
Are we prepared to fight flu and COVID-19 this winter?
Peer reviewed by Dr Sarah Jarvis MBE, FRCGPLast updated by Andrea DowneyLast updated 18 Oct 2021
Meets Patient’s editorial guidelines
- DownloadDownload
- Share
- Language
- Discussion
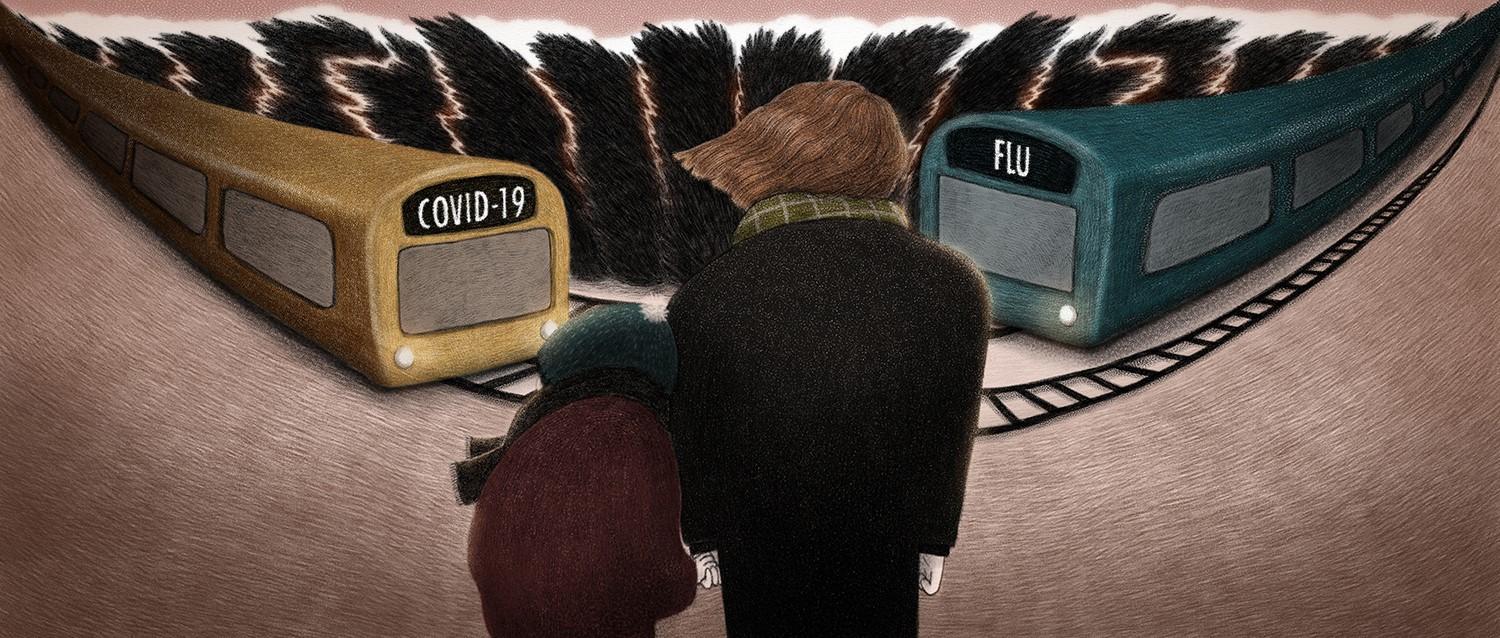
This winter is likely to be unlike one we've seen before. With COVID-19 and flu set to be circulating as the weather gets colder, there's an increased risk from both infections. A big spike in either of the viruses will put extra strain on the NHS, which is already struggling to recover from the impact of the pandemic so far.
In this article:
So how prepared are we to fight flu and COVID-19 this winter? And what measures can you take to protect yourself, your loved ones and the NHS?
Professor Martin Michaelis, virologist and professor of molecular medicine at the University of Kent, and Dr Alisha Damani, founder of The Medic Today, explain more.
Continue reading below
Be prepared
Even without COVID-19, the NHS is used to being under significant pressure every winter. But with the pandemic thrown into the mix, it could mean this winter is worse than usual, Prof Michaelis says.
"Last winter, lockdowns and other COVID-19 restrictions did not only inhibit the spread of COVID-19 but also that of other respiratory viruses and other pathogens that we typically see in the winter," he explains.
"In the absence of comparable measures, we will probably see a resurgence of many pathogens including influenza viruses (which cause the flu), common cold viruses, respiratory syncytial virus (RSV, which causes severe issues in children and older adults), and norovirus (known as winter vomiting bug)."
