Cervical screening
Cervical smear test
Peer reviewed by Dr Rosalyn Adleman, MRCGPLast updated by Dr Toni Hazell, MRCGPLast updated 7 Feb 2025
Meets Patient’s editorial guidelines
- DownloadDownload
- Share
- Language
- Discussion
In this series:Gynaecological cancerCancer of the uterusOvarian cancerCervical cancerVulval cancerVulval intraepithelial neoplasia
A note on terminology - cervical screening is available to those of the female sex, and this leaflet will therefore use the words woman/women and the pronouns she/her. The information also applies to those whose gender identity is not the same as their biological sex, as long as they have not had their cervix surgically removed.
Cervical screening tests (smear tests) are available to women aged 25-64 years in the UK. The tests are done to prevent cervical cancer by finding abnormalities that can, with relatively simple treatments, be prevented from progressing to cervical cancer. Cervical screening tests are not used to diagnose cancer.
In this article:
Video picks for Screening tests
Continue reading below
What is cervical screening?
Cervical screening looks for the human papillomavirus (HPV) which can cause abnormal cells on the cervix. Cervical screening samples are tested for types of HPV that can cause cervical cancer. Cervical screening is a free service on the NHS.
Who is eligible?
All women (those registered female at birth), who have not had their cervix surgically removed, are eligible to have a smear tests. However, only those who are registered as female with a GP automatically receive an invitation by mail. Trans men do not receive invitations if they are registered as male with their GP, and should contact their GP to find out how to access a smear test at the correct time.
How accurate is it?
Testing for HPV first is proven to be a more sensitive and more accurate test than just looking at the cells using a microscope (cytology). It will help to find more people with cervical cell abnormalities that may need treatment. If the HPV test is positive then the cells will be examined under the microscope (cytology) to look for any abnormal cells.
Why is it important?
Most HPV infections are temporary, and slightly abnormal cells often go away on their own when the virus clears. However, if HPV persists, abnormal cells can, if left untreated, turn into cancer over time. You are very unlikely to develop cervical cancer if you have regular cervical screening tests at the times advised by your doctor. If the test shows any abnormality, you will have treatment to stop you ever getting cancer of the cervix. So, an abnormal test usually does not mean you have cancer. It means you should have some treatment to stop you getting cancer.
The HPV vaccination programme started in 2008. if you have had this vaccination, you should still have cervical screening tests, as the vaccine does not protect against all types of HPV. If you were not vaccinated against HPV, but you are now aged under 25, you can access the vaccine via your GP. Some people who are considered to be at higher risk can access the vaccine via a sexual health clinic - more detail on this is in the further reading section.
Cases of cervical cancer have dropped worldwide since HPV vaccination was introduced and it is hoped that cervical cancer will eventually be completely eradicated. However, there are still around 3,300 new cases of cervical cancer diagnosed each year in the UK. Most of these occur in those people who have never had a screening test, or who have not had one for many years. Cervical cancer can be prevented if you have regular screening tests. It is estimated that over 4,000 people are prevented from developing cervical cancer every year in the UK, due to cervical screening.
What happens in a cervical smear test?
The cervix is the lowest part of the womb (uterus). It is often called the neck of the womb. It is inside the vagina. If you were to put a clean finger into your vagina as far as it will go, you should be able to feel your cervix deep inside.
Preparation. You will be asked to remove your clothing from the waist down. If you wear a loose skirt, you may only need to remove your knickers.
Position. You will be asked to lie on your back on the examination couch. You should bend your knees, put your ankles together and let your knees fall open.
Procedure. A doctor or nurse will put an instrument called a speculum into your vagina. The speculum is put in while it is shut. The doctor or nurse then gently opens it. This opens the vagina and allows the cervix to be seen (at the top of the vagina). The doctor or nurse then uses a thin plastic stick with a small soft brush at the end to gently scrape some cells from the surface of the cervix. The cells that are obtained on the brush are sent away to be tested for HPV.
