Guillain-Barré syndrome
Peer reviewed by Dr Toni Hazell, MRCGPLast updated by Dr Colin Tidy, MRCGPLast updated 21 May 2025
Meets Patient’s editorial guidelines
- DownloadDownload
- Share
- Language
- Discussion
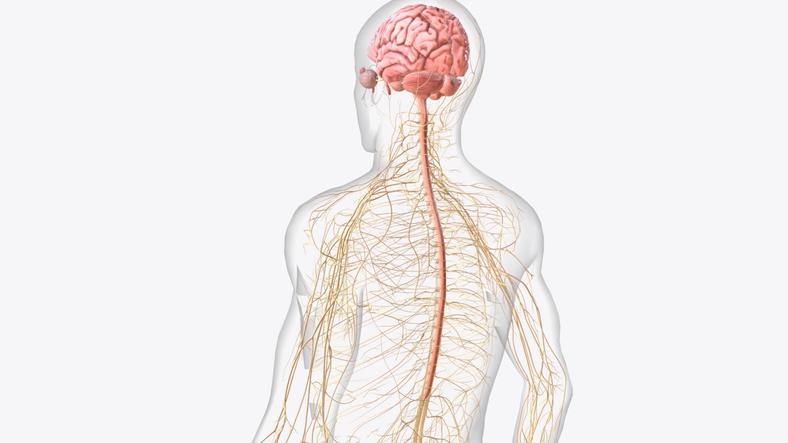
Guillain-Barré syndrome affects the nerves of the limbs and body and is usually triggered by an infection. The main symptom is sudden onset weakness of the muscles that are supplied by the affected nerves. It requires immediate hospital admission as it can rapidly become very serious. With appropriate treatment and monitoring, most people make a full recovery.
In this article:
Continue reading below
What is Guillain-Barré syndrome?
Guillain-Barré syndrome (GBS) is a disease that affects nerves throughout the body and limbs. It is usually triggered by an infection. It is named after Dr Guillain and Dr Barré who were two of the doctors who described this syndrome early in the last century.
Who gets Guillain-Barré syndrome?
Back to contentsGuillain-Barré syndrome is rare but may affect anyone. It occurs more commonly in early adulthood and in the elderly. It is generally more common in males than females but is also more common in women immediately after they have given birth.
Every year about 1,500 people develop GBS in the UK.
Continue reading below
What causes Guillain-Barré syndrome?
Back to contentsMost cases of Guillain-Barré syndrome start within three weeks of an infection. Some of the infections that are known to be related to GBS include:
Campylobacter jejuni (which can cause bowel infection and diarrhoea).
Epstein Barr virus (which causes glandular fever - also called infectious mononucleosis).
Cytomegalovirus (usually causes no symptoms).
Mycoplasma pneumoniae infection (a germ (bacterial) infection that can cause a cough, cold or pneumonia).
HIV.
However, there are probably others. For example, influenza A virus and COVID-19. (Note: the vast majority of people who get these infections do not develop GBS.) GBS has also been reported after certain vaccinations, but this is very rare and much less common than GBS developing after an infection.
Guillain-Barré syndrome is an autoimmune disease. The immune system normally makes small proteins (antibodies) to attack bacteria, viruses, and other germs. In autoimmune diseases, the immune system makes antibodies that can attack and damage the body's own tissues. In GBS, the earlier (preceding) infection stimulates the body to produce antibodies to attack the infecting germ. However, in some people, the antibodies that attack the germ also mistake some of the body's own nerves as germs, because they have similar structures. So the antibodies also attach to, and damage, these nerves, causing inflammation of the nerves, which leads to GBS. If a nerve is damaged, the muscles which that nerve supplies also stop working.
Note: there are various other autoimmune diseases. Most tend to run a persistent (chronic) course once the immune system is triggered - for example, rheumatoid arthritis. However, Guillain-Barré syndrome is different in that the disease activity seems to be time-limited. That is, the immune system reacts to a recent infection which can cause nerve damage, but then settles down again. This is why most people with GBS recover fully.
What are the symptoms of Guillain-Barré syndrome?
