Polycythaemia rubra vera
High red blood cell count
Peer reviewed by Dr Toni Hazell, MRCGPLast updated by Dr Hayley Willacy, FRCGP Last updated 26 Feb 2023
Meets Patient’s editorial guidelines
- DownloadDownload
- Share
- Language
- Discussion
In this series:Myelofibrosis
Polycythaemia rubra vera (PRV) is a myeloproliferative disorder, which means the bone marrow makes too many blood cells. It is also sometimes just called polycythaemia (PV). There is an abnormally high number of red blood cells in your blood. You may also have an abnormally high number of platelets and white blood cells.
In this article:
Continue reading below
What is normal blood made up of?
Blood cells, which can be seen under a microscope, make up about 40% of the blood's volume. Blood cells are divided into three main types:
Red cells (erythrocytes). These make blood a red colour. One drop of blood contains about five million red cells. Red cells contain a chemical called haemoglobin. This binds to oxygen and takes oxygen from the lungs to all parts of the body.
White cells (leukocytes). There are different types of white cells, which are called neutrophils (polymorphs), lymphocytes, eosinophils, monocytes and basophils. They are part of the immune system. Their main role is to defend the body against infection.
Platelets. These are tiny and help the blood to clot if we cut ourselves.
Plasma is the liquid part of blood and makes up about 60% of the blood's volume. Plasma is mainly made from water. However, it contains many different proteins and other chemicals, such as hormones, antibodies, enzymes, glucose, fat particles, salts, etc.
When blood spills from your body (or a blood sample is taken into a plain glass tube) the cells and certain plasma proteins clump together to form a clot. The remaining clear fluid is called serum.
The bone marrow, stem cells and blood cell production
Back to contentsHaematopoietic System of the Bone Marrow
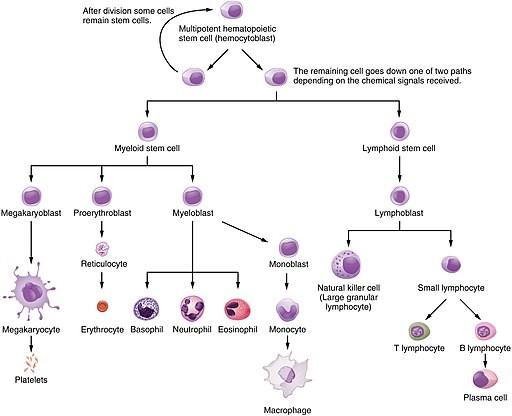
© JulieJenksButteCollege, CC BY-SA 4.0, via Wikimedia Commons
By JulieJenksButteCollege, CC BY-SA 4.0, via Wikimedia Commons
Bone marrow
Blood cells are made in the bone marrow by stem cells. The bone marrow is the soft sponge-like material in the centre of bones. The large flat bones, such as the pelvis and breastbone (sternum), contain the most bone marrow. To make blood cells constantly you need a healthy bone marrow. You also need nutrients from your diet, including iron and certain vitamins.
Stem cells
Stem cells are immature (primitive) cells. There are two main types in the bone marrow - myeloid and lymphoid stem cells. These derive from even more primitive cells called common pluripotent stem cells. Stem cells constantly divide and produce new cells. Some new cells remain as stem cells and others go through a series of maturing stages (precursor or blast cells) before forming into mature blood cells. Mature blood cells are released from the bone marrow into the bloodstream.
Lymphocyte white blood cells develop from lymphoid stem cells. All the other different blood cells (red blood cells, platelets, neutrophils, basophils, eosinophils and monocytes) develop from myeloid stem cells.
Blood production
You make millions of blood cells every day. Each type of cell has an expected lifespan. For example, red blood cells normally last about 120 days. Some white blood cells last just hours or days - some last longer. Every day millions of blood cells die and are broken down at the end of their lifespan. There is normally a fine balance between the number of blood cells that you make and the number that die and are broken down. Various factors help to maintain this balance. For example, certain hormones in the bloodstream and chemicals in the bone marrow, called growth factors, help to regulate the number of blood cells that are made.
Continue reading below
What is polycythaemia rubra vera?
