Vitreous haemorrhage
Peer reviewed by Dr Doug McKechnie, MRCGPLast updated by Dr Colin Tidy, MRCGPLast updated 29 Jun 2024
Meets Patient’s editorial guidelines
- DownloadDownload
- Share
- Language
- Discussion
- Audio Version
In this series:Visual problemsMacular degenerationEye floaters, flashes and haloesRetinal vein occlusionGiant Cell ArteritisSquint in children
Vitreous haemorrhage is bleeding into the jelly-like filling of the back part of your eye. This substance is the vitreous humour. It helps the eye keep its shape and is normally clear, allowing light from outside the eye to pass through it to reach the retina.
Vitreous haemorrhage varies in degree from mild, with 'floaters' and haziness in the vision, to complete loss of vision. It is painless and it comes on quite quickly. Usually only one eye is affected. Whilst it is very alarming, once the bleeding has been treated, many cases resolve and vision is restored to where it was before.
In this article:
Video picks for Eye conditions
Continue reading below
What is vitreous haemorrhage?
Vitreous haemorrhage occurs when blood leaks into the vitreous humour inside the eye. The leaked blood most commonly comes from blood vessels at the back of the eye (retinal blood vessels). This is more likely to happen if the blood vessels have been damaged (eg, by trauma) or are particularly fragile (because of eye disease related to diabetes).
In order for us to see clearly, the vitreous humour needs to be clear. If the vitreous humour is clouded or filled with blood, vision will be impaired. This impairment varies from a few 'floaters' and cloudiness of the vision through to the vision going completely dark (sometimes with a reddish tinge).
Vitreous haemorrhage can therefore cause anything from floaters, hazy or dulled vision (reduced visual acuity) to complete loss of vision.
What is the vitreous humour?
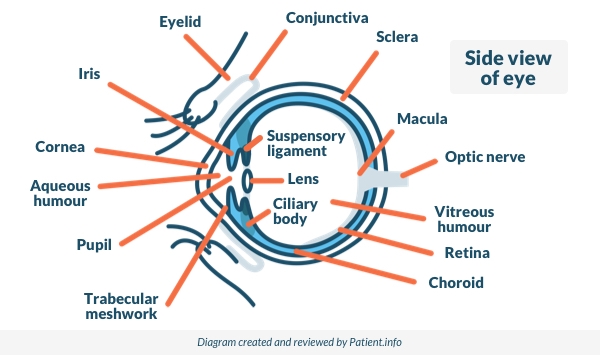
Back to contentsThe vitreous humour is a clear jelly-like substance that makes up about 80% of the volume of the globe of the eye. It supports the shape of the globe of the eye whilst letting light through.
It is made up mainly of water but with some collagen and hyaluronic acid. The outside is made of fine fibres which are attached to the retina at the back and to the back of the lens at the front.
Side View of the Eye
Continue reading below
What are the causes of vitreous haemorrhage?
Back to contentsThe most common causes, accounting for about 90% of all cases of vitreous haemorrhage, are:
Bleeding from abnormal new blood vessels forming in advanced diabetic eye disease.
Bleeding from tears in the retina caused by vitreous detachment (see below).
Trauma to the eye (the most common cause in younger people).
Bleeding inside the eye can come from:
Abnormal blood vessels which grow because the back of the eye is short of oxygen. These are fragile and bleed easily. Conditions in which this can occur include:
Diabetic eye disease (the most common cause).
Retinopathy with sickle cell disease.
Damage to the back of the eye in very premature babies who have been on oxygen in special care baby units.
Normal blood vessels which are damaged. They may be damaged by:
Posterior vitreous detachment, often because it causes a retinal tear (see below).
Retinal macroaneurysms - swollen blood vessels on the retina, usually related to high blood pressure, atherosclerosis and smoking.
Blunt trauma - suddenly compressing the eye - for example, if hit by a squash ball.
Penetrating trauma - this will cause bleeding throughout the eye. Penetrating trauma can occur from high-velocity injuries such as grinding and hammering. They do not always cause severe eye pain.
Subarachnoid haemorrhage, which can increase the pressure in the veins in the retina, causing them to bleed.
Surgery to the eye, particularly if it involves the inside of the eye.