Vaginal speculum and cervical brush
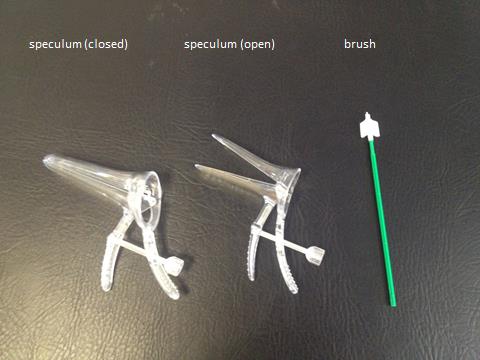
By Dr Mary Harding (Own work), Patient.info©
Female reproductive organs with illustration of cervical smear method
The cervical screening test is not a cancer test. The test is used to detect early abnormalities of the cervix which, if untreated, could lead to cervical cancer in the future.
How to book a smear test
In the UK most people have the test at their GP surgery. It is usually done by the practice nurse. In some areas it can also be done on evenings or weekends at a central GP hub, which may not be at your usual surgery - this is convenient for those who work during the week or for some other reason find it difficult to attend their GP surgery. Smear tests are available at some sexual health clinics, but usually only for certain populations rather than for the general public. This might include transgender people, those with HIV and commercial sex workers; it is likely to vary by area.
How long do smear results take
This takes about two weeks. Ask at your GP surgery for the result of the test if you do not receive it.
The NHS Cervical Screening Programme
Back to contentsThe NHS Cervical Screening Programme in the UK invites all women for regular tests automatically. You need to be registered with a GP, as this is how the programme obtains your name. It is therefore important that your GP has the correct address details for you. Your record on the computer is updated when you have a test so it knows when your next one is due. You should receive a letter asking you to make an appointment to have a test when it is due. Computerised recall systems are good - but not foolproof. Contact your GP if you think you should have had a cervical screening test but have not yet received an invitation to have one.
How often do you have a smear test?
Depending on which country you live in, you may be called at different ages for cervical screening:
Your first invitation for screening is sent six months before your 25th birthday.
If your tests remain negative then you will be invited again at the following intervals:
If you live in Scotland or Wales, you will then be invited for a repeat smear every five years until the age of 64.
If you live in England or Northern Ireland, you will be invited every three years until the age of 49, and then every five years until the age of 64.
Screening stops at the age of 65, unless you have not had a smear test since the age of 50, or if you are still having investigations for a recent abnormal test.
Continue reading below
Do's and don'ts before a smear test
Back to contentsThe following information might answer some questions that you have about when you can or can't have a smear test.
Can you have a smear when you are having your period?
It is best to have your cervical screening test when you are not having your period (menstruating). Ideally, the test is best performed mid-cycle. If you are bleeding heavily, there may be too much blood and mucus on the brush and too few cells from the cervix will be removed.
Can you have a smear test when pregnant?
If you are due your routine cervical screening test and you are pregnant, this should be put back until after your baby is born. Usually, it is advisable to wait until at least 12 weeks after your baby is born. This gives the cervix a chance to recover from pregnancy and childbirth. Tests performed earlier are more likely to be inadequate.
Can you have intercourse before a smear test?
Ideally you should wait 24 hours after having sex (intercourse) before you have a smear test.
Can you have a smear test if you use an intrauterine device (coil) for contraception?
Yes, women who use an intrauterine device for contraception should have smear tests at the usual interval for their age.
Results
Back to contentsThe initial test looks for human papillomavirus (HPV). This is a type of wart virus that can be passed on by having sex. It is involved in the development of nearly all cases of cervical cancer. However, most infections with HPV will clear completely from the body within two years. This means that most people who are infected with HPV do not develop cancer.
A few screening test samples are inadequate and need to be repeated. Inadequate simply means no result can be given, as not enough cervical cells were present for examination under the microscope. If the HPV test result is unavailable or cytology is inadequate at any screening episode, a sample is repeated in no less than three months.
If HPV is not found (normal test result):
You will be offered a further routine screening test appointment in 3-5 years (depending on your age and country, as above).
If the test shows that HPV is present then the same smear sample is looked at under the microscope to see if HPV has caused any abnormal cell changes:
If HPV is found but there are no abnormal cells, a follow-up screen is arranged for 12 months' time. This will check to see if your immune system has cleared the virus. If your test is HPV-negative at 12 months, you will return to routine recall, that is, you will be offered a further screening test in 3-5 years.
If the repeat test at 12 months is still positive for HPV but there are still no abnormal cells, a further follow-up screen is arranged for 12 months' time. This will check to see if your immune system has cleared the virus.