Back to contentsPolycythaemia rubra vera (PRV) is a myeloproliferative disorder, which means the bone marrow makes too many blood cells. In PRV there is an abnormally high number of red blood cells in your blood. This is because the myeloid stem cells in your bone marrow have started to multiply out of control. As these stem cells can develop into either red blood cells, platelets or white blood cells, if you have PRV, you may also have an abnormally high number of platelets and white blood cells.
An abnormally high number of red blood cells is called erythrocytosis. An abnormally high number of platelets is called thrombocytosis. An abnormally high number of white blood cells is called leukocytosis.
Because of the extra number of blood cells circulating if you have PRV, your blood becomes more viscous. This means that it is thicker or more sludgy than normal. This causes your blood to flow more slowly and also causes an increased risk of a blood clot (thrombosis) forming.
What causes polycythaemia rubra vera?
Back to contentsOver 19 in 20 people with PRV have an abnormality (called a mutation) in a protein called the JAK2 protein. The JAK2 protein normally helps to regulate and control the production of blood cells. So, it is thought that the abnormal JAK2 protein is involved in the stem cells starting to multiply out of control in people with PRV. The cause of the JAK2 protein problem may be as a result of some damage to the bone marrow. For example, damage due to a viral infection or due to background radiation. However, more research is needed to find the exact cause.
PRV is one of a group of diseases called myeloproliferative disorders. In all myeloproliferative disorders, there is excessive production of blood cells in the bone marrow for whatever reason. In 2008 the World Health Organization changed the way it classifies these blood conditions. From 2008 PRV has been classified as a myeloproliferative neoplasm - a type of blood cancer.
Continue reading below
How common is polycythaemia rubra vera?
Back to contentsPRV is not very common. It is thought that about 2 in 100,000 people develop PRV each year. PRV can affect people of any age. However, most people are diagnosed at around the age of 60 years.
Polycythaemia rubra vera symptoms
Back to contentsPRV can cause a number of different symptoms or complications (described below). However, not everyone with PRV will have all of these. Some people have only mild symptoms, whilst others may develop one or more complications. Treatment (see below) can help to reduce your chance of developing symptoms and complications.
Symptoms because of sluggish blood flow
The sluggish blood flow means that oxygen (that is carried bound to haemoglobin in your red blood cells) cannot get to the tissues of your body as easily. This can lead to various symptoms, including:
Tiredness.
Ringing in your ears (tinnitus).
Chest pain or pain in your calf muscles when walking.
Blood clots
There is an increased risk of developing a blood clot (thrombosis) if you have PRV. A deep vein thrombosis (DVT) is a blood clot that develops in a deep vein, usually a leg vein. If you develop a DVT, there is also a risk of the blood clot becoming dislodged and travelling through your circulation. Eventually, the clot can become stuck in your lung, causing pulmonary embolisms. If you have PRV and are over the age of 60 years, or you have previously had a DVT, your risk is increased.
If you have PRV, there is also an increased risk of developing a blood clot in an artery blood vessel. This can lead to a heart attack, a stroke or a transient ischaemic attack (TIA, or mini stroke). See the separate leaflets called Heart Attack (Myocardial Infarction), Stroke and Transient Ischaemic Attack for more details. Your risk may be increased further if you have other risk factors for heart attacks and strokes, such as high blood pressure (hypertension), smoking, diabetes or high cholesterol levels.
Bleeding problems
Some people with PRV can develop bleeding problems, including nosebleeds, bleeding gums, bruising or bleeding from their gut.
Other symptoms
People with PRV may have itching of their skin (known as pruritus), particularly after having a bath or a shower. This is due to a chemical called histamine that is released by the high levels of basophil blood cells. You may also notice that your complexion is a bit more ruddy than normal. This is due to the increased numbers of red blood cells. Weight loss can be a problem for some people with PRV. Also, about 1 in 10 people with PRV develop gout.
Myelofibrosis
There is a chance that, after about 15 years, PRV can develop into a condition known as myelofibrosis.
With myelofibrosis, your bone marrow becomes filled with fibrous tissue (a bit like scar tissue). The number of bone marrow cells is greatly reduced and they fail to make enough blood cells.
Therefore, if you have myelofibrosis, the number of red and white blood cells and platelets in your blood becomes too low. (That is, the opposite of what happens in PRV without myelofibrosis.) This can make you more prone to develop infections. You can also develop symptoms of anaemia such as tiredness and breathlessness. Between 6 and 15 in 100 people with PRV will develop myelofibrosis. Blood transfusions may be needed to keep up your red blood cell levels.
