Giant Cell Arteritis
Giant cell arteritis
Peer reviewed by Dr Rosalyn Adleman, MRCGPLast updated by Dr Philippa Vincent, MRCGPLast updated 24 Jul 2025
Meets Patient’s editorial guidelines
- DownloadDownload
- Share
- Language
- Discussion
In this series:Visual problemsMacular degenerationEye floaters, flashes and haloesRetinal vein occlusionVitreous haemorrhageSquint in children
Giant cell arteritis is also known as temporal arteritis.
The typical symptoms of giant cell arteritis (temporal arteritis) are headache, tenderness over one or both sides of the forehead, and feeling generally unwell. Other symptoms that may occur include pain in your jaw muscles when chewing, and visual loss.
Seek medical attention immediately if you suspect that you have giant cell arteritis. People with giant cell arteritis need urgent treatment with steroids. Prompt treatment aims to prevent serious complications such as severe sight impairment which can occur soon after the disease starts.
In this article:
Continue reading below
What is giant cell arteritis?
Giant cell arteritis (GCA), also known as temporal arteritis, is a condition which causes inflammation on the inside of some blood vessels (arteries). It is called 'giant cell' because abnormal large cells develop in the wall of these inflamed arteries. The arteries affected are those which supply blood to the head. Several arteries may be affected at the same time; part of the aorta (the biggest artery in the body) is called the "arch of the aorta" - this is the part of the aorta which has arteries coming from it to supply the head with blood. These are the arteries that are typically affected by giant cell arteritis (temporal arteritis).
One of the arteries that is commonly affected is the temporal artery. (You have a temporal artery on each side of your head. They lie under the skin to the sides of the forehead - the temple area - and supply blood to this area).
This is why the condition is also called temporal arteritis.
Giant cell arteritis (temporal arteritis) causes
No one really knows exactly what causes giant cell arteritis (temporal arteritis). We do know that there are genetic changes in some people which make them more likely to develop giant cell (temporal) arteritis.
Continue reading below
Who is likely to develop giant cell arteritis (temporal arteritis)?
Giant cell (temporal) arteritis is uncommon. It mainly affects people over the age of 70 years. It is extremely rare for it to occur in people under the age of 50.
Women are more commonly affected than men. Studies in the United States have suggested that about 1 in 100 women develop this in their lifetime and about 1 in 200 men. It is most common in people in Scandinavian countries or of Northern European and Scandinavian descent. It is less common with people from African, Asian, Japanese or Arabic heritage.
About half the people with giant cell (temporal) arteritis also have a condition called polymyalgia rheumatica. Fewer than one in five people with polymyalgia rheumatica develop giant cell (temporal) arteritis.
Giant cell arteritis (temporal arteritis) symptoms
Symptoms of giant cell (temporal) arteritis can vary, and may depend on which artery or arteries are mainly affected.
Headache is the common symptom. It occurs in about two thirds of people with giant cell arteritis (GCA). This typically develops suddenly over a day or so but it sometimes develops gradually over several days or weeks. The headache can be one-sided, or on both sides. Typically, it affects the temple (the sides of the head), but it can affect any part of the head.
Tenderness of the scalp over the temporal arteries is common. You may be able to feel one or both of the inflamed temporal arteries under the skin, or see that they are more swollen than normal.
Other symptoms may occur if the arteries going to these parts of the body are inflamed, become narrowed and reduce the blood supply to these areas. These include:
Pain in the jaw muscles (jaw claudication) while eating or talking. This jaw pain occurs in nearly half of affected people. The pain eases when you rest the jaw muscles and gradually gets worse the more that you use them.
Visual disturbances: partial or complete loss of vision in one or both eyes occurs in about 1 in 5 affected people and is often an early symptom. People who are affected typically report a feeling of a shade covering one eye, which can progress to total loss of vision. The eye is not painful. If untreated, the second eye is likely to become affected within 1-2 weeks, although it can be affected within 24 hours. Urgent treatment is therefore essential. A temporary loss of vision in one eye or double vision (diplopia) may occur as a 'warning' symptom before any permanent visual loss. Permanent visual loss occurs in about 1 in 12 people with giant cell arteritis (temporal arteritis).
Some general symptoms also occur in almost half the people with giant cell arteritis (temporal arteritis). These include tiredness, depression, night sweats, fever, loss of appetite, and weight loss. These symptoms may develop gradually and may be present for weeks before a specific symptom such as headache develops.
Polymyalgia rheumatica - is often also present
Half of the people with giant cell arteritis develop a related condition called polymyalgia rheumatica (PMR); one in five people with PMR will develop giant cell (temporal) arteritis. It often occurs at the same time but may occur before or after the development of giant cell arteritis (temporal arteritis).
The typical symptoms of PMR are pain, tenderness and stiffness of muscles around:
The shoulders and upper arms.
Sometimes around the hips and neck.
PMR is due to inflammation in the affected muscles, but the cause is unknown. The treatment is similar for both conditions. Treatment for PMR is usually very effective. See the separate leaflet called Polymyalgia rheumatica for more details.
Continue reading below
What are the possible complications of giant cell arteritis?
