Bowel polyps
Colonic polyps
Peer reviewed by Dr Colin Tidy, MRCGPLast updated by Dr Toni Hazell, MRCGPLast updated 15 Sept 2023
Meets Patient’s editorial guidelines
- DownloadDownload
- Share
- Language
- Discussion
- Audio Version
In this series:Bowel cancerBowel cancer screeningFaecal immunochemical testSigmoidoscopyColonoscopyCT colonography
Bowel polyps (colonic polyps) are small non-cancerous (benign) growths on the inside lining of the bowel (colon and rectum).
In this article:
Video picks for Bowel problems
Continue reading below
What are bowel polyps?
A bowel polyp is a small non-cancerous growth. There are many types of polyps, such as those that occur in the nose - this leaflet is about polyps that occur in the bowel.
Types of bowel polyps
Back to contentsLarge bowel - polyp
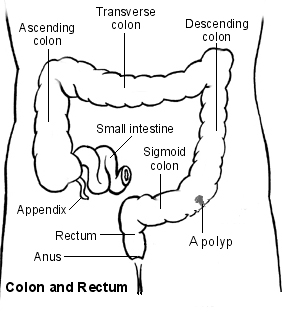
Most bowel polyps develop in the part of the colon called the descending colon, which leads down to the rectum. However, they can occur anywhere in the colon or rectum. Bowel polyps can be divided into three types: hyperplastic polyps, adenomas and polyposis syndromes.
Hyperplastic bowel polyps
These are a common type of bowel polyps. They are small - usually less than half a centimetre in diameter. They are generally regarded as harmless and only very rarely turn into cancer.
Adenomas
These too are a common type of bowel polyp. Most are small (usually less than a centimetre in diameter) but they can be bigger. There is a small risk that an adenoma may, in time, become cancerous. If one does turn cancerous, the change usually takes place after a number of years.
The relationship between polyps and cancer is that most bowel cancers (colorectal cancers) develop from a polyp that has been present for 5-15 years. In other words, although most adenomas do not become cancerous, the vast majority of cancers in the bowel initially develop from an adenoma that has been present for a number of years.
It is difficult to be certain of the exact risk of developing cancer from an adenoma. One study suggested that for a single 1 cm adenoma, the risk of it turning cancerous was about 1 in 12 after 10 years, and about a 1 in 4 after 20 years. However, the risk seems to vary depending on factors such as the size of the adenoma and the exact type of adenoma.
There are different types of adenoma and some types are more likely than others to develop into bowel cancer. See also the separate leaflet on Bowel Cancer Screening.
Polyposis syndromes
Polyposis syndromes are a group of inherited conditions. They include:
Familial adenomatous polyposis (FAP).
Hereditary nonpolyposis colorectal cancer (HNPCC)/Lynch's syndrome.
Gardner's syndrome.
Turcot's syndrome.
Peutz-Jeghers syndrome.
Cowden's disease.
Familial juvenile polyposis.
Hyperplastic polyposis.
These are rare syndromes. They cause polyps in young people and often cause multiple bowel polyps that have a high chance of developing into bowel cancer.
Continue reading below
Bowel polyp symptoms
Back to contentsMost people with one or more bowel polyps do not have any symptoms. Most people who have a bowel polyp will never know they have one.
However, some people with bowel polyps will get symptoms. Polyps do not usually cause abdominal pain or a change in bowel habits. Symptoms include:
Blood in the stools (faeces). There may also be mucus in the stools.
Diarrhoea or constipation, but this is much less likely than blood in the stools. Diarrhoea or constipation is much more likely to have a cause other than a bowel polyp.
Causes of bowel polyps
Back to contentsThe lining of the bowel constantly renews itself throughout our lives. New cells are made in the lining of the bowel and these cells eventually die to be replaced by more new cells. Each of these cells contains genes which control how the cell works.
Family history may play a role, because if the gene doesn't work properly then some cells may grow more quickly. This may eventually cause a polyp to develop. Some faulty genes cause a tendency for the lining of the bowel to develop polyps or bowel cancer, which may be inherited from our parents.
Continue reading below
How common are bowel polyps?
Back to contentsBowel polyps are really common in older people. About 1 in 4 people over the age of 50 years develop at least one colonic polyp. Bowel polyps are much less common in younger people.
Some people develop just one bowel polyp. It is not uncommon to have two or more. However, having more than five polyps is unusual.
Risk factors
Risk factors include increasing age, being overweight and smoking. If you have a family history of a bowel polyp or cancer, or have had either of these yourself in the past, you are also at higher risk. Another risk factor is having inflammatory bowel disease (ulcerative colitis or Crohn's disease).
Diagnosing bowel polyps
Back to contentsMost bowel (colonic) polyps do not cause symptoms. So, most people with bowel polyps will not be diagnosed. Screening tests may be done if you have symptoms that indicate a bowel problem, or for various other reasons. For example, if you have seen blood in your stools (faeces) or if you are found to have blood in your stools following a routine screening test which is now offered to older people.
See the separate leaflet called Faecal Occult Blood Test for more details.
What is a colonoscopy?
Most bowel polyps are diagnosed by this procedure. Colonoscopy is a test where an operator - a doctor or a nurse - looks into your colon. A colonoscope is a thin, flexible telescope. It is about as thick as a little finger. It is passed through the anus and into the colon. It can be pushed all the way around the colon as far as the caecum (where the small and large intestine meet). The colonoscope contains fibre-optic channels which allow light to shine down so the operator can see inside your colon.
See the separate leaflet called Colonoscopy for more details.
A sample (biopsy) will be taken at the time of the colonoscopy. This is very important so that it can be checked whether the polyp is cancerous (malignant).
What about other tests?
Sometimes a bowel polyp is diagnosed by other tests:
A special X-ray test of the bowel - this procedure is called a barium enema.
A CT colonogram - air and a contrast dye are pumped into the bowel to make the anatomy clearer to see and you are then examined by a CT scanner.
A test procedure called sigmoidoscopy - this enables a doctor or nurse to use an instrument called a sigmoidoscope to look into the rectum and sigmoid colon. The procedure is similar to a colonoscopy but it uses a shorter telescope.
If a bowel polyp is seen on a barium enema or CT colonogram you will still need a colonoscopy to remove the polyp and to take a sample (biopsy) of it for further investigation. The advantage of a colonoscopy as the first test is that the biopsy can be taken and/or the polyp removed all at the same time.
You will also need a colonoscopy if a polyp is found when you have a sigmoidoscopy. This is to make sure there are no more polyps beyond the reach of sigmoidoscopy.
Treatments for bowel polyps
Back to contentsIf you are diagnosed with a bowel polyp, you will usually be advised to have it removed, even if it is not causing any symptoms. This is because there is a small risk of the polyp developing into a cancerous (malignant) growth at some time in the future.
Colonoscopy
Most bowel polyps can be removed during a colonoscopy. The colonoscope has a side channel down which a grabbing device can be passed. This device can be manipulated by the operator. The operator can therefore see and also remove a polyp during a colonoscopy. The removal of the polyp is usually painless. Once removed, the bowel/colon polyp is sent to the laboratory to be looked at under a microscope. This is done to check:
That it has been completely removed.
The type of polyp.
Whether it is non-cancerous (benign) or showing signs of cancerous (malignant) change.
Most removed polyps will show full removal and be totally benign.
Your consultant will advise on the need for follow-up. This may depend on factors such as the size of the bowel polyp, the exact type of polyp that has been removed, the laboratory report about the polyp, and your age. Once these factors are considered, some people are advised to have regular colonoscopies in the future to make sure no more bowel polyps develop. As with any test, the results should be given to you by the team who arranged the test. So if you are not sure about how to access the results, phone or email your consultant's secretary, not your GP.
Surgery
If you have many bowel polyps (especially if you have a polyposis syndrome) then you may need to have an operation to remove part of your bowel. This is because it isn't possible to completely remove all the bowel polyps by using colonoscopy.
Preventing bowel polyps
Back to contentsPolyps cannot be prevented, but a healthy lifestyle (not smoking and not being overweight) can help to reduce your risk.
Patient picks for Bowel problems