Rarely, acute myeloid leukaemia can develop in people with PRV. The risk is increased if you develop myelofibrosis. This risk of acute leukaemia may also be increased a little if certain medicines are taken to help treat PRV (see below).
Polycythaemia rubra vera diagnosis
Back to contentsPRV may be discovered after testing because you are found to have symptoms, or one of the complications described above. However, in some people, it may be discovered because a routine blood test (done for another reason) shows raised levels of red blood cells. Typically, blood tests in someone with PRV show high numbers of red blood cells, raised platelets and raised white blood cell levels, particularly neutrophils.
If your doctor suspects PRV, they may ask about your medical history and may also examine your tummy (abdomen) to look for any signs that your spleen or liver is enlarged. An enlarged spleen is particularly common in people with PRV. High blood pressure (hypertension) is also more common so your doctor may notice this when they examine you. You will usually be referred to a blood specialist (a haematologist) if your doctor suspects that you have PRV.
The specialist may suggest further tests to help confirm the diagnosis. These may include:
A test called a red cell mass study. If you have PRV, your red cell mass will be raised. The test is done by taking a sample of your blood, treating the sample with a weakly radioactive dye and then giving the blood sample back to you. The dyed red blood cells then distribute themselves among your other red blood cells. Another blood sample is then taken and, from this, the laboratory staff are able to calculate the total mass of your red blood cells.
A blood test to look for the abnormal JAK2 protein.
A blood test to check your level of erythropoietin, which is usually low in PRV.
Other blood tests to look at your liver and kidneys and to check your iron and vitamin levels.
A bone marrow biopsy. This is a procedure where a sample of tissue is taken from the inside of a bone. See the separate leaflet called Bone Marrow Biopsy and Aspiration for more details. Certain changes in the bone marrow may be seen if you have PRV.
An ultrasound or CT scan of your tummy (abdomen) to look for an enlarged spleen.
What is the treatment for polycythaemia vera?
Back to contentsThere is no cure for PRV. The aim of treatment is to reduce the risk of you developing symptoms or complications due to PRV. However, as mentioned above, not everyone may develop symptoms or complications. Sometimes it can be difficult for doctors to predict who is likely to develop complications and so what treatment is best.
The treatment options include:
Bloodletting
Bloodletting (venesection) is the main treatment for PRV. Essentially, this reduces the number of red blood cells in your blood and so helps to make your blood thinner (less viscous) so that it circulates better. Venesection is done by removing blood, usually from a vein in your arm, using a needle and syringe - a bit like when someone donates blood. Regular venesection is usually needed if you have PRV, until your red blood cell numbers have reduced and your blood thickness is satisfactory.
Medicines to help slow the production of red blood cells
In many people with PRV, a medicine may also be suggested to help to slow down the production of red blood cells. Some medicines also slow down the production of platelets. The decision about starting such treatment with medicines, and what medicine to use, depends on various things. These include:
Your age.
Your red blood cell count.
How well venesection is working and how well you are managing with this.
What your platelet levels are.
Whether you have already had problems with either blood clots (thromboses) or bleeding.
Various medicines may be considered and they are discussed below. They have different advantages and disadvantages. Your blood specialist (haematologist) will be able to discuss with you the medicine that may be best in your situation. Some medicines can have effects on your fertility and also on a developing baby. Ask your doctor if you have PRV and are considering trying for a baby. This includes both men and women.
Hydroxycarbamide is commonly used in people over the age of 40 years. It used to be known as hydroxyurea. Most people tolerate this medicine well but it may cause some side-effects in some. These include some darkening of your skin pigment, mouth and leg ulcers and digestion or bowel problems. Also, hydroxycarbamide should not be used by pregnant women or someone trying to conceive because it may have effects on both fertility and the developing baby. Some research studies have shown that there is a small chance that hydroxycarbamide increases your risk of developing acute leukaemia if you take the drug for 10-15 years.
Editor’s note
Dr Krishna Vakharia, 24th November 2023
The National Institute for Health and Care Excellence (NICE) has recommended an oral medication called ruxolitinib is for treating polycythaemia vera in adults who cannot tolerate hydroxycarbamide (also called hydroxyurea) or when the condition doesn't respond to it. If this is an option for you, your specialist doctor will discuss it with you.