If the smear remains HPV-positive, with normal or abnormal cells, or an inadequate smear sample at the third test, 24 months after the initial HPV positive test, you will be referred for colposcopy.
If HPV is found and there are abnormal cells at any time during routine screening or 12-month review then you will be referred for colposcopy (see below).
Abnormal cells
There are a range of changes that may occur. In nearly all cases, these changes do not mean cancer.
Dyskaryosis is a medical term used to describe abnormal cell changes, seen with cervical screening. Dyskaryosis is not cancer. About 9 out of 10 cases of dyskaryosis revert back to normal on their own, without treatment. Nearly all abnormal tests show no more than small changes in the cervical cells.
Borderline change is the mildest abnormality seen on cervical screening. About 3-4 in 100 results are borderline. Whilst the cells are not quite normal, they are not abnormal enough to be categorised as dyskaryosis.
Mild dyskaryosis is a common abnormal result from cervical screening. About 2 tests in every 100 show mild abnormalities of the cervical cells. Most of these changes go back to normal without any treatment.
Moderate or severe dyskaryosis. About 1 in every 100 smear tests shows either one of these abnormalities. If your test shows moderate or severe dyskaryosis it is still very unlikely that you will have cervical cancer. The main difference is that these changes are less likely to return to normal by themselves. You will probably need some treatment and this will happen at colposcopy.
Invasive or glandular neoplasia is a more serious abnormality which shows in fewer less than 1 test in 1,000. Neoplasia means new growth of cells. Invasive neoplasia suggests cervical cancer might be present. This is not proven until a sample of cervical tissue (a biopsy) has been taken at colposcopy. Glandular neoplasia is another significant abnormality that can be seen on cervical screening. It suggests that there is an abnormality in the lining of the womb (the endometrium), rather than on the cervix. This is because glandular cells (found lining the womb) are different to the ones normally found on the cervix. Glandular neoplasia again does not necessarily mean cancer, but cancer needs to be excluded. You will probably need to have a colposcopy and may need to have a small camera passed into the womb (called hysteroscopy).
It is important to remember that it is rare for cervical cancer to be found on cervical screening. Screening is designed to find early changes that could become cancer in the future, if left untreated.
Continue reading below
Can abnormal cervical cells be treated?
Back to contentsYes, but it might not be needed - minor abnormal change often go away without treatment. This is why a repeat test after 3-12 months may be all that is needed. If the cells remain abnormal, or the changes are more marked, treatment is offered at a colposcopy clinic. This will stop cancer from developing in the future. Treatment, if needed, is simple and almost 100% effective. Treatment is done at the colposcopy session. Abnormal cells are removed or destroyed by freezing, burning, laser or cutting them away.
Colposcopy
Colposcopy is a more detailed examination of the neck of the womb (cervix). An instrument called a colposcope is used to magnify the cervix so it can be seen in more detail.
You may be referred for a colposcopy if you have one of the higher grades of abnormality on your test. You may also be referred for colposcopy if you have had three inadequate or borderline results in a row, or if you have had three abnormal results (of any grade) within a 10-year period.
The laboratory that reports the cervical screening results will determine whether you need to be referred for colposcopy (based on the current result and your past results). Usually in the UK the laboratory will refer you directly to colposcopy, and they will let you and your GP know and send you an information leaflet about the process. Read more in the separate leaflet called Colposcopy and cervical treatments.
It is probably best to delay your colposcopy examination if your period starts. It is not impossible to perform colposcopy when you are menstruating, but it can make it difficult to get a good view. You should ring up the clinic where you have your appointment to check whether they would prefer you to reschedule or not.
You should attend colposcopy even if you are pregnant; make sure you tell the health professionals that you are pregnant, even if it is very early in the pregnancy. Colposcopy can be safely carried out on pregnant women. As long as no major problems are found, treatments will probably be delayed until after you have had your baby. Sometimes repeat colposcopy may be done later in pregnancy. It is possible to give treatment to the cervix, if it is essential, whilst you are pregnant.
Common questions
Back to contentsI have never had sex. Do I need a cervical screening test?
The test is recommended for all women, even if you have never had sex. Any sexual activity carries the risk of HPV, not just full sex, but those who have never had sex have a much lower risk. There are also other, less common types of cervical cancer, not caused by HPV, so anyone with a cervix who has never had sex is still at risk.
