Intrauterine contraceptive device
The coil
Peer reviewed by Dr Colin Tidy, MRCGPLast updated by Dr Rosalyn Adleman, MRCGPLast updated 1 Mar 2023
Meets Patient’s editorial guidelines
- DownloadDownload
- Share
- Language
- Discussion
- Audio Version
In this series:Long-acting reversible contraceptivesContraceptive implantContraceptive injectionLevonorgestrel intrauterine device
An intrauterine device (IUD) is a small device made from plastic and copper which sits inside the womb (uterus). It is also known as the coil.
In this article:
Video picks for Long-acting reversible contraceptives
Continue reading below
What is an intrauterine device?
An intrauterine device (IUD) is a small device made from plastic and copper which sits inside the womb (uterus). It is also known as "the coil". Two threads are attached to the IUD and pass out through the neck of the womb (cervix) to lie in the vagina. These allow the IUD to be removed easily. Most devices are T-shaped (the two arms of the T fold flat for insertion) and are about as long as a matchstick. The inside of the womb itself is only a little longer than a matchstick, so the device sits neatly inside.
How does the intrauterine device work?
Back to contentsIt works mainly by making it difficult for sperm to fertilise an egg. This is an effect of the copper in the device. It makes the mucus at the neck of the womb (cervix) and the womb lining itself hostile to sperm and eggs. This means that it prevents sperm getting in through the cervix, and from travelling through the womb (uterus). It also makes your womb lining much less likely to accept an egg.
The IUD does not cause an abortion (which occurs when a pregnancy is ended after the fertilised egg as planted in the wall of the womb).
Continue reading below
How effective is the intrauterine device?
Back to contentsModern IUDs are very effective. Only 1-2 of every 100 women using the IUD as contraception will become pregnant over five years of use.
By comparison to this, more than 80 of every 100 sexually active women who do not use contraception become pregnant within one year.
How long will the intrauterine device work for?
Back to contentsThere are many different types of IUD. Most copper IUDs work well for at least five years, and many types now work for ten years. If you were over 40 years old when the device was fitted it can be assumed to last until your menopause.
Continue reading below
Why would I choose an intrauterine device?
Back to contentsOnce an IUD is inserted you no longer need to use other contraception. So, unlike users of contraceptive pills, you don't need to think about contraception every day.
The IUD does not interfere with sex (intercourse) or sex drive (libido). It is not a hormonal method so it has no side-effects on the rest of the body. This means that it will not affect your mood, weight or libido. This lack of side-effects is one of the reasons many women choose it.
Having an IUD does not increase your risk of having any type of cancer in the future.
Because it does not contain hormones, if they wish to, most women can have an IUD. There are a few situations where an IUD is not recommended. Your doctor or nurse will make sure it is safe for you to use an IUD, by asking questions about your health.
Where do I go to get an intrauterine device?
Back to contentsIn the UK, the IUD may be offered at your local GP surgery or at asexual health/family planning clinic- see Further Reading below. You will need to make an appointment.
How is the intrauterine device fitted?
Back to contentsThis is usually done towards the end of a period or shortly afterwards, as this tends to be more comfortable for you. Also, the doctor can be sure that you are not pregnant. However, it can be fitted at any time provided that you are certain you are not pregnant.
You will need to have a vaginal examination. The doctor or nurse will pass a small instrument into your womb (uterus) to check its size and position. The IUD is then fitted using a small plastic insertion device. You will be taught how to feel the threads of the IUD so you can check it is in place. It is best to check the threads regularly - for example, once a month just after a period.
Intrauterine device
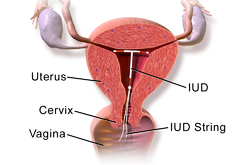
© "Medical gallery of Blausen Medical 2014". WikiJournal of Medicine 1 (2). DOI:10.15347/wjm/2014.010. ISSN 2002-4436., CC BY 3.0, via Wikimedia Commons
By Blausen.com staff (2014). "Medical gallery of Blausen Medical 2014". WikiJournal of Medicine 1 (2). DOI:10.15347/wjm/2014.010. ISSN 2002-4436., CC BY 3.0, via Wikimedia Commons
The process of fitting an IUD can sometimes be very uncomfortable. Once the IUD has been inserted, some women have crampy pains like period pains for a few hours (and up to 48 hours) afterwards. These can be eased by painkillers such as paracetamol or ibuprofen, and it can be sensible to take these an hour before your fitting. Light vaginal bleeding may also occur for a short while.
