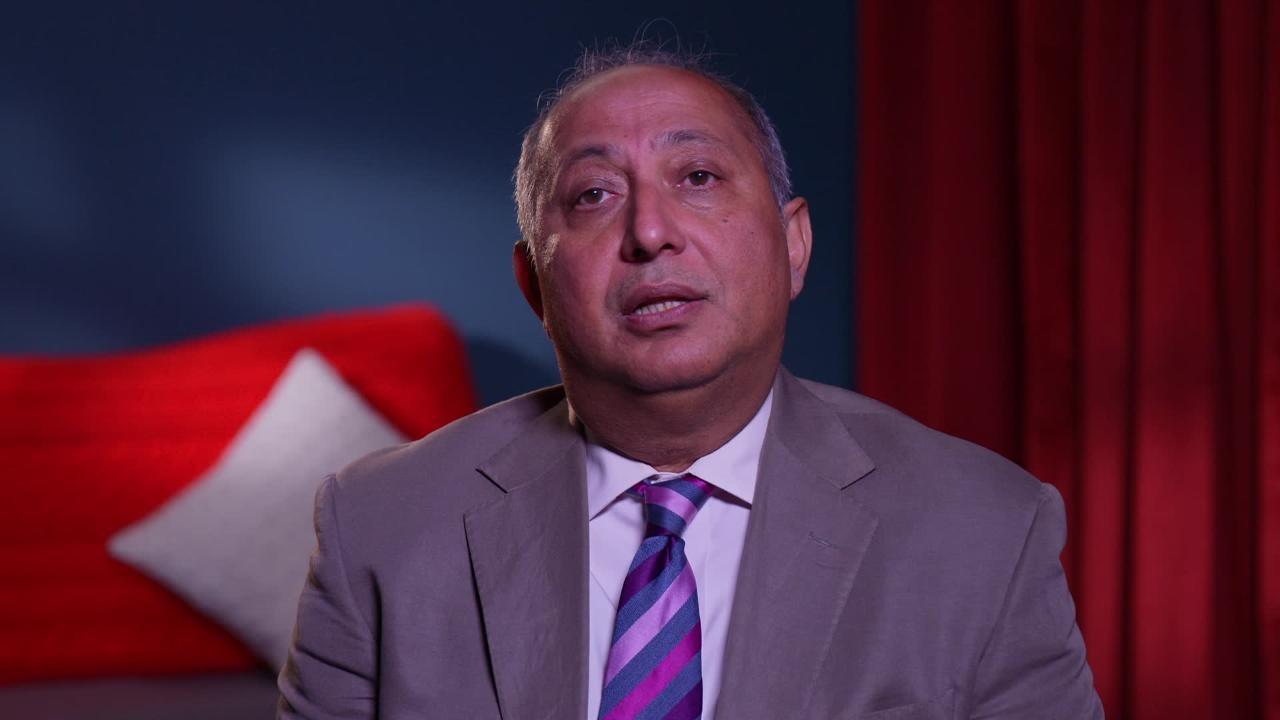
Video: Why do people get depressed?
With a condition as complicated as depression, two cases are rarely the same and the underlying reasons why you or those close to you are affected may need professional support to uncover. We may not be able to offer all the answers, but our experts have tackled some of the common questions that arise.
by Prof Swaran Singh, FRCPsych
Article history
The information on this page is peer reviewed by qualified clinicians.
7 Nov 2017 | Latest version

Ask, share, connect.
Browse discussions, ask questions, and share experiences across hundreds of health topics.

Feeling unwell?
Assess your symptoms online for free
Sign up to the Patient newsletter
Your weekly dose of clear, trustworthy health advice - written to help you feel informed, confident and in control.
By subscribing you accept our Privacy Policy. You can unsubscribe at any time. We never sell your data.