Cervical cancer
Peer reviewed by Dr Doug McKechnie, MRCGPLast updated by Dr Hayley Willacy, FRCGP Last updated 26 Mar 2023
Meets Patient’s editorial guidelines
- DownloadDownload
- Share
- Language
- Discussion
In this series:Gynaecological cancerCancer of the uterusOvarian cancerVulval cancerVulval intraepithelial neoplasiaCervical screening
If the cells that make up the cervix multiply abnormally, you develop cervical cancer (cancer of the cervix).
In this article:
Video picks for Gynaecological cancer
Continue reading below
What is cervical cancer?
What is cervical cancer?
Cervical cancer is cancer of the cervix. The cervix is the lower part of your womb (uterus) which extends slightly into the top of your vagina. The cervix is often called the neck of the womb. The surface of your cervix is covered with skin-like cells. There are also some tiny glands in the lining of the cervical canal which make mucus.
Uterus and cervix
Types of cervical cancer
Back to contentsSquamous cell cervical cancer is the most common. This develops from a skin-like cell (a squamous cell) that covers the neck of the womb (cervix), which becomes cancerous.
Adenocarcinoma cervical cancer is less common. This develops from a glandular cell (a cell that makes mucus) within the cervical canal, which becomes cancerous.
Both types are diagnosed and usually treated in a similar way.
See the separate leaflet called Cancer for more information about cancer in general.
Continue reading below
Cervical cancer symptoms
Back to contentsYou may have no cervical cancer signs at first, when the tumour is small. As the tumour becomes larger, symptoms include:
Bleeding between normal periods (intermenstrual bleeding).
Bleeding after having sex (postcoital bleeding).
Any vaginal bleeding in women past the menopause.
A vaginal discharge that smells unpleasant.
Discomfort or pain during sex.
All the above symptoms can be caused by various other common conditions. But if you develop any of these symptoms, you should see a doctor.
In time, if the cancer spreads to other parts of the body, various other symptoms can develop.
How common is cervical cancer?
Back to contentsMost cases develop in women aged between 25 and 45. Some cases develop in older and younger women. It is rare in women aged under 25 years.
Cervical cancer is the fourteenth most common type of cancer in women in the UK. The number of cases diagnosed each year has mostly fallen over recent years. This is because cervical cancer can be prevented by regular cervical screening tests. In less developed parts of the world, cervical cancer is the second or third most common type of cancer in women.
Continue reading below
What causes cervical cancer?
Back to contentsA cancerous tumour starts from one cell. It is thought that something damages or alters certain genes in the cell. This makes the cell very abnormal and multiply out of control. See the separate leaflet called Causes of Cancer for more details.
In the case of cervical cancer, the cancer develops from a cell which is already abnormal - see above. In most cases, abnormal cells are present for years before one of the abnormal cells becomes cancerous and starts to multiply out of control into a cancerous tumour.
The initial pre-cancerous abnormality of cervical cells is usually caused by a prior infection with the human papillomavirus (HPV). This virus is found in more than 99 out of 100 women with cervical cancer.
HPV and cervical cancer
There are many strains of HPV. Two types, HPV 16 and 18, are involved in the development of most cases of cervical cancer. (Note: some other strains of HPV cause common warts and verrucas. These strains of HPV are not associated with cervical cancer.)
The strains of HPV associated with cervical cancer are nearly always passed on by having sex with an infected person. An infection with one of these strains of HPV does not usually cause symptoms.
So, you cannot tell if you or the person you have sex with are infected with one of these strains of HPV. The more sexual partners you have, the higher your chances of becoming infected with HPV, and therefore the higher the risk of cervical cancer.
In some women, the strains of HPV that are associated with cervical cancer affect the cells of the neck of the womb (cervix). This makes them more likely to become abnormal which may later (usually years later) turn into cancerous cells.
Note: within two years, 9 out of 10 infections with HPV will clear completely from the body. This means that most women who are infected with these strains of HPV do not develop cancer.
