Achilles tendon rupture
Peer reviewed by Dr Hayley Willacy, FRCGP Last updated by Dr Doug McKechnie, MRCGPLast updated 31 Jul 2023
Meets Patient’s editorial guidelines
- DownloadDownload
- Share
- Language
- Discussion
In this series:Plantar fasciitisAchilles tendinopathyMetatarsalgiaMetatarsal fracturesMorton's neuromaFlat feet and fallen arches
The Achilles tendon is at the back of the heel. It can be ruptured by sudden force on the foot or ankle. If your Achilles tendon is ruptured you will be unable to stand on tiptoe and will have a flat-footed walk. It is important to diagnose and treat this injury as soon as possible, to help promote healing. Treatment involves wearing a plaster cast or brace (orthosis) for several weeks, and possibly having an operation.
In this article:
Video picks for Heel and foot pain
Continue reading below
What is an Achilles tendon rupture?
Foot and heel pain - Achilles tendon
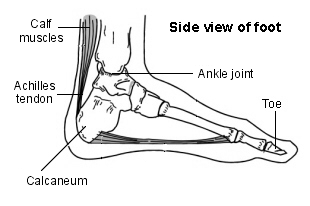
If the Achilles tendon is torn, this is called an Achilles tendon rupture. The tear may be either partial or complete. In a partial tear, the tendon is partly torn but still joined to the calf muscle. With complete tears, the tendon is completely torn so that the connection between the calf muscles and the ankle bone is lost.
The Achilles tendon is an important part of the leg. It is located just behind and above the heel. It connects the calf muscle to the heel bone. Its function is to help in bending the foot downwards at the ankle (this movement is called plantar flexion).
Causes of an Achilles tendon rupture
Back to contentsAs with any muscle or tendon in the body, the Achilles tendon can be torn if there is a high force or stress on it. This can happen with activities which involve a forceful push off with the foot - for example, in football, running, jumping, basketball, diving and tennis. The push off movement uses a strong contraction of the calf muscles which can stress the Achilles tendon too much.
The Achilles tendon can also be damaged by injuries such as falls, if the foot is suddenly forced into an upward-pointing position - this movement stretches the tendon. Another possible injury is a deep cut at the back of the ankle, which might go into the tendon.
Sometimes the Achilles tendon is weak, making it more prone to rupture. Factors that weaken the Achilles tendon are:
Corticosteroid medication (such as prednisolone) - mainly if it is used as long-term treatment rather than a short course.
Corticosteroid injection near the Achilles tendon.
Certain rare medical conditions, such as Cushing's syndrome, where the body makes too much of its own corticosteroid hormones. See the separate leaflet called Cushing's Syndrome for more information.
Tendinopathy of the Achilles tendon. See the separate leaflet called Achilles Tendinopathy for more information.
Other medical conditions which can make the tendon more prone to rupture; for example, rheumatoid arthritis, gout and systemic lupus erythematosus.
Certain antibiotic medicines may slightly increase the risk of having an Achilles tendon rupture. These are the quinolone antibiotics such as ciprofloxacin and ofloxacin. The risk of having an Achilles tendon rupture with these antibiotics is still low and mainly applies if you are also taking corticosteroid medication.
Continue reading below
How common is an Achilles tendon rupture?
Back to contentsIt affects about 4,500 people a year in the UK, It seem to be becoming more frequent due to more people taking up sport and training more intensely. It can occur at any age but is most common in people between the ages of 30 and 50.
Achilles tendon rupture symptoms
Back to contentsCommon symptoms of an Achilles tendon rupture include:
Hearing a snapping sound and feeling a sharp pain when the tendon is torn (ruptured).
Some people describe this as feeling as if they have been kicked in the back of the ankle.
Aching at the back of the lower leg.
Swelling and bruising on your lower leg.
A flat-footed type of walk. You can walk and bear weight but cannot push off the ground properly on the side where the tendon is ruptured.
Inability to stand on tiptoe.
If the tendon is completely torn, you may feel a gap just above the back of the heel. However, if there is bruising then the swelling may disguise the gap.
If you suspect an Achilles tendon rupture, see a doctor urgently because the tendon heals better if treated sooner rather than later.
Continue reading below
How is an Achilles tendon rupture diagnosed?
Back to contentsThe Achilles tendon tear (rupture) diagnosis is usually made on the basis of symptoms, the history of the injury and a doctor's examination.
