Achilles tendinopathy
Peer reviewed by Dr Hayley Willacy, FRCGP Last updated by Dr Doug McKechnie, MRCGPLast updated 26 Jul 2023
Meets Patient’s editorial guidelines
- DownloadDownload
- Share
- Language
- Discussion
- Audio Version
In this series:Plantar fasciitisAchilles tendon ruptureMetatarsalgiaMetatarsal fracturesMorton's neuromaFlat feet and fallen arches
Achilles tendinopathy is a condition that causes pain, swelling and stiffness of the Achilles tendon that joins the heel bone to the calf muscles. It is thought to be caused by repeated tiny injuries to the Achilles tendon. These may occur for a number of reasons, including overuse of the tendon - for example, in runners. Treatment includes rest, ice packs, painkillers and special exercises to help to stretch and strengthen the Achilles tendon. For most people, the symptoms of Achilles tendinopathy usually clear within 3-6 months of starting treatment.
In this article:
Video picks for Heel and foot pain
Continue reading below
What is Achilles tendinopathy?
Achilles tendinopathy is a condition that causes pain, swelling and stiffness of the Achilles tendon. It is thought to be caused by repeated tiny injuries (known as microtrauma) to the Achilles tendon. After each injury, the tendon does not heal completely, as should normally happen. This means that over time, damage to the Achilles tendon builds up and Achilles tendinopathy can develop.
What is the Achilles tendon?
Back to contentsFoot and heel pain - Achilles tendon
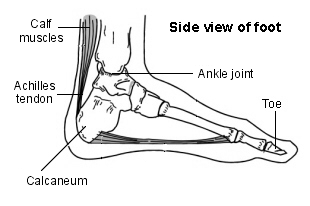
The Achilles tendon is an important part of the leg. It is found just behind and above the heel. It joins the heel bone (calcaneum) to the calf muscles. The function of the Achilles tendon is to help in bending the foot downwards at the ankle. (This movement is called plantar flexion.)
Continue reading below
Symptoms of Achilles tendinopathy
Back to contentsThe main symptoms include:
Pain and stiffness around the affected Achilles tendon.
Swelling of the ankle.
Tenderness around the tendon.
Pain and stiffness tend to develop gradually and are usually worse when first waking up in the morning. (Severe pain that comes on suddenly and difficulty walking can be symptoms of Achilles tendon tear (rupture). See a doctor urgently if you develop these symptoms.)
Some people have pain during exercise but, in general, pain is worse after exercise. Runners may notice pain at the beginning of their run, which then tends to ease and become more bearable, followed by an increase in pain when they have stopped running.
Pain due to Achilles tendinopathy may prevent people from being able to carry out their usual everyday activities such as walking to the shops, etc. People may notice that they have pain when they touch the area around the Achilles tendon. There may also be some swelling around this area.
Causes of Achilles tendinopathy
Back to contentsThere are a number of things that may lead to these repeated tiny injuries to the Achilles tendon. For example:
Overuse of the Achilles tendon. This can be a problem for people who run regularly. (Achilles tendinopathy can also be a problem for dancers and for people who play a lot of tennis or other sports activities that involve jumping.)
Training or exercising wearing inappropriate footwear.
Having poor training or exercising techniques - for example, a poor running technique.
Making a change to a training programme - for example, rapidly increasing the intensity of training and how often you train.
Training or exercising on hard or sloped surfaces.
Continue reading below
How common is Achilles tendinopathy?
Back to contentsAchilles tendinopathy affects more than 150,000 people in the UK every year. It's becoming more frequent, which is thought to be due to the increase in people engaging in sport and participating in more strenuous training. It can be a particular problem for long-distance runners but is also more prevalent in dancers and tennis players.
Risk factors
Back to contentsAchilles tendinopathy is also more common in people who have certain types of arthritis, such as ankylosing spondylitis or psoriatic arthritis. It is also thought that our genetic 'makeup' (the material inherited from our parents which controls various aspects of our body) may play a part for some people who develop Achilles tendinopathy. It is also more common in people who have high blood pressure, high cholesterol or diabetes.
People who are taking medicines from a group called fluoroquinolones (for example, the antibiotics ciprofloxacin and ofloxacin) also have an increased risk of developing Achilles tendinopathy.
Achilles tendinopathy used to be known as Achilles tendonitis. In general, 'itis' usually refers to inflammation, so tendonitis would mean inflammation of a tendon. However, Achilles tendinopathy is now thought to be a better term to use because it is thought that there is little or no inflammation that causes the problem.