How quickly does the intrauterine device work?
Back to contentsOnce the IUD is in place it works immediately. However, when it is fitted there is a very small chance that your body will expel it again. If this happens it usually happens in the first 24-48 hours.
Do I need follow-up?
Back to contentsThe doctor or nurse will usually want to check that there are no problems a few weeks after fitting an IUD. It is best done after your next period. After this, there is no need for any routine check until it is time to remove the IUD. However, return to see your doctor or nurse at any time if you have any problems or queries. Most women have no problems, and the IUD can remain in place for several years.
You should consult a doctor if any of the following occur:
Prolonged tummy (abdominal) pain (severe or beyond 48 hours) after an IUD is inserted.
A delayed period, or bleeding between periods.
A delayed period and lower or one-sided tummy (abdominal) pain (which may be due to an ectopic pregnancy).
Vaginal discharge with or without pain (which may indicate infection).
If you suspect that the IUD has come out or is coming out. It is usually possible to feel the threads of the IUD inside the vagina to check it is in place. If you cannot feel the threads then use other contraceptive methods (such as condoms) until you have been checked by a doctor or nurse.
What are the side-effects or risks of the intrauterine device?
Back to contentsAlthough the majority of women with an IUD have no problems, the following may occasionally occur as side-effects or consequences.
Heavy, painful periods
Some women find that their periods become heavier, longer or more painful with an IUD. This tends to be in the first few months after insertion and then often settles. This means that the IUD may not be suitable if you already have heavy or painful periods. There is a special intrauterine contraceptive called the intrauterine system (IUS), which is like an IUD but it also releases a hormone into the womb (uterus). This is an effective treatment for heavy periods as well as being a contraceptive. Read more about the intrauterine system.
If you have painful, heavy periods with an IUD in place this can still be treated in the same way as in women who do not have an IUD. For example, your doctor may prescribe anti-inflammatory painkillers or other medicines to take just before and during your periods.
Infection
There is a risk of worsening an existing infection of the womb (pelvic infection) when you have an IUD inserted. A check for infection of the vagina or neck of the womb (cervix) may be advised by taking a sample (swab) before an IUD is inserted. The doctor or nurse fitting the device may ask you some intimate questions about your sex life in order to determine whether it might be sensible to do a swab or urine tests. If there is thought to be a risk, you may be given antibiotics at the time the IUD is fitted.
Ectopic pregnancy
The chance of becoming pregnant is very small if you use an IUD. However, if you do become pregnant, your doctors will need to check this is not an ectopic pregnancy (a pregnancy in the Fallopian tube and not in the womb). This is because IUD prevents ectopic pregnancy slightly less well than it prevents normal (uterine) pregnancy. However the risk of ectopic pregnancy is not increased by IUD compared to no contraception - it is in fact decreased by it.
The IUD does not cause ectopic pregnancy. However, whilst it is very effective at preventing intrauterine pregnancy, it is less effective at preventing ectopic pregnancy. This means that those pregnancies that do develop with an IUD in the womb have a significant chance of being ectopic. See a doctor urgently if you miss a period (or your period is light and prolonged) and you develop lower, one-sided tummy (abdominal) pain.
Expulsion
Rarely, the IUD may come out without you noticing. This may happen during a period, most commonly in the first three months after fitting. It is slightly more likely to happen if you have not had children or if the fitting was particularly uncomfortable.
It is a good idea to check you can feel the threads of the IUD after your period. If you cannot feel them, you should use extra precautions such as a condom, until your doctor has checked the IUD is still there.
If the IUD has come out in the last few days you may need emergency contraception. If the IUD could have come out more than a few days ago, and you are sexually active, the doctor will make sure you are not already pregnant before fitting another one or starting alternative contraception.
Lost threads
When the IUD is inserted the threads dangle out of the neck of the womb (cervix). They will often come to lie against the cervix, in the cervical mucus, and you or your partner should not notice them unless you feel for them. The threads allow you to check that the IUD is still in place, and when the IUD is removed they are used to pull it gently out.