Digestive health
Duodenal ulcer
A duodenal ulcer is usually caused by an infection with a germ (bacterium) called Helicobacter pylori (H. pylori). A 4- to 8-week course of acid-suppressing medication will allow the ulcer to heal. In addition, a one-week course of two antibiotics plus an acid-suppressing medicine will usually clear the H. pylori infection. This usually prevents the ulcer from coming back. Anti-inflammatory medicines used to treat conditions such as arthritis sometimes cause duodenal ulcers. It would be very unusual for a person with a known duodenal ulcer to be given anti-inflammatory medication, but if there is absolutely no alternative then it may be given with long-term acid-suppressing medication.
by Dr Toni Hazell, MRCGP

Digestive health
Ulcerative colitis
Ulcerative colitis is a disease where inflammation develops in the colon and the rectum (the large intestine). The most common symptom when the disease flares up is diarrhoea mixed with blood. Treatment can usually ease a flare-up of symptoms. The disease can often be prevented from flaring up by taking medication, usually mesalazine, each day. Surgery to remove the colon is needed in some cases.
by Dr Colin Tidy, MRCGP
Further reading and references
- Combined endoscopic and laparoscopic removal of colonic polyps; NICE Interventional procedures guidance, September 2014
- Colorectal cancer (management in people aged 18 and over); NICE Guidance (2020, last updated December 2021)
- Bowel screening; NICE CKS, May 2019 (UK access only)
- Bonnington SN, Rutter MD; Surveillance of colonic polyps: Are we getting it right? World J Gastroenterol. 2016 Feb 14;22(6):1925-34. doi: 10.3748/wjg.v22.i6.1925.
Continue reading below
Article history
The information on this page is written and peer reviewed by qualified clinicians.
Next review due: 13 Sept 2028
15 Sept 2023 | Latest version

Ask, share, connect.
Browse discussions, ask questions, and share experiences across hundreds of health topics.

Feeling unwell?
Assess your symptoms online for free
Sign up to the Patient newsletter
Your weekly dose of clear, trustworthy health advice - written to help you feel informed, confident and in control.
By subscribing you accept our Privacy Policy. You can unsubscribe at any time. We never sell your data.