The HPV vaccine has been introduced for girls from the age of 12 years in the UK. Studies have shown that the HPV vaccine is very effective at stopping cancer of the cervix from developing.
The vaccine has been shown to work better for people who are given the vaccine when they are younger, before they are sexually active, compared to when it is given to adults. However, even if you have had the HPV vaccine, you must attend for cervical screening. This is because the vaccine does not guarantee complete protection against cervical cancer.
See the separate leaflet called Human Papillomavirus Immunisation (HPV) for more details.
Other factors
Other factors that increase the risk of developing cervical cancer include the following:
Smoking. Chemicals from cigarettes are carried in the bloodstream and can affect cells in the body. Smokers are 2 x more likely than non-smokers to develop cervical cancer. In particular, if you smoke and have HPV infection, the risk is greater.
A poor immune system. For example, people with AIDS or people taking immunosuppressant medication have an increased risk. (If your immune system is not working fully then you are less able to deal with HPV infection and abnormal cells and you are more at risk of developing cervical cancer.)
There is a possible link between the combined oral contraceptive (COC) pill - also known as 'the pill' - and a slightly increased risk of cervical cancer if the pill is taken for more than five years.
Cervical cancer diagnosis
Back to contentsConfirming the diagnosis
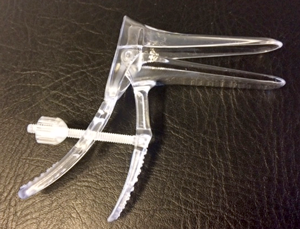
A doctor will usually do a vaginal examination if you have symptoms which may possibly be cervical cancer. He or she may feel an abnormal neck of the womb (cervix). Your doctor is also likely to perform a speculum examination, which is the same instrument used when you have a smear test taken. See the separate leaflet called Cervical Screening (Cervical Smear Test).
A speculum
Editor’s note
Dr Krishna Vakharia, 16th October 2023
The National Institute for Health and Care Excellence (NICE) has recommended that a person should receive a diagnosis or ruling out of cancer within 28 days of being referred urgently by their GP for suspected cancer.
Colposcopy
If cervical cancer is suspected, you will usually be referred for colposcopy. This is a procedure which allows a more detailed examination of the cervix. For this test, a speculum is gently put into the vagina so the cervix can be seen. The doctor uses a magnifier (colposcope) to look at the cervix in more detail. The test takes about 15 minutes. During colposcopy it is usual to take a small piece of tissue (biopsy) from the cervix. The biopsy sample is then examined under a microscope to look for cancer cells. See the separate leaflet called Colposcopy and Cervical Treatments.
Cervical cancer stages
Back to contentsAssessing the extent and spread
If you are found to have cervical cancer then further tests may be advised to assess if the cancer has spread. For example, a computerised tomography (CT) scan, a magnetic resonance imaging (MRI) scan, a chest X-ray, an ultrasound scan, blood tests or other tests. This assessment is called staging of the cancer. The aim of staging is to find out:
How much the tumour has grown and whether it has grown into other nearby structures such as the bladder or back passage (rectum).
Whether the cancer has spread to local lymph glands (nodes).
Whether the cancer has spread to other areas of the body (metastasised).
Exactly what tests are needed depends on the initial assessment and the results of the biopsy. For example, the biopsy may show that the cancer is at a very early stage and remains just in the surface cells of the cervix.
This is unlikely to have spread and you may not need many other tests. However, if the cancer appears to be more advanced and likely to have spread then a range of tests may be needed.
Finding out the stage of the cancer helps doctors to advise on the best treatment options. It also gives a reasonable indication of outlook (prognosis). See the separate leaflet called Stages of Cancer for details.
The staging system of the International Federation of Gynecology and Obstetrics (FIGO) is most commonly used for staging cervical cancer. This classification is based on tumour size, whether there is spread into the vagina or surrounding tissues, or spread into the bladder or rectum and whether there are distant metastases.
Stage 0: no evidence of primary tumour.
Stage I: cervical cancer is confined to the uterus.