Occasionally, however, the threads are lost. This can either mean that:
The threads have come off the device, and the device is still in place.
The device is in the right place but the threads have got tucked up behind it.
The device has moved further into the womb so that the threads can no longer be felt.
The device has come out.
If you cannot feel the threads it is important to use other forms of contraception (if you don't wish to become pregnant) until you can be checked to find out what has happened. You may also need emergency contraception.
An ultrasound examination will show whether the IUD is where it should be. If it has come out then it can be replaced, as long as you are not pregnant. If it is still in place but has lost its threads then it can remain there. When the time comes to remove it, doctors experienced in removal of IUDs with lost threads will advise you on whether this can be done in clinic, or whether you might need a short procedure under anaesthetic to take it out.
Damage to the womb
The fitting of an IUD can, very rarely, make a small hole in the womb - this is called perforation. It protrudes through the wall of the womb and can escape into the pelvis. This happens in fewer than 2 women per 1,000, usually at the time of fitting. It can cause pain but this is not usually severe and often there is no pain. The main symptom is not being able to feel the threads.
You should tell your doctor or nurse if you can no longer feel the threads of your IUD. This can mean perforation has occurred. However, more commonly it means either that the threads are tucked up inside the cervix or (less commonly) the threads have come off the device. An ultrasound scan will be carried out to find a lost IUD. If ultrasound does not find the IUD, an X-ray will be ordered.
How do you remove or change an intrauterine device?
Back to contentsAn IUD can be removed at any time by a trained doctor or nurse. If you plan to have it removed but do not want to get pregnant, you should abstain from having sex (intercourse). Or, you should use other methods of contraception (such as condoms) for seven days before the IUD is removed. This is because sperm can last up to seven days in the womb (uterus) and can fertilise an egg after the IUD is removed.
If you have had your IUD for its maximum effective time (usually five or ten years, depending on the device) and you need, therefore, to have it changed for another one, you should again abstain from having sex. Or, you should use other forms of contraception for seven days before removal. This is because occasionally when the device is removed, the neck of your womb (cervix) clamps tightly shut for a while. If this does happen, the doctor cannot immediately insert the new device. As sperm can last up to seven days in the womb, they could, therefore, fertilise an egg whilst you are waiting for your replacement IUD fitting.
Can I exercise with the device in place?
Back to contentsThe IUD's initial side-effects can include cramps and back pain after insertion. Usually, these symptoms last only a few hours, so you may need to wait until the next day to exercise as usual. Some women, however, experience bleeding, cramping and pain for a couple of weeks, and may wish to wait longer. However, there is no medical reason to avoid exercise after insertion of an IUD.
Some gyms advise that women with an IUD should not use vibrating gym plates because of theoretical concerns about an increased risk of expulsion caused by the vibrations. There is no evidence that this can occur but women are advised to avoid such activity in the first few weeks following insertion when the expulsion rate is highest.
Can the intrauterine device be used as emergency contraception?
Back to contentsThe IUD is a very effective form of emergency contraception which is effective for up to five days after you have had unprotected sex (intercourse). It prevents more than 9 out of 10 pregnancies which would otherwise have occurred. It can be left in place to provide ongoing contraception.
The IUD is the most effective method of emergency contraception - but it is not available everywhere, not all doctors are able to fit it and there may not be emergency appointments available at just the right time. Therefore, if you need emergency contraception it is important to try to make arrangements for this as early as possible.
If you don't want to continue to use the IUD as contraception it can be removed after you have had your next period.
Is there anyone who should not have the intrauterine device?
Back to contentsThe IUD is not generally considered the best choice of contraceptive for those who already have heavy, painful periods, as it is likely to make this worse. In this case you may be better to consider an intrauterine system (IUS), which is a similarly shaped device which contains progestogen rather than copper.
The IUD should not be put in if you are pregnant, have unexplained vaginal bleeding or vaginal or pelvic infection, or if you are known to have an abnormally shaped womb. It is also not advisable if you have any form of cancer affecting the pelvis.
If you have previously become pregnant with an IUD in your womb, you might wish to choose another method for the future.
Can the intrauterine device be used when breastfeeding?
Back to contentsYes, the IUD can be used when breastfeeding.
Although breastfeeding alone can delay the return of your periods and does slightly reduce the chance of another pregnancy, it is not a reliable contraceptive and it is possible to become pregnant whilst breastfeeding even before you have a period.