Blood from behind the retina tracking through into the eye. This is the least common cause of vitreous haemorrhage. It may result from:
Tumours of the back of the eye (eye tumours are rare. The most common type is ocular melanoma).
Fragile new blood vessels behind the retina.
Posterior vitreous detachment is usually experienced between the ages of 60 and 80 - it happens to most of us between those ages. It occurs when the vitreous pulls away from the retina at the back. This can happen quite suddenly as the vitreous tends to shrink with age.
Most commonly there are no symptoms. Sometimes posterior vitreous detachment causes bleeding from the retina as it pulls away. Sometimes the retina is torn as the vitreous pulls away from it - in this case bleeding is more likely.
Most people experience posterior vitreous detachment in their 60s or later, and most do not have significant vitreous haemorrhage when it happens. However, episodes of noticeable floaters are very common and are probably caused by tiny bleeds.
Vitreous haemorrhage symptoms
Back to contentsThe symptoms of smaller bleeds (most bleeds are smaller bleeds) include:
Floaters in vision.
Cobweb haze.
Haze and shadows in the eye.
Red tint to the vision.
Symptoms most commonly affect one eye only, although both eyes can be affected.
Some people find that their vision is worse in the morning, because blood settles to the back of the eye overnight whilst lying down.
More severe bleeds cause:
Haziness of vision.
Blind spots or dark streaks.
The most severe bleeds cause visual loss, which can be complete, leaving the vision hazily red or black. For most people this is extremely alarming, particularly as it tends to come on very quickly with no clear explanation.
Continue reading below
How common is vitreous haemorrhage?
Back to contentsVitreous haemorrhage affects about 7 per 100,000 people each year. This makes it one of the most common causes of sudden deterioration in vision. It most often affects only one eye.
Who is likely to experience vitreous haemorrhage?
Back to contentsThe most common cause of vitreous haemorrhage is severe diabetic eye disease, which is mainly seen in older adults. The other common causes of vitreous haemorrhage also tend to occur in adults aged 60 and above, except for eye trauma, which can occur at any age.
How is vitreous haemorrhage diagnosed?
Back to contentsAn examination using a slit lamp is performed by opticians and eye specialists (ophthalmologists) to look in detail at the inside of the eye. The slit lamp will allow the examiner to see if there is blood in the vitreous.
Finding the source of the bleeding may be possible with the slit lamp, although if there is a lot of blood in the vitreous humour this prevents a clear view and it may therefore be difficult to know what has happened. In this case an ultrasound scan of your eye can help. Ultrasound can detect many causes of vitreous haemorrhage, including posterior vitreous detachment, retinal tears and detachments, tumours and foreign objects.
Sometimes an angiogram is needed. This test shows up the blood vessels in the back of the eye. This can be helpful if looking for abnormal blood vessels such as in diabetes.
Computerised tomography (CT) scanning of the eyes is useful if there is a suspicion of a penetrating injury.
What is the treatment for vitreous haemorrhage?
Back to contentsThe treatment of vitreous haemorrhage varies with the cause. Aims of treatment are to:
Find the source of the bleeding.
Stop the bleeding.
Repair any damage to the retina before it results in permanent loss of vision.
Restore normal vision.
Once the source of the bleeding has been identified, treatment will depend on the cause. If there is not too much blood in the vitreous and the source of bleeding can be seen then it is treated. This means laser treatment to bleeding vessels and any other abnormal vessels, and repair to any tears in the retina. After this it is a matter of waiting for the blood to slowly clear as the red blood cells break down. This can take several weeks.
Strenuous activity should be avoided for several days at least, as this might dislodge clots and trigger new bleeding. It is also advised to sleep with the head of the bed elevated, as this allows the blood in the vitreous to settle into the bottom of the eye, out of the line of vision.
If the blood in the vitreous obscures the view and prevents treatment of the bleeding then the entire vitreous may be removed first. This procedure is called a vitrectomy. Doctors will perform a vitrectomy if they can't see the back of the eye, or if the view isn't good enough to treat the bleeding there safely.
Specific treatments
Laser photocoagulation
This is the usual treatment for fragile abnormal vessels. Treating them both stops the bleeding and prevents later bleeding. Laser photocoagulation is also used in repairing damage to the retina, including retinal detachments.