Stage II: the tumour has invaded beyond the uterus but not into the pelvic wall or the lower part of the vagina.
Stage III: the tumour extends into the pelvic wall and/or involves the lower third of the vagina and/or causes swelling of the kidney (hydronephrosis), or the kidney not to function.
Stage IV: further spread beyond the pelvis.
The vast majority of women are diagnosed with early-stage cancers.
Aims of treatment
Back to contentsYou should also discuss with your specialist the aims of treatment. For example:
Curing cervical cancer
In some cases, treatment aims to cure the cancer. Some cervical cancers can be cured, particularly if they are treated in the early stages of the disease. (Doctors tend to use the word remission rather than the word cured.)
Remission means there is no evidence of cancer following treatment. If you are in remission, you may be cured. However, in some cases, a cancer returns months or years later.
Controlling cervical cancer
In some cases, treatment aims to control the cancer. If a cure is not realistic, with treatment it is often possible to limit the growth or spread of the cancer so that it progresses less rapidly. This may keep you free of symptoms for some time.
Easing the symptoms
In some cases, treatment aims to ease symptoms. For example, if a cancer is advanced then you may require treatments such as painkillers or other treatments to help keep you free of pain or other symptoms. Some treatments may be used to reduce the size of a cancer, which may ease symptoms such as pain.
Cervical cancer treatment
Back to contentsWhat does the cervical cancer jab do?
The cervical cancer treatment advised for each case depends on various factors. For example, the stage of the cancer (how large the first (primary) cancer tumour is and whether it has spread), your general health and also if you are planning on having children.
You should have a full discussion with a specialist who knows your case. They will be able to give information on:
The pros and cons.
Likely success rate.
Details of possible side-effects.
The various possible treatment options for your type and stage of cancer.
Cervical cancer treatments include:
Hysterectomy
An operation (called a hysterectomy) to remove the neck of the womb (cervix) and the womb (uterus) is a common treatment. If the cancer is at an early stage and has not spread then surgery alone can be curative.
In some cases, in very early-stage cancer, it may be possible just to remove the part of the cervix affected by the cancer without removing the entire uterus. This would mean that you could still have the chance to try to have your own children.
Other surgery
If the cancer has spread to other parts of the body, surgery may still be advised, often in addition to other treatments. For example, in some cases where the cancer has spread to other nearby structures, extensive surgery may be an option.
This may be to remove not only the cervix and uterus but also nearby structures which may have become affected, such as the bladder and/or bowel.
Even if the cancer is advanced and a cure is not possible, some surgical techniques may still have a place to ease symptoms. For example, to relieve a blockage of the bowel or urinary tract which has been caused by the spread of the cancer.
Radiotherapy
Radiotherapy is a treatment which uses high-energy beams of radiation which are focused on cancerous tissue. This kills cancer cells or stops cancer cells from multiplying. See the separate leaflet called Radiotherapy for more details.
Radiotherapy alone can cure early-stage cervical cancer and may be an alternative to surgery. For more advanced cancers, radiotherapy may be advised in addition to other treatments.
Two types of radiotherapy are used for cervical cancer - external and internal. In many cases both types are used:
External radiotherapy. Radiation is targeted on the cancer from a machine. (This is the common type of radiotherapy used for many types of cancer.)
Internal radiotherapy (brachytherapy). This treatment involves placing a small radioactive implant next to the cancerous tumour (in the vagina) for a short time.
Even if the cancer is advanced and a cure is not possible, radiotherapy may still have a place to ease symptoms. For example, radiotherapy may be used to shrink secondary tumours which have developed in other parts of the body and are causing pain.
Chemotherapy
This is a treatment using anti-cancer medicines which kill cancer cells or stop them from multiplying. Chemotherapy may be given in addition to radiotherapy or surgery in certain situations.
Cervical cancer and pregnancy
Back to contentsIf you are diagnosed with cervical cancer when you are pregnant, what will happen depends on several factors:
What type of cancer you have.
How big the tumour is and whether it has spread.
How many weeks pregnant you are.