On top of that, we don't know how severe the common winter bugs will be because our bodies haven't had to fight them off for a while.
"Notably, we do not know what the gap year may mean for all the non-COVID-19 pathogens that hardly circulated last winter. There is concern that the lack of exposure may have resulted in reduced immunity and, hence, higher vulnerability in parts of the population," Prof Michaelis adds.
Dr Damani agrees, adding that bed occupancy in the NHS is already struggling in some areas.
"With the economy open and NHS services resumed, COVID-19 transmission rates are increasing. We are seeing an increase in hospitalisations with positive COVID-19 diagnoses, and the bed occupancy rates are already much higher than usual," she says.
"Resources are limited and this will impact how the NHS will be able to manage. This includes staff shortages from self-isolation, ill health, burn-out and fatigue.
"We have seen the impact of the pandemic with regard to delayed diagnoses and treatment, causing further ill health alongside increased acute illnesses, particularly from respiratory conditions. Recent modelling suggests that influenza and RSV [respiratory syncytial virus] hospitalisations and deaths could be twice what was previously anticipated."
Prof Michaelis warns that these two circumstances mean "we will have a tough winter that pushes the NHS to its limits again and occasionally beyond them".
Get the jab
Currently, the best protection against the flu and COVID-19 is the vaccination programme.
The COVID-19 vaccination programme has been hugely successful, and the government has recently expanded its free flu vaccination programme to more people, including those over 50.
Vaccines offer the best protection from viruses and therefore help stop their spread.
"Flu vaccines will be provided for free to schoolchildren and everyone over the age of 50. Moreover, COVID-19 booster jabs will be rolled out to many vulnerable groups, and the 12- to 15-year-olds will be offered COVID-19 vaccines," Prof Michaelis explains.
"This should reduce the impact of the flu and COVID-19 but will not cover other pathogens such as common cold viruses, RSV and norovirus that are also known to cause significant trouble in the winter.
"The level of protection these vaccines will provide to the health service will critically depend on the uptake."
The impact flu vaccines is likely to have also relies heavily on information about previous flu viruses that circulate. Every year the World Health Organization predicts the most common strain of flu based on last winter's most common strains, but due to last winter's lockdown, not a single case of flu was recorded by Public Health England.
"The efficacy of flu vaccines will also depend on which influenza viruses will circulate and how accurate the predictions have been. If the vaccines do not match the predominant influenza viruses, the protection will be limited," Prof Michaelis adds.
Then there's the issue of new COVID variants. As new variants emerge, the impact of the vaccines has the potential to change, Prof Michaelis explains.
"So far, the current COVID-19 vaccines seem to provide good protection against all circulating variants. However, if a new variant emerges that can (partially) bypass immunity provided by COVID-19 vaccines or previous COVID-19 infections, the situation may quickly become critical," he says.
Continue reading below
Plan B
Like all good plans, there needs to be a backup in case is fails. In this case, that will mean extra measures put in place to protect us from the spread of COVID-19.
"Currently, the main strategy is to vaccinate against COVID-19 and the flu. Moreover, the 'Test, Trace and Isolate system' will remain in place. If this is not enough and the NHS is in acute danger of becoming overwhelmed, the so-called 'Plan B' will come into action," Prof Michaelis explains.
"This will include measures such as warning of increased risk, mandatory face masks in places at high risk of virus transmission, working from home, and mandatory vaccine certificates for high-risk venues such as nightclubs. However, if this is not enough more drastic restrictions are likely."
So what does this mean for preventing big waves of illness?
Currently, modelling from the Scientific Advisory Group for Emergencies (SAGE) suggests that we may see 2,000 to 7,000 COVID-19 hospitalisations per day from October.
Last winter, the number of daily COVID-19 hospitalisations peaked at about 4,500.
If that prediction is right, the NHS will probably be able to cope if the number of COVID-19 cases remains at the lower end of these projections. But if daily hospitalisations reach the upper end of the model predictions, 7,000 hospitalisations a day, the NHS would be overwhelmed.
Prof Michaelis suggests this would probably result in a temporary collapse of our healthcare system.
It's also important to note that these predictions only include COVID-19 cases. It's currently hard to predict how bad the flu season is likely to be due to the previously mentioned lack of data and exposure.
A recent report from the Academy of Medical Sciences found the combination of COVID-19, flu and other respiratoryconditions could push the NHS to breaking point this winter.
The report, commissioned by government chief scientific advisor Sir Patrick Vallance, predicts a potential surge in respiratory viruses that could be "two times that of a 'normal year'.
