Rectal bleeding
Blood in stool
Peer reviewed by Dr Colin Tidy, MRCGPLast updated by Dr Doug McKechnie, MRCGPLast updated 25 Jun 2024
Meets Patient’s editorial guidelines
- DownloadDownload
- Share
- Language
- Discussion
- Audio Version
In this series:Rectal bleeding in childrenPilesAnal fissureIntussusception and volvulus in childrenLocal preparations for anal disorders
There are many causes of rectal bleeding (bleeding from your bottom). The severity can vary from mild bleeding (common) to a severe life-threatening bleeding (uncommon). If the bleeding is heavy or if you have black stools (faeces) - older blood due to a bleed from high up in the gut - then see a doctor immediately or call an ambulance. However, rectal bleeding is usually a mild bleed. In this situation, make an appointment with your doctor so that the cause can be found.
In this article:
Video picks for Anal and rectal problems
Continue reading below
What is rectal bleeding?
The term rectal bleeding is used by doctors to mean any blood that is passed out of your bottom when you go to the toilet to pass stools (faeces). However, not all bleeding that is passed out actually comes from the back passage (rectum). The blood can come from anywhere in the gut. The more correct term is gastrointestinal tract bleeding, often abbreviated to GI bleeding. There are many causes of rectal bleeding (GI bleeding) which are discussed later.
What is the gut?
The gut (gastrointestinal tract) starts at the mouth and ends at the anus. When we eat or drink, the food and liquid travel down the gullet (oesophagus) into the stomach. The stomach starts to break up the food and then passes it into the small intestine.
The small intestine (sometimes called the small bowel) is several metres long and is where food is digested and absorbed. Undigested food, water and waste products are then passed into the large intestine (sometimes called the large bowel). The main part of the large intestine is called the colon, which is about 150 cm long.
This is split into four sections: the ascending (on the right side of your tummy), transverse (across the top of your tummy), descending (on the left side of your tummy) and sigmoid colon (in your pelvis). Some water and salts are absorbed into the body from the colon. The colon leads into the back passage (rectum) which is about 15 cm long. The rectum stores stools (faeces) before they are passed out from the anus.
How common is rectal bleeding?
Back to contentsRectal bleeding is common. Studies suggest that about 15% of all people have experienced rectal bleeding in the last year.
Continue reading below
What causes rectal bleeding?
Back to contentsThere are many possible causes. Below is a brief overview of the more common causes:
Piles
Piles (haemorrhoids) are swellings that can occur in the anus and lower back passage (lower rectum). There is a network of small blood vessels (veins) within the inside lining of the anus and lower rectum. These veins sometimes become wider and filled with more blood than usual. These swollen (engorged) veins and the overlying tissue may then form into one or more small swellings called haemorrhoids. External haemorrhoids develop under the skin around the anus, and internal haemorrhoids form inside the rectum (the back passage).
Haemorrhoids are very common and many people develop one or more haemorrhoids at some stage. Small haemorrhoids are usually painless. The most common symptom is bleeding after going to the toilet. Larger haemorrhoids may cause a mucous discharge, some pain, irritation and itch.
Anal fissure
An anal fissure is a small tear of the skin of the anus. Although the tear of an anal fissure is usually small (usually less than a centimetre), it can be very painful because the anus is very sensitive. Often an anal fissure will bleed a little. You may notice blood after you pass stools (faeces). The blood is usually bright red and stains the toilet paper but soon stops.
Diverticula
A diverticulum is a small pouch in the wall of the gut (intestines). Diverticula is the word used for more than one diverticulum. They can develop on any part of the gut but usually occur in the colon. Several diverticula may develop over time.
A diverticulum may occasionally bleed and you may pass some blood via your anus. The bleeding is usually abrupt and painless. The bleeding is due to a burst blood vessel that can happen in the wall of a diverticulum and so the amount of blood loss can be heavy. Diverticula can cause other symptoms such as tummy pains and changes in your normal bowel habit.
Crohn's disease
Crohn's disease is a condition which causes the gut to become inflamed. The disease flares up from time to time. Symptoms vary, depending on the part of the gut affected and how bad the condition is. Common symptoms include bloody diarrhoea, tummy (abdominal) pain and feeling unwell. See the separate leaflet called Crohn's disease for details.