Anti-VEGF injections
Anti-VEGF injections (a type of intravitreal injection) aim to shrink abnormal new vessels which have formed in the eye. They are sometimes used in patients with diabetes, in addition to other treatments like laser photocoagulation and vitrectomy, in order to reduce bleeding.
Cryotherapy
This is also used as a treatment for retinal tears and retinal detachments.
Vitrectomy
Vitrectomy is removal of the vitreous humour completely, together with the membrane that surrounds it. This is done when there is so much blood in the vitreous that it is impossible to diagnose and treat the cause. Vitrectomy is also sometimes performed if the blood in the vitreous is clearing very slowly and vision remains impaired.
Waiting
Waiting is commonly the chosen option once the bleeding has stopped. Most cases of vitreous haemorrhage do not require vitrectomy. The blood clears slowly from the vitreous, allowing light to pass through it again. If the underlying vision is undamaged then normal vision will be restored.
General measures
Anyone with a suspected vitreous haemorrhage will usually be seen by an eye specialist on the same day. This is because sudden loss of vision is considered an eye emergency. The aim is to ensure accurate diagnosis and to avoid permanent loss of vision which could occur if there is a retinal detachment behind the bleeding.
Anyone who has a sudden loss of vision or any other unexplained disturbance in vision in one or both eyes should:
See a GP or optician, or attend an accident and emergency department, as soon as possible.
Try to remain calm - most vitreous haemorrhages respond well to treatment and there is a very good chance that vision will return to where it was.
Rest for a few hours a day sitting upwards and elevate the head at night on pillows.
Ask a GP to check blood pressure - raised blood pressure increases the chance of further bleeding.
Avoid any heavy lifting, which can increase the chance of further bleeding.
What is the outlook for vitreous haemorrhage?
Back to contentsThe outlook (prognosis) in vitreous haemorrhage depends both on the cause and on the severity.
Vitreous haemorrhage resulting from posterior vitreous detachment usually has a good prognosis, with restoration of vision, particularly if the eye is otherwise normal.
Where severe diabetic eye disease or macular degeneration has resulted in abnormal blood vessels, the outlook for the vision is much less good. The outlook in penetrating eye injury is often poor.
How is vitreous haemorrhage prevented?
Back to contentsPrevention of vitreous haemorrhage involves preventing the underlying causes. This includes careful and regular management of diabetic eye disease (which tends to be worse in less well-controlled diabetes) and high blood pressure, and giving up smoking.
The eye should always be protected from trauma during high-risk activities such as filing, grinding and hammering, using firearms and playing sports with high-speed balls, such as squash.
Dr Mary Lowth is an author or the original author of this leaflet.
Patient picks for Eye conditions

Eye health
Colour vision deficiency
Colour vision deficiency, also called colour blindness, is when you are unable to see certain colours. The most common form of the condition is red-green colour vision deficiency.
by Dr Hayley Willacy, FRCGP

Eye health
Astigmatism
Astigmatism is a common eye condition that affects the shape of the cornea or the lens of the eye. The cornea and lens are typically smooth and round in shape, but in people with astigmatism, they are irregularly shaped. The main symptom of astigmatism is blurred vision. It occurs because the cornea at the front of the eye is unevenly curved. Vision problems, such as astigmatism, are also known as refractive errors. Astigmatism is a common condition that can be corrected by glasses or contact lenses, or cured with laser eye surgery.
by Dr Doug McKechnie, MRCGP
Further reading and references
- Shaikh N, Srishti R, Khanum A, et al; Vitreous hemorrhage - Causes, diagnosis, and management. Indian J Ophthalmol. 2023 Jan;71(1):28-38. doi: 10.4103/ijo.IJO_928_22.
- Mathen,T, Leng, T, Shah VA; Terson Syndrome, EyeWiki - American Academy of Ophthalmology
Continue reading below
Article history
The information on this page is written and peer reviewed by qualified clinicians.
Next review due: 28 Jun 2027
29 Jun 2024 | Latest version

Ask, share, connect.
Browse discussions, ask questions, and share experiences across hundreds of health topics.

Feeling unwell?
Assess your symptoms online for free
Sign up to the Patient newsletter
Your weekly dose of clear, trustworthy health advice - written to help you feel informed, confident and in control.
By subscribing you accept our Privacy Policy. You can unsubscribe at any time. We never sell your data.