If the Achilles tendon is torn, this is called an Achilles tendon rupture. See the separate leaflet called Achilles Tendon Rupture for more details.
How is Achilles tendinopathy diagnosed?
Back to contentsDoctors can usually diagnose Achilles tendinopathy because of the typical symptoms and from examining the Achilles tendon. They may feel for swelling or tenderness of the tendon. They may also ask people to do some exercises to put some stress on the Achilles tendon. For example, they may ask them to stand on the affected leg and raise the heel off the ground.
For most people with Achilles tendinopathy this movement brings on (reproduces) their pain. If this does not bring on the pain, the doctor may ask you to hop on that foot, either on the spot or in a forwards direction.
Doctors may also do some other tests to make sure that there are no signs of a torn (ruptured) Achilles tendon. For example, squeezing calf muscles and looking at how the foot moves.
Sometimes, blood tests might be offered to rule out underlying causes such as high cholesterol or diabetes.
Tests are not usually needed to diagnose Achilles tendinopathy. However, an ultrasound scan or an MRI scan may sometimes be suggested by a specialist if the diagnosis is not clear. X-rays are poor at showing signs of Achilles tendinopathy, and so are only really useful if another diagnosis (such as a fracture) is suspected.
Achilles tendinopathy treatment
Back to contentsThere are a number of treatments for Achilles tendinopathy that may help. The treatments below are usually suggested first. They are all considered as conservative treatments. This means treatments that do not involve surgery.
Rest
Rest and time off from sporting activities are important for treating Achilles tendinopathy. At first, stop any high-impact activities or sports (such as running). As pain improves, you can restart exercise as pain allows.
Complete rest, particularly if prolonged, can delay healing; so, it's a good idea to continue with exercises that are not painful, or only slightly painful.
Switching to different exercises that don't put as much strain on the Achilles tendon can be helpful to maintain overall fitness whilst recovering. Examples include cycling and deep water running.
Painkillers
Painkillers such as paracetamol or ibuprofen may help to relieve pain. Ibuprofen is from a group of medicines called non-steroidal anti-inflammatory drugs (NSAIDs). Ibuprofen, and other NSAIDs, are useful for short-term pain relief. It's thought, though, that longer-term use (more than a week) may affect the healing process. They might also cover up or mask the pain, leading people to go back to doing activities that damage the Achilles tendon. It's therefore best to limit their use to a week or two, if possible.
Note: side-effects sometimes occur with anti-inflammatory painkillers. Stomach pain, and bleeding from the stomach, are the most serious. Some people with asthma, high blood pressure, kidney failure and heart failure may not be able to take anti-inflammatory painkillers. So, check with your doctor or pharmacist before taking them if you are unsure if they are suitable for you.
Ice packs
Ice treatment may be useful for pain control and may help to reduce swelling in the early stages of Achilles tendinopathy. An ice pack should be applied for 10-30 minutes. Less than 10 minutes has little effect. More than 30 minutes may damage the skin.
Make an ice pack by wrapping ice cubes in a plastic bag or towel. (Do not put ice directly next to skin, as it may cause ice burn.) A bag of frozen peas is an alternative. Gently press the ice pack on to the injured part. The cold from the ice is thought to reduce blood flow to the damaged tendon. This may reduce pain. Do not leave ice on while asleep.
Exercises for Achilles tendinopathy
Special exercises to help to stretch and strengthen the Achilles tendon are very helpful for treating Achilles tendinopathy. Aim to do these every day. These exercises also help with pain control and stiffness.
These exercises are called eccentric exercises. Eccentric exercises focus on the lengthening part of a muscle movement.
A physiotherapist may be able to help with these exercises. They may also use other treatments such as ultrasound and massage to help relieve symptoms and promote healing of the Achilles tendon.
The following exercises can be used to help treat Achilles tendinopathy:
Stand about 40 cm away from a wall and put both hands on the wall at shoulder height, feet slightly apart, with one foot in front of the other. Bend your front knee but keep your back knee straight and lean in towards the wall to stretch your calf. You should feel your calf muscle tighten. Keep this position for several seconds, then relax. Do this about 10 times and then switch to the other leg. Now repeat the same exercise for both legs but, this time, bring your back foot forward slightly so that your back knee is also slightly bent. Lean against the wall as before, keep the position, relax and then repeat 10 times before switching to the other leg. Repeat this routine twice a day.