Ulcerative colitis and other forms of colitis
Ulcerative colitis (UC) is a disease where inflammation develops in the colon and rectum. A common symptom when the disease flares up is diarrhoea mixed with blood. The blood comes from ulcers that develop on the lining of the inflamed gut. There are other rare causes of inflammation of the colon (colitis) or inflammation of the rectum (proctitis) that can cause rectal bleeding. See the separate leaflet called Ulcerative colitis for details.
Polyps
A bowel polyp is a small growth that sometimes forms on the inside lining of the colon or rectum. Most develop in older people. Polyps are non-cancerous (benign) and usually cause no problems. However, sometimes a polyp bleeds and sometimes a polyp can turn cancerous. See the separate leaflet called Bowel polyps (Colonic polyps) for details.
Colon cancer
Cancer of the colon and rectum are common cancers in older people. They sometimes affect younger people. Rectal bleeding is one symptom that may occur. Bleeding is often not visible (occult - see later) and other symptoms are often present before visible bleeding occurs. For example, weight loss, tiredness due to blood loss (anaemia), diarrhoea or constipation. Cancers of other parts of the gut higher up from the colon sometimes cause rectal bleeding but these are uncommon. See the separate leaflet called Bowel cancer for details.
Angiodysplasia
Angiodysplasia is a condition where you develop a number of enlarged blood vessels within the inner lining of the colon. Angiodysplasia most commonly develops in the ascending (right) colon, but they can develop anywhere in the colon. The cause is unknown but they occur most commonly in older people.
Bleeding from an angiodysplasia is painless. The blood seen can range from bright red brisk bleeding, to dark blood mixed with faeces, to black- or plum-coloured faeces (melaena). An angiodysplasia may also cause non-visible (occult) blood loss (see below).
Abnormalities of the gut
In young children various abnormalities of the gut or the gut wall may cause rectal bleeding. Examples include:
Volvulus - a twisting of the gut.
Intussusception - one part of the gut is sucked into another, creating a blockage.
Meckel's diverticulum - an extra bulge or pouch in the small intestine, present from birth (congenital).
Hirschsprung's disease - a condition where a part of the lower bowel does not function as it should. The muscles of the bowel wall are unable to squeeze along the faeces as they should do.
Abnormal blood vessel development.
Stomach and duodenal ulcers
An ulcer in the stomach or duodenum may bleed. This can cause melaena, where your faeces turn black- or plum-coloured as described earlier.
There are separate leaflets on both of these conditions, called Stomach ulcer (Gastric ulcer) and Duodenal ulcer.
Some gut infections
These may cause bloody diarrhoea due to inflammation of the gut, caused by some infections.
See the separate leaflet called Gastroenteritis for more information.
There are various other rarer causes.
When should I worry about rectal bleeding?
Back to contentsWhen you have GI bleeding, the things that a doctor needs to assess include the following:
How bad (severe) the bleeding is
Bleeding can range from a mild trickle to a massive life-threatening severe bleed (haemorrhage). In most cases the bleed is mild and intermittent. In this situation, any tests that need to be done can be done as an outpatient. There is no immediate risk to life with mild, intermittent GI bleeding. However, always report to a doctor if you have a large amount of bleeding, as a lot of blood loss needs urgent treatment.
Sometimes bleeding from a condition in the gut (GI tract) is so mild (like a slight trickle) that you do not notice any actual bleeding and it is not enough to change the colour of your stools (faeces). However, a test of your faeces can detect even small amounts of blood. This test may be done in various situations (described later).
Where the bleeding is coming from
Bleeding can come from anywhere in the GI tract. As a general rule:
Bleeding from the anus or low down in the back passage (rectum) - the blood tends to be bright red and fresh. It may not be mixed in with faeces but instead you may notice blood after a bowel movement, or streaks of blood covering faeces. You might also notice blood in the toilet bowl. For example, bleeding from an anal tear (fissure) or from haemorrhoids.
Bleeding from the colon - often the blood is mixed up with faeces. The blood may be a darker red. For example, bleeding from colitis, diverticular disease, or from a bowel tumour. However, sometimes, if the bleeding is brisk then you may still get bright red blood not mixed up too much with faeces. For example, if you have a sudden large bleed from a diverticulum.