Note: complications are much less likely to occur if treatment is started soon after symptoms begin.
Possible complications include the following:
Total loss of vision in one or both eyes
If an affected blood vessel (artery) becomes very swollen (inflamed), the blood supply going down that artery can become blocked. The most common arteries this affects are the small arteries going to the eye. If one of these arteries becomes blocked it can cause permanent, serious visual problems, even total loss of vision, in the affected eye. Visual loss or disturbances can be temporary or permanent. They affect 1 in 5 people with giant cell (temporal) arteritis. Permanent loss of vision may occur in up to 1 in 12 people with untreated giant cell arteritis (GCA). Therefore, treatment is aimed at preventing visual loss or, if visual loss has occurred in one eye, to prevent loss in the other eye. However, even with treatment, visual loss occurs in up to 1 in 20 cases.
Problems related to other arteries being affected
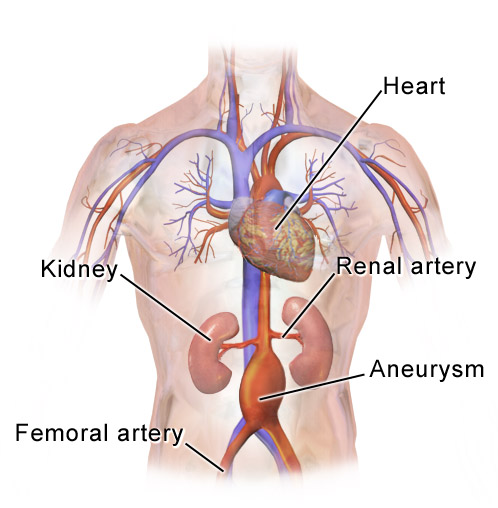
Other serious complications sometimes develop if the inflammation occurs in other arteries. For example, serious complications can include a heart attack, an aortic aneurysm, a stroke, damage to nerves, or deafness (caused by a blocked artery affecting hearing).
Do I need any tests for giant cell arteritis (temporal arteritis)?
A blood test can detect if there is inflammation in your body. This is the erythrocyte sedimentation rate (ESR) test or the C-reactive protein (CRP) test. If the blood test shows a high level of inflammation and you have the typical symptoms then giant cell arteritis is likely. However, the blood test is not specific for GCA (it can also be high in other inflammatory disorders). Also, some people with GCA have a normal blood test but this is unusual - only 4 in 100 people with giant cell (temporal) arteritis have normal ESR and CRP blood tests.
Biopsy. To confirm the diagnosis a hospital doctor may take a small part of the temporal artery (a biopsy) to look at under a microscope. If you have GCA the pathologist looking at the sample can see the inflammation and abnormal giant cells in the sample of the blood vessel (artery) wall. This was historically the test performed to confirm the diagnosis but increasingly ultrasound scans are being used instead.
Doppler ultrasound scan. These tests are less invasive and very accurate for testing for giant cell (temporal) arteritis. Guidelines suggest that they should be used first nowadays and biopsies are then needed in fewer people where the diagnosis remains unclear.
Giant cell arteritis (temporal arteritis) treatment
If giant cell arteritis is suspected, treatment is usually started straightaway - even before the diagnosis is confirmed with scans or biopsies. As long as the tests are performed within a week of starting the treatment, they will still show the signs of giant cell (temporal) arteritis. The main aim is to reduce the risk of possible complications. The second aim is to relieve the headache and any other symptoms.
Steroid tablets
A steroid medicine such as prednisolone is the usual main treatment. Steroids work by reducing inflammation. After starting treatment, symptoms usually ease within a few days.
A high dose of steroid is started at first, usually between 40 and 60 mg per day. This dose is usually maintained for between 2 and 4 weeks and is then reduced gradually to a lower 'maintenance' dose. It may take several months to reduce the dose gradually. The initial reduction is by 2.5 mg every 2 to 4 weeks until a dose of 10 mg a day and then reduced more gradually, usually by 1 mg every 4-8 weeks. The maintenance dose needed to keep symptoms away and prevent complications varies from person to person.
Steroid withdrawal should always take place under the supervision of a doctor, usually a rheumatologist. The aim is to try and stop the steroids by about 18 months although some people need to remain on them for longer. Relapses can be common after stopping or reducing the steroid dose.
People being prescribed long-term steroids will usually also be prescribed calcium and medication to protect the stomach (proton pump inhibitors).
Other treatments
Studies have shown that the use of a medication called tocilizumab alongside the steroids improves the chances of stopping or reducing the steroids without relapse. In the UK, the National Institute for Health and Care Excellence (NICE) guidance is currently that this should only be used in people who have already had a relapse or who are not responding well to steroids. The guidance also states that tocilizumab can only be used for a maximum of one year.
Some other points about steroid tablets
Do not stop taking steroid tablets suddenly. It probably does no harm if you forget to take the odd tablet. However, once your body is used to steroids, if you stop the tablets suddenly you may develop serious withdrawal effects within a few days.
Do not take anti-inflammatory painkillers whilst you take steroids, unless advised by a doctor. The two together increase your risk of developing a stomach ulcer.