Stand on both feet. Use your unaffected leg to raise up on to tiptoes. Transfer your weight across to your affected leg and lower yourself down. Repeat and aim for three sets of 15 repetitions twice each day. The standing on tiptoe exercise should be performed with your knees straight and with your knees bent.
Stand on the bottom step of some stairs (facing upstairs) with your legs slightly apart and with your heels just off the end of the step. Hold the stair rail for support. Raise up on tiptoes, then, standing on the affected leg, lower your heel, keeping your knee straight. Put your good leg down before lifting your heel. Repeat and aim for three sets of 15 repetitions twice each day. Repeat but this time keeping the knee of the affected leg slightly bent. Try to do these exercises twice a day. These exercises are sometimes called Alfredson's exercises after the person who first showed that they work.
Keep a towel (or a long piece of elastic) by the side of your bed. First thing in the morning, before you get out of bed, loop the towel around the ball of one of your feet. Then pull the towel towards you, keeping your knee straight. Hold the pull for about 30 seconds. This exercise will pull your toes and the upper part of your foot towards you. Repeat this exercise three times for each foot.
Sit on a chair with your knees bent at right angles and your feet and heels flat on the floor. Lift your foot upwards, keeping your heel on the floor. Hold the position for a few seconds and then relax. Repeat about 10 times. Try to do this exercise five to six times a day.
Orthotics
An orthotics specialist may suggest changing footwear or putting special inserts in shoes, such as inserts to lift the heel. This may help to reduce pain and symptoms.
A note about steroid injections
Steroid injections are sometimes used for other tendon injuries. However, steroid injections for Achilles tendinopathy are controversial. Steroid injections have a risk of weakening the tendon further, potentially leading to it tearing (rupturing) completely. Most experts feel that the benefits of steroid injections for Achilles tendinopathy are outweighed by the risks, and that they therefore shouldn't be used.
What happens if initial treatment fails?
Back to contentsFor most people, the symptoms of Achilles tendinopathy usually clear within 3-6 months of starting conservative treatment, as described above. In general, the earlier the problem is recognised and treatment started, the better the outcome.
If the symptoms have not improved after 3-6 months, your doctor may suggest that they refer you to a specialist orthopaedic surgeon or sports medicine doctor. However, this timescale may change depending on your symptoms, your sporting activities, etc.
Specialist treatments that are not surgery
There are some treatments that some specialists may suggest to help treat Achilles tendinopathy. You should discuss these treatments fully with your specialist, including their pros and cons, before any treatment is started. These treatments may not be widely available on the National Health Service (NHS). Some may also be carried out as part of a trial to look at the best ways of treating Achilles tendinopathy. Such treatments may include:
Extracorporeal shock-wave therapy - during this treatment, special sound waves are passed through the skin to the Achilles tendon. Side-effects can include reddening of the skin and an ache in the calf after treatment. This procedure is generally safe but there is a small risk of tearing (rupturing) the Achilles tendon with this treatment, particularly in older people. At the moment, it is uncertain how effective this treatment is and how well it works. The National Institute for Health and Care Excellence (NICE) therefore recommends that specialists discuss this treatment fully with anyone before it is started. This is so that the person understands the possible small risks and that the effectiveness of this treatment is uncertain. This does not mean that the procedure should not be done; it just means that you need to discuss it fully with your specialist beforehand.
Injection using your own blood - it is possible for a specialist to take some of your own blood (in the usual way) and to inject this around your Achilles tendon. This is called autologous blood injection. A similar treatment is called platelet-rich plasma (PRP). The idea is that this will help to promote healing of the damaged tendon by encouraging the growth of cells involved in the healing process. The specialist may use an ultrasound scan to help guide their injection. These treatments are controversial; in 2013, the UK's National Institute for Health and Clinical Excellence (NICE) stated that it was unclear if these treatments were effective, or what the long-term effects are. NICE states that these treatments should only be given if patients are fully aware of the uncertainty around them, and that all other treatment options have been discussed. Note that, since 2013, more recent research studies have found little, or no, benefit from platelet-rich plasma injections (see Further Reading, below).
Surgery for Achilles tendinopathy
Around 1 in 4 people who have persisting pain due to Achilles tendinopathy have surgery to treat the condition. Most people have a good result from surgery and their pain is relieved. Surgery involves either of the following:
Removing nodules or adhesions (parts of the fibres of the tendon that have stuck together) that have developed within the damaged tendon.
Making a lengthways cut in the tendon to help to stimulate and encourage tendon healing.