The doctor may look at your walking and observe whether you can stand on tiptoe. They may test the tendon using a method called Simmonds-Thompson's test (also known as the calf squeeze test). In this test, you will be asked to lie face down on the examination bench and to bend your knee.
The doctor will gently squeeze the calf muscles at the back of your leg and observe how the ankle moves. If the Achilles tendon is OK, the calf squeeze will make the foot point away from the leg (a movement called plantar flexion). If the tendon is torn, the foot won't move. This is quite an accurate test for Achilles tendon rupture.
If the diagnosis is uncertain, an ultrasound scan or MRI scan may help.
Note: an Achilles tendon rupture is sometimes difficult to diagnose and can be missed on first assessment. It is important for doctors and patients to be aware of this and to look carefully for an Achilles tendon rupture if it is suspected.
What else could it be?
Back to contentsSimilar symptoms can be caused by:
Overuse of the Achilles tendon (Achilles tendinopathy). See the separate leaflet called Achilles Tendinopathy for more information.
A strain or tear of the calf muscles.
A blood clot (thrombosis) of a deep vein in the calf. See the separate leaflet called Deep Vein Thrombosis for more information.
Achilles tendon rupture treatment
Back to contentsThis condition should be diagnosed and treated as soon as possible because prompt treatment probably improves recovery. You may need to be referred urgently to see a doctor in an orthopaedic department or A&E department. Meanwhile, if a torn (ruptured) Achilles tendon is suspected, you should not put any weight on that foot, so do not walk on it at all. There are two options for treatment.
Surgery
The surgeon sews together the torn ends of the Achilles tendon, and perhaps may also use another tendon or a tendon graft to help with the repair. A plaster cast or brace (orthosis) is needed after the operation. The surgery can be done with a single, larger cut ('open' surgery), or, sometimes, with several small cuts and a tiny camera (called 'minimally invasive' surgery).
Brace or plaster cast
The other option is to allow time for the tendon to heal naturally, resting it in a brace or plaster cast. This is called conservative treatment. If the tendon does not heal on its own, a surgical repair can then be done later.
Both options will involve having a plaster cast or a brace for about eight weeks, to protect the tendon while it heals. The plaster cast or the brace is positioned so that the foot is pointing slightly downwards, which takes the strain off the tendon.
Traditionally, crutches were used to keep weight off the leg during the first few weeks of treatment. Now there is a trend towards using the leg normally early on (early mobilisation and weight bearing). This involves fitting a plaster cast or a brace which you can walk on. It is more convenient because you do not need to use crutches.
Physiotherapy will usually be provided as well to strengthen or stretch your calf muscles.
Which treatment is best?
Back to contentsThere is debate as to which treatment is best: surgery or conservative treatment. This section summarises the research into treatment of Achilles tendon rupture.
Most of the research so far found that surgery has one advantage: it reduces the risk that the Achilles tendon will rupture again later (a problem known as re-rupture). The disadvantages of surgery are the risk of complications such as wound infection (see below), and the need for an operation.
For this reason, surgery may be recommended for younger people or those doing sports. Conservative treatment may be suggested for older or less active people and for people wishing to avoid surgery. The choice of treatment depends on individual preference and circumstances. Surgery may also be recommended if there has been a delay in starting treatment.
However, a new piece of research found that surgery and conservative treatment actually gave equally good results, when patients were also given early mobilisation treatment using a brace.
If an operation is needed, there is a type of surgery called percutaneous, which uses smaller cuts than the traditional operation. This seems to reduce the risk of developing a wound infection.
After surgery, a brace seems to be better than a plaster cast in terms of faster recovery and return to normal activities, a lower complication rate and patients preferring it.
Achilles tendon rupture recovery
Back to contentsDepending on the type of work, some people need several weeks off work after an Achilles tendon tear (rupture); the time taken to return to sport is between 4 and 12 months.
Generally, the outlook is good. However, the tendon does take time to heal, usually about six to eight weeks. More time will be needed after this to allow the muscles to regain their normal strength after being in a plaster cast or a brace (orthosis).
Complications
Back to contentsPossible complications during recovery include:
Whichever treatment option is used, there is a chance that the Achilles tendon will not heal fully and further treatment such as surgery may be needed.
Complications of surgery: these are usually minor complications such as a wound infection or reduced sensation near the operation site. About 4 in 100 people develop a wound infection following surgery to fix a ruptured Achilles tendon.
The tendon may scar or may become shorter during the healing process.
There is also a chance that the tendon could become torn again later (re-rupture). According to some research, the risk of a re-rupture is about 4 in 100 with surgical treatment and about 12 in 100 with conservative treatment.