What you want to happen.
Treatment for the cancer may be delayed until the baby is able to survive out of the womb, so it can be delivered (provided this delay is only for a few weeks). If this will take too long, or the tumour is large, a therapeutic abortion may be advised.
If you are more than three months pregnant when your cancer is diagnosed, your consultant may advise you can continue with the pregnancy, but you should have a caesarean section for delivery. The surgical team may also perform a hysterectomy after delivery and you will likely receive further treatment with chemotherapy and radiotherapy.
If you are less than three months pregnant your consultant may want to treat you straightaway. Leaving cervical cancer without treatment for six months is risky. They may advise having an abortion. If you want to carry on with your pregnancy, it may be possible to have some chemotherapy after the first 13 weeks have passed. Those first weeks are very important for the developing baby and chemotherapy may affect the baby or cause a miscarriage. Treating cancer whilst you are still pregnant is still experimental and there are no large experimental data to show outcomes yet. You should be able to have an honest discussion with your consultant about your treatment options, based on your cancer stage and the stage of your pregnancy.
As cervical cancer often affects women of childbearing age, fertility-sparing surgery is also an important issue when considering treatment options.
What's the outlook?
Back to contentsThe outlook (prognosis) is best in those who are diagnosed when the cancer is confined to the neck of the womb (cervix) and has not spread. Treatment in this situation gives a good chance of cure for at least 8-9 women out of 10. For women who are diagnosed when the cancer has already spread, a cure is less likely but still possible.
Even if a cure is not possible, treatment can often slow down the progression of the cancer. Prognosis is generally very good in women diagnosed at a young age. 9 in 10 women under the age of 40 survive for at least five years after diagnosis, compared to about a quarter of women aged 80 or more.
The treatment of cancer is a developing area of medicine. New treatments continue to be developed and the information on outlook above is very general.
The specialist who knows your case can give more accurate information about your particular outlook and how well your type and stage of cancer are likely to respond to treatment.
Can cervical cancer be prevented?
Back to contentsMany cases of cancer of the cervix are already prevented through the cervical screening programme. In this programme, women in the at-risk age category have regular smear tests. This test looks for early changes in cells, which could turn into cancer.
If early changes seem to be progressing towards cancer, you can have treatment to stop you developing cervical cancer. See the separate leaflet called Cervical Screening (Cervical Smear Test).
As above, it is also hoped that the HPV immunisation programme will prevent many cases of cervical cancer.
Patient picks for Gynaecological cancer

Cancer
Gynaecological cancer
A number of cancers can arise in the female reproductive organs. This leaflet explains where these organs are and links to information about the individual cancers.
by Dr Philippa Vincent, MRCGP

Cancer
Ovarian cancer
Ovarian cancer is the sixth most common cancer in women in the UK. It is more common than cancer of the neck of the womb (cervical cancer).
by Dr Hayley Willacy, FRCGP
Further reading and references
- Suspected cancer: recognition and referral; NICE guideline (2015 - last updated May 2025)
- Marth C, Landoni F, Mahner S, et al; Cervical cancer: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol. 2017 Jul 1;28(suppl_4):iv72-iv83. doi: 10.1093/annonc/mdx220.
- Cervical cancer; Survival by stage, Cancer Research UK.
- Fowler JR, Maani EV, Jack BW; Cervical Cancer
- Cervical cancer - Risks; Cancer Research UK.
- CKS Cervical cancer and HPV; NICE CKS, February 2022 (UK access only)
Continue reading below
Article history
The information on this page is written and peer reviewed by qualified clinicians.
Next review due: 7 Feb 2028
26 Mar 2023 | Latest version

Ask, share, connect.
Browse discussions, ask questions, and share experiences across hundreds of health topics.

Feeling unwell?
Assess your symptoms online for free
Sign up to the Patient newsletter
Your weekly dose of clear, trustworthy health advice - written to help you feel informed, confident and in control.
By subscribing you accept our Privacy Policy. You can unsubscribe at any time. We never sell your data.