Can the intrauterine device be put in after miscarriage or termination?
Back to contentsThe IUD can be put in immediately after miscarriage or termination of pregnancy in most cases.
Can the intrauterine device be put in after childbirth?
Back to contentsThe IUD can be inserted straight after caesarean section or vaginal delivery, after the placenta is delivered (and as long as your delivery is not complicated by heavy bleeding or infection).
For women who would like to use an effective contraceptive straight after childbirth, this can be extremely convenient, as insertion is unlikely to be uncomfortable. The IUD is not recommended between 48 hours and four weeks after delivery.
Beyond four weeks after delivery, the IUD can be inserted safely.
Can I use tampons with an intrauterine device?
Back to contentsYou can use sanitary towels or tampons with an IUD in place. A cervical smear can also be taken with an IUD in place. Sometimes, the smear result may show that there is an organism in the cervix; these are called actinomyces-like organisms. These are normally found in the vagina and do not mean the IUD should be removed. If you have had pelvic pain together with signs of infection, such as a temperature, your doctor may consider removing the IUD.
Can I use a menstrual cup with an intrauterine device?
Back to contentsMooncup® is a silicone cup designed to sit over the cervix to catch menstrual blood, as an alternative to tampons and sanitary pads.
The Mooncup® manufacturer recommends waiting six weeks after the insertion of your IUD before using the cup. They also recommend checking for IUD threads after each menses. They say that there have been instances where an IUD/intrauterine system (IUS) has become dislodged when using the devices together, possibly due to wearing the cup too high, or the cervix being very low. One in twenty IUDs/IUS will be expelled, most commonly in the first three months after the device has been inserted. These expulsions happen most frequently during menstruation. This is generally thought not to be due to the Mooncup®.
There should always be a space between the Mooncup® and the cervix. If you have a low-sitting cervix there may not be enough room for the cup to sit safely and work effectively. You should always place the Mooncup® low in the vagina and ensure you have an adequate seal. Always release the seal before removing.
If I have an intrauterine device, what do I do when I want to try to get pregnant?
Back to contentsIf you feel you would like to try for a baby, you will need to have the IUD removed. Your fertility will return immediately and if your periods have been heavier than before they will usually return to normal after a couple of cycles. It is possible to get pregnant before you have your first period. This is because you produce an egg two weeks before a period occurs.
If you want to try for a baby, start pre-pregnancy care such as taking folic acid, stopping smoking and reviewing your medication. You can ask your doctor or nurse for further advice.
Dr Mary Lowth is an author or the original author of this leaflet.
Patient picks for Long-acting reversible contraceptives

Sexual health
Contraceptive injection
The contraceptive injection contains a progestogen hormone. It is used to prevent pregnancy.
by Dr Caroline Wiggins, MRCGP

Sexual health
Levonorgestrel intrauterine device
The levonorgestrel intrauterine device (LNG-IUD), previously known as the intrauterine system (IUS) is a small, flexible, plastic device which sits inside the womb (uterus). There are two threads attached to it which pass out through the neck of the womb.
by Dr Toni Hazell, MRCGP
Further reading and references
- Long-acting reversible contraception; NICE Clinical Guideline (October 2005 - updated July 2019)
- Trussell J; Contraceptive failure in the United States, Contraception, 2011
- Intrauterine Contraception; Faculty of Sexual and Reproductive Healthcare Clinical Effectiveness Unit (March 2023 - last updated July 2023)
- UK Medical Eligibility Criteria Summary Table for intrauterine and hormonal contraception; Faculty of Sexual and Reproductive Healthcare, 2016 - amended September 2019
- Find a sexual health clinic near you; NHS services
Continue reading below
Article history
The information on this page is written and peer reviewed by qualified clinicians.
Next review due: 6 Jan 2028
1 Mar 2023 | Latest version

Ask, share, connect.
Browse discussions, ask questions, and share experiences across hundreds of health topics.

Feeling unwell?
Assess your symptoms online for free
Sign up to the Patient newsletter
Your weekly dose of clear, trustworthy health advice - written to help you feel informed, confident and in control.
By subscribing you accept our Privacy Policy. You can unsubscribe at any time. We never sell your data.