"Dealing with the current third wave of COVID-19, as well as multiple subsequent outbreaks, between summer 2021 and spring 2022, means the NHS cannot catch up with the backlog of routine care," the report found.
Between 15,000 and 60,000 people could die from influenza this winter, according to new modelling for the report, although the government's flu vaccination programme should help to reduce this risk.
What all this means is that it's vital you get your flu vaccine, and COVID vaccine, as soon as you're eligible.
Best and worst
As gloomy as it sounds, it's important we all understand the best-case and the worst-case scenarios for this winter.
Let's save the best news for last and take a look at the worst-case scenario first.
"Currently, we are seeing the hospitalisation rate increase whilst the death rate remains relatively low. The modelling predicts another peak in death rate based on the following assumptions: a more limited impact of vaccines on transmission (as we have seen with the Delta variant), the possibility of new variants emerging, the rate at which vaccines can wear off and a reduced uptake of the booster vaccine," Dr Damani says.
"The government would need to consider additional measures including another lockdown if our hospitalisation and death rates increase."
It's a sentiment echoed by Prof Michaelis.
"In the worst case, we would end up in a lockdown like last winter and experience another large death toll," he says.
And now for the better news. It could be a bumpy ride this winter but the NHS will be able to cope, just.
"In the best case, we will probably still have a bumpy ride during which the NHS will come under substantial strain, and we still see a substantial number of deaths. However, we will avoid severe legal restrictions," Prof Michaelis says.
Dr Damani adds: "The best-case scenario is that the economy remains open and, even with COVID-19 in transmission, our hospitalisation and death rates remain low.
"This would be based on appropriate government guidance and public responsibility, taking reasonable measures to reduce the risk of transmission."
Continue reading below
Do your bit
A lot of things are out of our control when it comes to planning for pressures on the NHS, but there are a few things you can do to prevent the spread of COVID-19 and flu - and also other winter bugs.
First of all, as already mentioned, get your vaccine. The government has expanded its flu vaccine programme and you can use the Patient Access flu eligibility checker to see if you're eligible. Vaccines are available from GP practices and community pharmacists. It's also really important to get your COVID-19 jab if you're eligible, as it's our best protection from the virus and further lockdown restrictions.
If you're in an eligible group (which includes all over-50s, anyone classed as clinically vulnerable or clinically extremely vulnerable, health and social care workers and anyone living with someone whose immune system is severely compromised), you'll also be offered a COVID-19 booster vaccine. You'll be invited for this shortly after the six month mark since your second vaccine.
"Living with COVID-19 is now a balance we must strive to reach - minimising the impact it has on our lives, whilst maximising our protection from the virus," Dr Damani explains.
"We have to work together as families, as communities and as an entire population to ensure that we play our part in reducing the risk of transmission. The economy is open which will inevitably bring some risk of infection transmission. We can keep this risk to a minimum by ensuring we follow government guidelines as they are updated.
"The best way to reduce your risk of illness is to ensure you are wearing a mask in public areas, and maintain social distancing and good hand hygiene. If everybody plays their part in these measures, we will significantly reduce the risk of transmission of infection."
It's also important to regularly test for COVID-19 and continue to self-isolate if you have symptoms. Lateral flow tests can be ordered for free from the government, as can PCR tests for those who have symptoms or have been told they need a test.
People who are double-jabbed no longer need to self-isolate if they're told they've come into contact with someone who has tested positive, but they will need to take a PCR test.
Everyone who shows symptoms must self-isolate.
Patient picks for General information
COVID-19
What happens if you catch flu and COVID-19 at the same time?
Thousands of people across the UK are living with tougher COVID-19 restrictions in a bid to curb infection rates ahead of winter. But each year winter also means a spike in flu cases, so what happens if you catch the flu and COVID-19 at the same time?
by Andrea Downey

COVID-19
COVID-19 - coping with loneliness this Christmas
Christmas can be a difficult time. Although many of us see the holiday season as a time to spend with family and friends, it can also exacerbate feelings of loneliness. Not only are we reminded of the loss of loved ones, the pressure to be festive can be overwhelming.
by Lydia Smith
Continue reading below
Article history
The information on this page is peer reviewed by qualified clinicians.
18 Oct 2021 | Latest version

Ask, share, connect.
Browse discussions, ask questions, and share experiences across hundreds of health topics.

Feeling unwell?
Assess your symptoms online for free
Sign up to the Patient newsletter
Your weekly dose of clear, trustworthy health advice - written to help you feel informed, confident and in control.
By subscribing you accept our Privacy Policy. You can unsubscribe at any time. We never sell your data.