Back to contentsMuscle weakness. This starts in the extremities such as the feet and hands and moves upwards towards the centre of the body. The legs are affected more often than the arms. If the nerves in the head, neck and chest are affected, there may be difficulty with swallowing, eye movements and breathing. Reflexes, such as the way the leg moves when the knee is tapped, are also lost early in most people.
Sensory symptoms. These may include tingling/pins and needles or numbness. The symptoms usually begin in the toes and/or the fingertips.
Pain. About 1 in 2 people with Guillain-Barré syndrome develop either nerve pain or deep aching muscle pain. This tends to be worse with movement and at night.
Autonomic symptoms. The autonomic nervous system (part of the peripheral nervous system) is responsible for body functions like sweating, breathing, the heart beating and digestion. In GBS, nerves within this system may be affected, causing problems with blood pressure, pulse, vision and lack of sweating.
Continue reading below
How does Guillain-Barré syndrome progress?
Back to contentsUsually, the weakness and sensory symptoms become worse and spread up the body. Symptoms typically peak in severity 1-4 weeks after first starting. The severity of symptoms and when they peak can vary from person to person. However, symptoms can often be severe. In many cases, both arms and legs become so weak that they cannot be used at all.
In some cases, the weakness does not progress much further than the lower legs. This may cause some moderate difficulty in walking, which may require a walking stick.
Once symptoms peak, they tend to remain in a stable level (plateau) phase for a while. Typically, this lasts for several days but, again, can be variable. Then the symptoms gradually start to ease off as the damaged nerves begin to heal. The time it takes to recover varies greatly from person to person; however, it is often several months.
How is Guillain-Barré syndrome diagnosed?
Back to contentsExamination. Guillain-Barré syndrome is usually first suspected after an examination by a doctor. This usually reveals weakness in the arms and legs, absent reflexes, and mild numbness. The signs are usually equal on both sides of the body.
Cerebrospinal fluid (CSF) sample. This is the fluid that surrounds your spinal cord and brain. A sample of this is collected through a needle in your back. It will usually show a high amount of protein and not very many white blood cells (blood cells that increase in infection) if you have GBS.
Electrodiagnostic tests. These are tests of the electrical activity of your nerves and will usually show a typical pattern in GBS.
Other tests may also be suggested. These include:
A test to show how well you breathe in and out (spirometry).
A tracing of the electrical activity of your heart (electrocardiogram, or ECG).
These can help to check for complications of GBS and to monitor progress.
What is the treatment for Guillain-Barré syndrome?
Back to contentsIf your doctor suspects Guillain-Barré syndrome, you will be sent to hospital immediately. This is because the disease may progress quickly within a few days, to affect your breathing and heart. You need to be monitored closely in hospital so that these complications can be treated quickly if they occur. Good supportive care is the most important part of treatment. For example, you may need help and support with feeding and breathing until the symptoms ease.
Some specific treatments that may be given include one or more of the following:
Immunoglobulin
Immunoglobulin is an antibody that is present in blood and is collected from blood given by blood donors. It is given as an injection directly into a vein. The precise way that it works is not clear. It may work to alter your immune system and help to clear the abnormal proteins (antibodies). It is thought that the sooner treatment is started after symptoms begin, ideally within two weeks, the better the effect this treatment is likely to have.
Plasma exchange
Your blood is made up of blood cells and a fluid called plasma. Plasma is where the damaging antibodies are present. Plasma exchange involves taking your blood out of your body and separating the blood into cells and plasma. The plasma is then taken away and the blood cells are returned to the body with a plasma substitute. A special machine is used for this treatment and only a small amount of blood is actually outside the body at any time. Again, the sooner treatment is started after symptoms begin, the better the effect this treatment is likely to have.
However, plasma exchange is done less commonly these days, because treatment with immunoglobulin is easier to give, seems to cause fewer side-effects, and has been shown to be just as effective.
Artificial ventilation
In about 1 in 3 cases, the muscles of the chest become so weak that breathing is affected. If this occurs, you will need support to breathe with a breathing machine (ventilator) in an intensive care unit (ICU).
Other supportive care
Swallowing may be affected and you may need to be fed via a tube passed into your stomach (nasogastric tube).