Bleeding from the stomach or small intestine - the blood has far to travel along the gut before it is passed out. During the time it takes to do this the blood changes and becomes dark red and mixed with faeces. This can make your faeces turn a black and tarry or plum colour - this is called melaena. For example, this may occur due to a bleeding stomach ulcer or a duodenal ulcer. Note: if you have melaena it is a medical emergency, as it usually indicates a lot of bleeding that is coming from the stomach or duodenum. You should tell a doctor immediately if you suspect that you have melaena.
The cause of the bleeding
A doctor may ask various questions to get a good idea as to the main possible causes of the bleeding. So, for example, you may be asked about possible symptoms. You may be asked about:
Whether you have any pain.
If you have any pain, where it is and what type of pain it is.
Any itching around your bottom.
Any change in your bowels, such as diarrhoea or constipation.
Any weight loss.
Whether you have been feeling unusually tired.
Any history in your family of bowel disease.
Any medications you take, as some can increase the risk of GI bleeding.
The doctor is then likely to examine you. This may include examining your back passage (anus and rectum) by inserting a lubricated gloved finger into your anus. Sometimes they may use an instrument called a proctoscope to look a little way inside your back passage. Sometimes, a diagnosis can be made after this. For example, of an anal fissure or pile (haemorrhoid).
However, further tests are commonly needed to clarify the cause. This is because the examining finger or the proctoscope can only go a short way up your GI tract. If no cause is found, the bleeding may be coming from higher up.
Continue reading below
What should I do if I have rectal bleeding?
Back to contentsSee a doctor. If the bleeding is heavy, or if you have black- or plum-coloured stools (faeces) - called melaena (described above), see a doctor immediately or call an ambulance. If you feel dizzy, collapse or feel generally unwell then consider calling an ambulance, as this might indicate a heavy bleed. However, often the bleeding is mild. In this situation, make an appointment with your doctor soon.
Some people assume that their rectal bleeding is due to piles (haemorrhoids) and do not get it checked out. Haemorrhoids are perhaps the most common cause of rectal bleeding. However, you should not assume the bleeding is coming from a haemorrhoid unless you have been properly assessed by a doctor.
What tests might be advised?
Back to contentsIt depends on the possible causes of the bleeding. This will be determined by a doctor talking to you (your history) and examining you. You will often have a blood test (for anaemia) and usually one of the following tests is suggested:
Sigmoidoscopy.
Colonoscopy.
A virtual colonoscopy (CT colonography).
Colonoscopy new
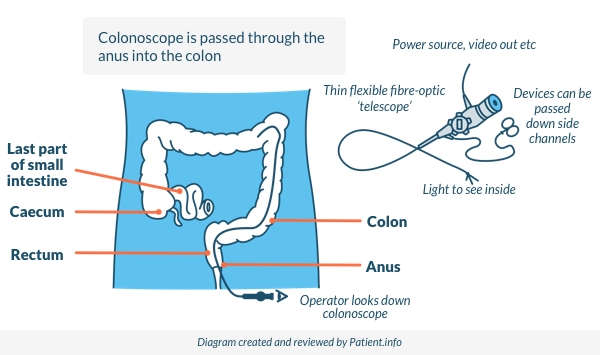
What is a colonoscopy?
A colonoscopy is a test where a doctor or nurse looks into your colon using a colonoscope. A colonoscope has fibre-optic channels that light up the inside of the colon. It is also possible to take a small sample (biopsy) using a colonoscope and sometimes to treat the cause of the rectal bleeding.
What is a sigmoidoscopy?
A sigmoidoscopy is a test that allows a doctor or nurse to look inside the rectum and sigmoid colon. The sigmoid colon is the final portion of the bowel that is joined to the rectum. A sigmoidoscope is similar to a colonoscope but much shorter. A sigmoidoscopy is quicker and easier to do than a colonoscopy, but doesn't assess as much of the gut.
What is a virtual colonoscopy?
A virtual colonoscopy (also called CT colonography) is a newer test. It uses a CT scanner to produce detailed pictures of the inside of the colon. It is usually used for people who are more frail and cannot tolerate a colonoscopy. It is not possible to have a sample (biopsy) taken during a virtual colonoscopy.
What is a FIT kit used for?