For more information, see the separate leaflets called HPV vaccine and Cervical cancer. You may decide that you do not want to have a test if you have never had sex.
I am a lesbian. Do I need a cervical screening test?
Yes. If you are a lesbian, you are still advised to have cervical screening. This is because there is still a risk of cervical cancer, and HPV can still be transmitted between partners. Additionally, some lesbians may have had sexual contact with a man in the past.
I have had a hysterectomy - do I need to have a cervical screening test?
This depends on the type of hysterectomy, and why it was done. Your doctor will advise you on this. In general, if you have a total hysterectomy - removal of the womb (uterus) and cervix - for a reason not due to cancer, you no longer need cervical screening tests. Some types of hysterectomy leave the cervix (called subtotal hysterectomy), and some are done to remove a cancer. In these situations, a test of the cells of the remaining cervix, or of the top of the vagina (called the vault), may still be advised.
Does the cervical screening test really save lives?
Yes. By studying the statistics of cancer cases since the tests began it is estimated that up to 4,500 cases of cervical cancer are prevented each year in the UK. After screening was introduced, the number of cases of cervical cancer each year dropped by almost half.
Wouldn't it be better to have yearly tests?
No - yearly cervical screening is not usually recommended. This is because cervical cancer takes a long time to develop. The early changes that can occur in cervical cells often improve without treatment anyway. More frequent screening would be expensive for the NHS, is unlikely to identify or prevent any more cancers, and could cause physical or psychological harm - through over-treatment or anxiety. More frequent cervical screening is therefore not a cost-effective use of resources.
Some people will need to have more frequent cervical screening or colposcopy, after abnormal results or cervical treatment. This is an extremely important part of follow-up. Your doctor will advise you how often you need to be recalled.
Why isn't cervical screening offered before age 25?
This decision was made by a panel of experts who looked at all the evidence. Their main reasons are:
Cervical cancer is extremely rare in those under 25 years of age.
Abnormal cervical screening test results are very common under the age of 25. Many of these changes seen revert back to normal without any treatment.
Cervical screening in those aged under 25 may do more harm than good. People may be very anxious and worried about abnormalities that eventually go away anyway. Also, there is the potential for harm to occur, as these people might end up being over-treated. This would mean removing cells from the cervix earlier than was needed, perhaps without waiting for the problems to go away by themselves. This can lead to problems in the future, particularly a risk of any future babies being born too early (prematurity).
It is really important not to miss your first invitation for cervical screening at age 25. Otherwise, there is the potential (especially if you have been sexually active since her teenage years) for abnormalities in the cervix to become more serious. So, the main risk of starting the screening programme at age 25, is that some people might miss their first invitation. However, since the starting age was changed from 20 to 25 (in 2013), experts have been following up the effect and there has been no rise in cancers in this age group.
I have irregular bleeding - do I need to have a cervical screening test straightaway?
No. Cervical screening is a routine test performed on people without any symptoms. The aim is to look for problems in cervical cells that could become cancer in the future. A cervical screening test would not be used as an investigation for irregular bleeding (but you should still attend for your cervical screening test when invited).
If you get any of the following symptoms, you should see your GP as soon as possible, even if you have recently had a normal smear test.
Bleeding after having sex (called postcoital bleeding).
Bleeding between periods (called intermenstrual bleeding).
Bleeding after the menopause (called postmenopausal bleeding)
I am a trans man - do I need cervical screening?
If you were born female, you still need to have cervical screening if you have retained your cervix. If you have had a total hysterectomy (with removal of the cervix), you do not need to attend for screening. Some trans men find that a smear test makes their gender dysphoria worse - let your GP practice know if you are worried about this.
I have HIV infection - do I need to do anything differently?
People with HIV infection should ideally have cervical screening and colposcopy when their disease is diagnosed. Current recommendations are to have a cervical screening test every year, even if the test is normal each year. This is because HIV increases your risk of developing cervical cancer.
Does being immunosuppressed increase my risk of cervical cancer?
Yes - people who are immunosuppressed are at an increased risk of having changes that may become cancerous. Immunosuppressed means your immune system doesn't work well. This may be because of certain diseases or medicines. The main groups affected are:
People with HIV - the virus that causes AIDS. These people need yearly cervical screening (see above).