Interferon can be used in younger people without affecting their fertility and it can also be taken by pregnant women. However, interferon does have a number of side-effects, including hair loss, depression and flu-like symptoms. The chance of PRV developing into myelofibrosis seems to be less in people who take interferon. It also does not seem to increase your risk of acute leukaemia. Interferon is given by injection.
Radioactive phosphorus and busulfan belong to a group of medicines known as alkylating agents. The problem with these medicines is that they may permanently affect your fertility and your bone marrow so they are not generally used in younger people. There is also thought to be a slightly higher risk of developing acute leukaemia if these medicines are used. These medicines are generally used if other medicines are not working to control PRV, or their side-effects are unacceptable for some reason.
Anagrelide is another medicine that is sometimes used if other medicines are not working. It is not known to have an effect on fertility but it cannot be used during pregnancy. Like interferon, anagrelide does not seem to increase the risk of developing acute leukaemia.
Other treatments
A daily low-dose aspirin is usually recommended if you have PRV, unless there is some reason why you may not be able to take this. Aspirin may help to prevent blood clots forming and so also the complications that can result from this. It does not have any effect on the numbers of red blood cells.
Treatment for gout may be needed by some people with PRV. Venesection can help to treat an episode of gout along with some painkillers. For some people, a medicine called allopurinol is recommended to help to prevent attacks of gout.
Itching can be a troublesome problem for some people. Soothing creams may help and sometimes your doctor may be able to prescribe a medicine to help with the itching.
Because of the risk of blood clots forming in your arteries if you have PRV, it is important that you also do all you can to reduce any other risk factors you may have for heart attacks and strokes. These include high blood pressure (hypertension), smoking, diabetes or high cholesterol levels. See the separate leaflet called Cardiovascular Disease (Atheroma) for more details.
What is the outlook for polycythaemia rubra vera?
Back to contentsThe outlook (prognosis) depends on a number of things, including:
Your age.
Any other medical problems or illnesses that you may have.
Any complications of PRV that you may develop.
The most common complication is a blood clot (thrombosis). Your risk of developing a blood clot increases with your age and also increases with the more blood clots that you have had.
Provided that you do not have any other diseases and that you do not develop any complications related to PRV, in particular myelofibrosis or acute myeloid leukaemia, your life expectancy is probably not affected.
Patient picks for Blood problems

Allergies, blood and immune system
Haemochromatosis
Haemochromatosis is an inherited (genetic) disorder which causes the body to absorb too much iron from the diet. This excess iron causes damage to organs in which it builds up. The main treatment is the regular removal of blood which helps to remove the excess iron from the body. If treatment is started early, before complications occur, then the outlook for people with haemochromatosis is very good.
by Dr Philippa Vincent, MRCGP

Allergies, blood and immune system
Thrombophilia
The body has a natural clotting process in the blood, which is altered in thrombophilia. The normal clotting process is called haemostasis.
by Dr Toni Hazell, MRCGP
Further reading and references
- Polycythemia vera, PV; Online Mendelian Inheritance in Man (OMIM)
- Polycythemia Vera Treatment Overview; National Cancer Institute (US)
- Polycythaemia/erythrocytosis; NICE CKS, September 2024 (UK access only)
- Tremblay D, Kosiorek HE, Dueck AC, et al; Evaluation of Therapeutic Strategies to Reduce the Number of Thrombotic Events in Patients With Polycythemia Vera and Essential Thrombocythemia. Front Oncol. 2021 Feb 16;10:636675. doi: 10.3389/fonc.2020.636675. eCollection 2020.
Continue reading below
Article history
The information on this page is written and peer reviewed by qualified clinicians.
Next review due: 25 Feb 2028
26 Feb 2023 | Latest version
25 Nov 2010 | Originally published
Authored by:
Dr Michelle Wright, MRCGP

Ask, share, connect.
Browse discussions, ask questions, and share experiences across hundreds of health topics.

Feeling unwell?
Assess your symptoms online for free
Sign up to the Patient newsletter
Your weekly dose of clear, trustworthy health advice - written to help you feel informed, confident and in control.
By subscribing you accept our Privacy Policy. You can unsubscribe at any time. We never sell your data.