Back to contentsFaecal immunochemical testing (FIT) detects small amounts of blood in your stools (faeces) which you would not normally see or be aware of. Testing using the FIT kit has replaced the older 'guaiac' faecal occult blood test (FOBT).
When and why is testing using the FIT kit done?
Testing with the FIT kit is used to look for 'serious' gut problems, to help determine who should be offered an urgent colonoscopy.
The test detects tiny amounts of blood in poo that can't be seen with the naked eye. The tests can be used to look for blood in people with symptoms like persistent diarrhoea, weight loss, anaemia, or persistent tummy (abdominal) pain. Surprisingly, testing using the FIT kit is also useful even in people with visible rectal bleeding, as a normal (negative) FIT result makes it unlikely that there is a serious cause of visible bleeding.
FIT is used:
As a screening test, to look for bowel cancer in people who don't have any symptoms.
To help to decide who should have further investigation (such as a colonoscopy), amongst people with symptoms of a gut problem (including rectal bleeding).
A positive FIT result doesn't necessarily mean that something is wrong, but will usually lead to further urgent tests - likely a colonoscopy - to look for bowel cancer and other gut problems.
How is testing using the FIT kit done?
FIT is a special test kit. You use a stick provided in the sample kit to collect a sample of poo, and then put this stick back into the sample bottle. You then return it, either in the post or to your doctor, depending on the instructions.
In a laboratory, the poo sample is tested using antibodies which measure the amount of blood in the sample.
Screening for bowel cancer
Screening means looking for early signs of a particular disease in otherwise healthy people who do not have any symptoms and when treatment is likely to be curative. Bowel cancer (colorectal cancer) screening aims to detect colorectal cancer at an early stage when there is a good chance that treatment will cure the cancer.
In the UK there is a screening programme for certain age groups. This involves testing three samples of your faeces for blood. The age group is slightly different in different parts of the UK. If you are in the relevant age groups, you will automatically be sent an invitation and then your FIT screening kit, so you can do the test at home. After your first screening test, you will then be sent another invitation and screening kit every two years until you reach the maximum age. You can then request further kits if you would like to continue to be included in the screening programme.
What to do about rectal bleeding
Back to contentsSee a doctor if you have rectal bleeding. The treatment depends on the cause; for example, stool softeners can help haemorrhoids and an anal fissure. See individual leaflets on the various diseases that can cause rectal bleeding and the medical treatments to help them.
Patient picks for Anal and rectal problems
Digestive health
Piles
Piles (haemorrhoids) are swollen lumps in or around the bottom that cause discomfort, itching, or bleeding. They often get better on their own but may need treatment to remove them.
by Dr Toni Hazell, MRCGP

Digestive health
Anal fissure
An anal fissure is a small tear in the lining of the skin around the back passage (anus). An anal fissure that lasts more than six weeks is called a chronic anal fissure. For most people, the anal fissure heals quite quickly but some form of treatment is often needed. Anal fissures may keep coming back.
by Dr Hayley Willacy, FRCGP
Further reading and references
- Suspected cancer: recognition and referral; NICE guideline (2015 - last updated January 2026)
- Gastrointestinal tract (lower) cancers - recognition and referral; NICE CKS, August 2023 (UK access only)
- Haemorrhoids; NICE CKS, July 2021 (UK access only)
- Monahan KJ, Davies MM, Abulafi M, et al; Faecal immunochemical testing (FIT) in patients with signs or symptoms of suspected colorectal cancer (CRC): a joint guideline from the Association of Coloproctology of Great Britain and Ireland (ACPGBI) and the British Society of Gastroenterology (BSG). Gut. 2022 Jul 12;71(10):1939-62. doi: 10.1136/gutjnl-2022-327985.
Continue reading below
Article history
The information on this page is written and peer reviewed by qualified clinicians.
Next review due: 25 Jun 2027
25 Jun 2024 | Latest version

Ask, share, connect.
Browse discussions, ask questions, and share experiences across hundreds of health topics.

Feeling unwell?
Assess your symptoms online for free
Sign up to the Patient newsletter
Your weekly dose of clear, trustworthy health advice - written to help you feel informed, confident and in control.
By subscribing you accept our Privacy Policy. You can unsubscribe at any time. We never sell your data.