Complications from surgery are not common but, if they do occur, can include problems with wound healing.
Complications of Achilles tendinopathy
Back to contentsThere is a risk of tearing (rupturing) the Achilles tendon if you have Achilles tendinopathy. This is because the tendon is damaged and weaker than usual. However, this risk is usually quite low. Severe pain around the Achilles tendon that develops suddenly may be a sign of tendon rupture. See a doctor urgently if you think that you may have ruptured your Achilles tendon.
If you do have problems with one Achilles tendon, there is also an increased chance that you will develop problems with the other over time.
Preventing Achilles tendinopathy
Back to contentsAchilles tendinopathy is a common injury, especially in people who are very physically active.
Being physically active is very good for your health. Things that help to prevent Achilles tendinopathy, particularly for people who do lots of exercise, include:
Doing warm-up and cool-down exercises, before and after exercising, including calf stretches.
Maintaining a healthy weight. Having overweight or obesity puts extra strain on the Achilles tendon.
Avoiding sudden increases in the amount or intensity of exercise you do. If you're starting a new exercise regime, build up gradually.
Wearing the right footwear. Choose shoes with good heel and arch support. Replace shoes that have worn out.
Avoiding or stopping activities that cause Achilles tendon pain; 'pushing through' usually makes it worse.
Trying to avoid changing your usual running surface; research suggests that many different types of running surface (firm, soft, and uneven) may be linked with different types of strain on the Achilles tendon, but that changing from one type to another may be particularly problematic.
Getting expert advice on exercise technique; for example, from a physiotherapist or running coach.
Patient picks for Heel and foot pain

Foot care
Morton's neuroma
Morton's neuroma is a condition that affects one of the nerves that run between the long bones (metatarsals) in the foot. The exact cause is not certain. Symptoms include pain, burning, numbness and tingling between two of the toes of the foot. About a third of cases resolve withd simple treatments including modification of footwear. Sometimes surgery is needed for long-standing (chronic) symptoms.
by Dr Philippa Vincent, MRCGP

Foot care
Flat feet and fallen arches
Flat feet are just as they sound - feet that are flatter on the undersurface (or plantar surface) than they should be, because the arches (insteps) have dropped. This can (but does not always) lead to pain and tiredness in the feet. It can also cause problems in the ankles, legs or back.
by Dr Hayley Willacy, FRCGP
Further reading and references
- Autologous blood injection for tendinopathy; NICE Interventional procedure guidance, January 2013
- Asplund CA, Best TM; Achilles tendon disorders. BMJ. 2013 Mar 12;346:f1262. doi: 10.1136/bmj.f1262.
- van der Plas A, de Jonge S, de Vos RJ, et al; A 5-year follow-up study of Alfredson's heel-drop exercise programme in chronic midportion Achilles tendinopathy. Br J Sports Med. 2012 Mar;46(3):214-8. doi: 10.1136/bjsports-2011-090035. Epub 2011 Nov 10.
- Kearney RS, Parsons N, Metcalfe D, et al; Injection therapies for Achilles tendinopathy. Cochrane Database Syst Rev. 2015 May 26;5:CD010960. doi: 10.1002/14651858.CD010960.pub2.
- Extracorporeal shockwave therapy for Achilles tendinopathy; NICE Interventional Procedure Guidance, December 2016
- Achilles tendinopathy; NICE CKS, June 2020 (UK access only)
- Aicale R, Oliviero A, Maffulli N; Management of Achilles and patellar tendinopathy: what we know, what we can do. J Foot Ankle Res. 2020 Sep 29;13(1):59. doi: 10.1186/s13047-020-00418-8.
- Kearney RS, Ji C, Warwick J, et al; Effect of Platelet-Rich Plasma Injection vs Sham Injection on Tendon Dysfunction in Patients With Chronic Midportion Achilles Tendinopathy: A Randomized Clinical Trial. JAMA. 2021 Jul 13;326(2):137-144. doi: 10.1001/jama.2021.6986.
Continue reading below
Article history
The information on this page is written and peer reviewed by qualified clinicians.
Next review due: 24 Jul 2028
26 Jul 2023 | Latest version

Ask, share, connect.
Browse discussions, ask questions, and share experiences across hundreds of health topics.

Feeling unwell?
Assess your symptoms online for free
Sign up to the Patient newsletter
Your weekly dose of clear, trustworthy health advice - written to help you feel informed, confident and in control.
By subscribing you accept our Privacy Policy. You can unsubscribe at any time. We never sell your data.