A clot can form in the blood vessels in the leg and this is more common after an Achilles tendon rupture.
Can an Achilles tendon rupture be prevented?
Back to contentsNot always. However, here are some suggestions to help to prevent this injury:
Corticosteroid medication such as prednisolone should be used carefully and the dose should be reduced if possible. But note that there are many conditions where corticosteroid medication is important or life-saving.
Quinolone antibiotics should be used carefully in people aged over 60 or in those taking steroids.
There are also some general measures to help prevent Achilles problems, which may help:
Doing warm-up and cool-down exercises, before and after exercising, including calf stretches.
Maintaining a healthy weight. Having overweight or obesity puts extra strain on the Achilles tendon.
Avoiding sudden increases in the amount or intensity of exercise you do. If you're starting a new exercise regime, build up gradually.
Wearing the right footwear. Choose shoes with good heel and arch support. Replace shoes that have worn out.
Avoiding or stopping activities that cause Achilles tendon pain; 'pushing through' usually makes it worse.
Trying to avoid changing your usual running surface; research suggests that many different types of running surface (firm, soft, and uneven) may be linked with different types of strain on the Achilles tendon, but that changing from one type to another may be particularly problematic.
Getting expert advice on exercise technique; for example, from a physiotherapist or running coach.
Maintaining a healthy weight. Having overweight or obesity puts extra strain on the Achilles tendon.
Avoiding sudden increases in the amount or intensity of exercise you do. If you're starting a new exercise regime, build up gradually.
Wearing the right footwear. Choose shoes with good heel and arch support. Replace shoes that have worn out.
Avoiding or stopping activities that cause Achilles tendon pain; 'pushing through' usually makes it worse.
Trying to avoid changing your usual running surface; research suggests that many different types of running surface (firm, soft, and uneven) may be linked with different types of strain on the Achilles tendon, but that changing from one type to another may be particularly problematic.
Getting expert advice on exercise technique; for example, from a physiotherapist or running coach.
Patient picks for Heel and foot pain

Foot care
Plantar fasciitis
Heel and foot pain are very common. A common cause is plantar fasciitis which causes pain under the heel. It usually goes away with time but various treatments may help.
by Dr Surangi Mendis, MRCGP

Foot care
Achilles tendinopathy
Achilles tendinopathy is a condition that causes pain, swelling and stiffness of the Achilles tendon that joins the heel bone to the calf muscles. It is thought to be caused by repeated tiny injuries to the Achilles tendon. These may occur for a number of reasons, including overuse of the tendon - for example, in runners. Treatment includes rest, ice packs, painkillers and special exercises to help to stretch and strengthen the Achilles tendon. For most people, the symptoms of Achilles tendinopathy usually clear within 3-6 months of starting treatment.
by Dr Doug McKechnie, MRCGP
Further reading and references
- Sode J, Obel N, Hallas J, et al; Use of fluroquinolone and risk of Achilles tendon rupture: a population-based cohort study. Eur J Clin Pharmacol. 2007 May;63(5):499-503. Epub 2007 Mar 3.
- Achilles tendinopathy; NICE CKS, June 2020 (UK access only)
- Costa ML, Achten J, Wagland S, et al; Plaster cast versus functional bracing for Achilles tendon rupture: the UKSTAR RCT. Health Technol Assess. 2020 Feb;24(8):1-86. doi: 10.3310/hta24080.
- Mundi R, Madden K, Bhandari M; Cochrane in CORR(R): Surgical interventions for treating acute Achilles tendon ruptures (Review). Clin Orthop Relat Res. 2014 Jun;472(6):1703-8. doi: 10.1007/s11999-013-3350-7. Epub 2013 Oct 25.
- Westin O, Sjogren T, Svedman S, et al; Treatment of acute Achilles tendon rupture - a multicentre, non-inferiority analysis. BMC Musculoskelet Disord. 2020 Jun 8;21(1):358. doi: 10.1186/s12891-020-03320-3.
Continue reading below
Article history
The information on this page is written and peer reviewed by qualified clinicians.
Next review due: 29 Jul 2028
31 Jul 2023 | Latest version

Ask, share, connect.
Browse discussions, ask questions, and share experiences across hundreds of health topics.

Feeling unwell?
Assess your symptoms online for free
Sign up to the Patient newsletter
Your weekly dose of clear, trustworthy health advice - written to help you feel informed, confident and in control.
By subscribing you accept our Privacy Policy. You can unsubscribe at any time. We never sell your data.