Deep vein thrombosis (DVT) prevention
You will usually be given special stockings to wear and blood-thinning (heparin) injections to try to prevent blood clots in your leg (DVT) which may occur as a result of being immobile.
Pain relief
This may be with particular medicines that work well for nerve-related pain.
Physiotherapy and occupational therapy
These may also be helpful treatments for Guillain-Barré syndrome. Physiotherapy may help build up strength and prevent or treat muscle stiffness that may develop. It may also help with pain relief. Occupational therapists help people maximise their daily functioning as part of a rehabilitation team.
Support and counselling
Low mood can be a problem for people with Guillain-Barré syndrome. You may find it helpful to talk through some of your feelings with a counsellor and to get support from them.
A note about steroids
In general, steroids are not thought to help much in the treatment of Guillain-Barré syndrome, and may even delay recovery, so they are not routinely used.
Does Guillain-Barré syndrome go away?
Back to contentsDue to improvements in treating Guillain-Barré syndrome, around 7-8 in 10 people recover in 6-12 months. However, you may be in hospital for a few months. About 2 in 10 people with GBS will be left with some degree of problems long-term, such as some weakness, muscle wasting, difficulty walking or pain. Between 1 in 30 and 1 in 10 people with GBS will die. This is usually due to severe breathing problems, problems with the rhythm of the heart, or infections. (You are more prone to infections if you become immobile.)
It is rare to have GBS a second time.
If you have a relative or friend in hospital with severe Guillain-Barré syndrome you will inevitably be very worried by what is happening. But remember: even total paralysis due to GBS is compatible with total recovery.
Patient picks for Limb weakness and numbness

Brain and nerves
Multiple sclerosis
Multiple sclerosis is a disorder of the brain and spinal cord. It can cause various symptoms. In most cases, episodes of symptoms come and go for several years. In time, some symptoms can become permanent and can cause disability. Although there is no cure for multiple sclerosis, various medicines and therapies may reduce the number of flare-ups and can help to ease symptoms and disability.
by Dr Hayley Willacy, FRCGP
Brain and nerves
Motor neurone disease
Motor neurone disease (MND) is a neurological condition causes a progressive weakness and wasting of many of the muscles in the body. There are various types of motor neurone disease. This leaflet is mainly about amyotrophic lateral sclerosis (ALS), which is the most common type of motor neurone disease. Although there is no cure for motor neurone disease, treatments can help to ease symptoms and disability.
by Dr Rachel Hudson, MRCGP
Further reading and references
- Bellanti R, Rinaldi S; Guillain-Barre syndrome: a comprehensive review. Eur J Neurol. 2024 Aug;31(8):e16365. doi: 10.1111/ene.16365. Epub 2024 May 30.
- Leonhard SE, Mandarakas MR, Gondim FAA, et al; Diagnosis and management of Guillain-Barre syndrome in ten steps. Nat Rev Neurol. 2019 Nov;15(11):671-683. doi: 10.1038/s41582-019-0250-9. Epub 2019 Sep 20.
- Hughes RA, Brassington R, Gunn AA, et al; Corticosteroids for Guillain-Barre syndrome. Cochrane Database Syst Rev. 2016 Oct 24;10:CD001446.
- Hughes RA, Swan AV, van Doorn PA; Intravenous immunoglobulin for Guillain-Barre syndrome. Cochrane Database Syst Rev. 2014 Sep 19;(9):CD002063. doi: 10.1002/14651858.CD002063.pub6.
- Chevret S, Hughes RA, Annane D; Plasma exchange for Guillain-Barre syndrome. Cochrane Database Syst Rev. 2017 Feb 27;2:CD001798. doi: 10.1002/14651858.CD001798.pub3.
Continue reading below
Article history
The information on this page is written and peer reviewed by qualified clinicians.
Next review due: 20 May 2028
21 May 2025 | Latest version

Ask, share, connect.
Browse discussions, ask questions, and share experiences across hundreds of health topics.

Feeling unwell?
Assess your symptoms online for free
Sign up to the Patient newsletter
Your weekly dose of clear, trustworthy health advice - written to help you feel informed, confident and in control.
By subscribing you accept our Privacy Policy. You can unsubscribe at any time. We never sell your data.