People with kidney failure who require dialysis (or any other disease with a high chance of needing organ transplantation) should have a cervical smear and/or colposcopy done as soon as possible after the decision for transplant or dialysis has been made. However, it is not recommended that these people have more frequent cervical screening - just that early referral to colposcopy is advisable with any abnormal screening results.
People who have had an organ transplant should ideally have a smear test less than a year before their transplant.
People taking cytotoxic medicines for rheumatological disorders, immunosuppressive medicines after other transplants, chemotherapy for cancer, steroids or tamoxifen have not been shown to be at increased risk. They should, however, have regular screening in line with their age group.
Does a cervical smear hurt?
Cervical screening tests are not painful, although some people find the speculum uncomfortable. It generally helps if you can relax - this makes the experience better for you and easier for the person taking the sample. The sample taken from your cervix is put into some liquid to be sent to the laboratory for testing. If there is a particular reason why you are very nervous about having this test, for example you have been a victim of sexual assault in the past, or you find examinations difficult for some other reason, please tell your practice. They may be able to arrange a longer appointment or make other adjustments.
I'm nervous about having a smear - can I do a self-taken swab for HPV instead?
Trials have been done where women have been given a swab to take themselves. Only those whose swab is positive for HPV need to then have a smear test taken with a speculum. We are not 100% certain whether this is as sensitive as a smear test taken with a speculum, or whether there is a risk that some cases of HPV will be missed. For this reason, it is not yet offered as an alternative for all women. However, in some areas women who have not had a smear test for many years are being offered such a swab, as it is definitely better than having no screening at all.
Should I worry if I have bleeding after a smear?
A little bit of light bleeding or spotting for up to a day after having a smear test may sometimes happen, and is normal.
Patient picks for Screening tests

Tests and investigations
Chorionic villus sampling
Chorionic villus sampling (CVS) is a procedure that is carried out during pregnancy to diagnose or exclude various chromosomal or genetic conditions.
by Dr Mary Harding, MRCGP

Tests and investigations
NHS screening programme
Screening involves tests on people without symptoms to check if they have a disease or condition before it causes symptoms. The reason for screening is the expectation that a problem can be discovered in the early stages and either prevented from progressing further or treated before they cause significant problems. Not all conditions have suitable tests which allow them to be detected early, and not all conditions can be treated successfully even if they are picked up early on. Therefore, only certain conditions are part of our national screening programmes. The screening programmes currently available in the UK are listed below.
by Dr Philippa Vincent, MRCGP
Further reading and references
- Cervical cancer - UK mortality statistics; Cancer Research UK
- Population Screening Programmes (England); GOV.UK
- Arbyn M, Roelens J, Simoens C, et al; Human papillomavirus testing versus repeat cytology for triage of minor cytological cervical lesions. Cochrane Database Syst Rev. 2013 Mar 28;3:CD008054. doi: 10.1002/14651858.CD008054.pub2.
- Koliopoulos G, Nyaga VN, Santesso N, et al; Cytology versus HPV testing for cervical cancer screening in the general population. Cochrane Database Syst Rev. 2017 Aug 10;8:CD008587. doi: 10.1002/14651858.CD008587.pub2.
- Cervical screening; NICE CKS, September 2022 (UK access only)
- CKS Cervical cancer and HPV; NICE CKS, February 2022 (UK access only)
- Cervical screening; Public Health Scotland
- Cervical Screening Wales; Public Health Wales
- Cervical screening; HSC Northern Ireland Public Health Agency
- HPV vaccine; NHS September 2023
- HPV self-sampling could help screen one million more women for cervical cancer; CRUK, 2024
Continue reading below
Article history
The information on this page is written and peer reviewed by qualified clinicians.
Next review due: 6 Feb 2028
7 Feb 2025 | Latest version

Ask, share, connect.
Browse discussions, ask questions, and share experiences across hundreds of health topics.

Feeling unwell?
Assess your symptoms online for free
Sign up to the Patient newsletter
Your weekly dose of clear, trustworthy health advice - written to help you feel informed, confident and in control.
By subscribing you accept our Privacy Policy. You can unsubscribe at any time. We never sell your data.