Most people who take regular steroids carry a steroid card. This gives details of your dose, condition, etc, in case of emergencies.
If you are ill with other conditions, or have surgery, the dose of steroid may need to be increased for a short time. This is because you need more steroid during physical stress.
Side-effects
The risk of developing side-effects from steroids is increased with higher doses. This is why the dose used is the lowest that keeps symptoms away. Possible side-effects from steroids include the following:
'Thinning of the bones' (osteoporosis) - but you can take a medicine to help protect against this. Because the dose of steroids for giant cell (temporal) arteritis is high, everyone who is having steroids to treat this should also be offered a medication called a bisphosphonate to reduce the risks of osteoporosis. See the separate leaflet called Preventing steroid-induced osteoporosis for more information.
Increased chance of infections - in particular, a severe form of chickenpox and measles. Note: most people have had chickenpox and are immune to it. Also, most people have been immunised against measles and are therefore immune (or people born before the MMR vaccine was available are likely to have had measles and be immune due to that). But, if you have not had chickenpox or measles (or immunisation for measles), keep away from people with measles, chickenpox, or shingles (which is caused by the same virus as chickenpox).
Weight gain.
Increase in blood pressure. Have your blood pressure checked regularly. It can be treated if it becomes high.
High blood sugar, This may mean extra treatment if you have diabetes. Steroids also may cause diabetes to develop. If you take long-term steroids, you should have a yearly blood sugar test to check for diabetes. Steroid-induced diabetes may resolve once you stop taking the steroids.
Skin problems such as poor healing after injuries, thinning skin and easy bruising. Stretchmarks sometimes develop.
Muscle weakness.
Mood and behavioural changes. Some people actually feel better in themselves when they take steroids. However, steroids may aggravate depression and other mental health problems and may occasionally cause mental health problems. If this side-effect occurs it tends to happen within a few weeks of starting treatment and is more likely with higher doses. Some people become confused and irritable. They may even develop delusions and suicidal thoughts. These mental health effects can also occur when steroid treatment is being withdrawn. Seek medical advice if worrying mood or behavioural changes occur.
An increased risk of developing cataracts.
An increased risk of duodenal ulcers and stomach ulcers. Seek medical advice if you develop indigestion or stomach (abdominal) pains.
Although the above points have to be mentioned, the benefits of steroids normally outweigh any of the risks. The relief of symptoms and the prevention of serious complications mean that steroids are essential treatment for giant cell (temporal) arteritis.
Patient picks for Arteries
Heart health and blood vessels
Abdominal aortic aneurysm
The aorta is the main blood vessel in the abdomen, running down from your heart. It is normally about the diameter of a garden hose. In older people, particularly those who smoke, part of it can enlarge and balloon up. This is called an abdominal aortic aneurysm (often abbreviated to AAA, pronounced 'triple-A'). This doesn't cause any symptoms and the person is usually unaware they have it, until it leaks or bursts. The medical term for this is rupture. If the aneurysm ruptures, it can be fatal. In the UK there is a screening programme for men over the age of 65, to see if they have a triple-A. An operation to repair the aneurysm may be advised if it is larger than 5.5 cm, as above this size the risk of rupture increases significantly.
by Dr Doug McKechnie, MRCGP

Heart health and blood vessels
Pulmonary embolism
A pulmonary embolism (embolus) is a serious, potentially life-threatening condition. It is due to a blockage in a blood vessel in the lungs. A pulmonary embolism (PE) can cause symptoms such as chest pain or breathlessness. It may have no symptoms and be hard to detect. A massive PE can cause collapse and death. PE usually happens due to an underlying blood clot in the leg - deep vein thrombosis (DVT). Prompt treatment is important and can be life-saving. Pregnancy, various medical conditions and medicines, immobility and major surgery all increase the risk of a PE. Anticoagulation, initially with heparin and then warfarin, or other oral blood thinning tablets, is the usual treatment for PE.
by Dr Rachel Hudson, MRCGP
Further reading and references
- Giant cell arteritis; NICE CKS, July 2024 (UK access only)
- Serling-Boyd N, Stone JH; Recent advances in the diagnosis and management of giant cell arteritis. Curr Opin Rheumatol. 2020 May;32(3):201-207. doi: 10.1097/BOR.0000000000000700.
- Giant cell arteritis: Update on clinical manifestations, diagnosis, and management; N Farina et al; European Journal of Internal Medicine
- Ameer MA, Vaqar S, Khazaeni B; Giant Cell Arteritis (Temporal Arteritis).
Continue reading below
Article history
The information on this page is written and peer reviewed by qualified clinicians.
Next review due: 23 Jul 2028
24 Jul 2025 | Latest version

Ask, share, connect.
Browse discussions, ask questions, and share experiences across hundreds of health topics.

Feeling unwell?
Assess your symptoms online for free
Sign up to the Patient newsletter
Your weekly dose of clear, trustworthy health advice - written to help you feel informed, confident and in control.
By subscribing you accept our Privacy Policy. You can unsubscribe at any time. We never sell your data.