Chondrodermatitis nodularis
Peer reviewed by Dr Hayley Willacy, FRCGP Last updated by Dr Colin Tidy, MRCGPLast updated 10 Feb 2023
Meets Patient’s editorial guidelines
- DownloadDownload
- Share
- Language
- Discussion
Medical Professionals
Professional Reference articles are designed for health professionals to use. They are written by UK doctors and based on research evidence, UK and European Guidelines. You may find one of our health articles more useful.
In this article:
Synonyms: chondrodermatitis nodularis helicis (or antihelicis - depending on the site of the lesion); chondrodermatitis nodularis chronica helicis; ear pressure sore; painful nodule of the ear; Winkler's disease
This is a painful, inflamed nodule of the ear, involving the cartilage and skin of the pinna. It is usually located at the apex of the helix.
Chondrodermatitis nodularis causes (aetiology)1
It is probably caused mainly by pressure, combined with the anatomy of the pinna and its blood supply:
The initial damage may be triggered by inflammation, oedema and necrosis from trauma, cold, actinic damage or pressure.
The pinna has relatively little subcutaneous tissue for insulation and padding. Only small dermal blood vessels supply the epidermis, dermis, perichondrium and cartilage. These features may prevent adequate healing and lead to secondary perichondritis.
Possibly, perichondrial arteriolar changes may be involved. An autoimmune aetiology has also been implicated.2
How common is chondrodermatitis nodularis? (Epidemiology)3
Back to contentsThe condition is probably relatively common but is rarely documented in the literature. It is most common in elderly men but It affects those of all ages, gender and pigmentation.
Data suggest that the condition is likely to be localised to the helix in men and the antihelix (the curved raised ridge of cartilage in front of the helix) in women.
Anything that puts pressure on the external ear, such as headphones, may precipitate the condition, as may a tendency always to sleep on the same side.
Antihelix position
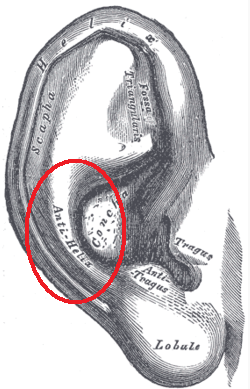
© Mikael Häggström, Public domain, via Wikimedia Commons
By Mikael Häggström, Public domain, via Wikimedia Commons
Continue reading below
Chondrodermatitis nodularis symptoms4
Back to contentsHistory:
It presents as a painful nodule on the helix or antihelix of the ear.
It appears spontaneously and then usually enlarges rapidly to its maximum size and remains stable. Onset may be precipitated by pressure, trauma or cold.
Chondrodermatitis nodularis of the ear

© Klaus D. Peter, Wiehl, Germany,CC BY 3.0 DE, via Wikimedia Commons
By Klaus D. Peter, Wiehl, Germany, CC BY 3.0 DE, via Wikimedia Commons
Signs
There is usually only one nodule - most often on the outer side of the helix, commonly at its apex:
The nodule is firm, tender and well demarcated.
Size range is 3-20 mm in diameter - usually about 6 mm in diameter.
It is round or oval, slightly raised and firmly stuck to the underlying cartilage.
It may appear inflamed.
The surface appears scaly or crusty. If the crust is removed, a small raw area or core may be visible centrally.
Differential diagnosis5
Back to contentsElastotic nodules of the ears.
Cystic chondromalacia.
Continue reading below
Investigations6
Back to contentsBiopsy is needed if the diagnosis is uncertain, particularly to exclude basal cell carcinoma or squamous cell carcinoma.
Associated diseases
Back to contentsThe condition is benign. One study suggested an association with immune-mediated vascular compromise and necrobiotic collagenous disease such as granuloma annulare, especially in younger patients.7
Another report concerns a patient with systemic sclerosis and primary biliary cirrhosis (Reynold's syndrome). Such patients have an increased risk of developing skin malignancies.2
Chondrodermatitis nodularis treatment and management4
Back to contentsThe lesion rarely resolves spontaneously and so will usually need some form of treatment if it is causing discomfort or annoyance. A trial of conservative therapy for all patients is suggested.1 8
Conservative management
The aim of treatment is to reduce pressure on the site of the lesion - for example, by:
Altering the way headphones or telephone receivers are held to the ear.
Sleeping on the opposite side, if possible.
Using a soft pillow, or modifying the pillow with a hole where the nodule is in contact. A doughnut-shaped pillow was effective in one study.8 A haemorrhoid cushion is a novel cheap alternative.9
Using a corn plaster.
A pressure-relieving device, which can be made by using foam plastic to be applied at night.7
Using a protective made-to-measure silicone splint.1
In addition:
Avoid excessive exposure to the cold and the sun.
Topical antibiotics for secondary infections or ulceration. Petroleum jelly may also help if the lesion is ulcerated.1
Further management10
Topical nitroglycerin has been beneficial in the control of symptoms and in improving appearance.11
Topical and intralesional steroids may relieve discomfort.
Cryotherapy has been used.
CO2 and argon lasers have been used with benefit in a small number of patients.
Photodynamic therapy has shown some promise and is currently being investigated.
Surgery:
There are various surgical techniques used to achieve excision of the affected cartilage with reconstruction of the overlying skin.
Excision of the damaged area of cartilage is usually successful but recurrence can occur at the edge of the excised area.
Narrow elliptical excision of the skin lesion with shaving of the underlying cartilage appears to be as effective and less invasive, and to have similar recurrence rates (around 13.5% after four years or so).12
Excision by punch biopsy, with full-thickness skin grafting (the 'punch and graft' technique).1
Prognosis
Back to contentsFurther reading and references
- Elsensohn A, Getty S, Shiu J, et al; Intradermal Proliferative Fasciitis Occurring With Chondrodermatitis Nodularis Helicis. Am J Dermatopathol. 2017 Nov 21. doi: 10.1097/DAD.0000000000001027.
- Kumar P, Barkat R; Chondrodermatitis nodularis chronica helicis. Indian Dermatol Online J. 2017 Jan-Feb;8(1):48-49. doi: 10.4103/2229-5178.198767.
- Chondrodermatitis nodularis helicis; DermNet NZ
- Sifuentes Giraldo WA, Gonzalez-Garcia C, de Las Heras Alonso E, et al; Chondrodermatitis nodularis chronica helicis in a patient with systemic sclerosis associated with primary biliary cirrhosis (Reynolds syndrome): A case report. Eur J Rheumatol. 2014 Dec;1(4):161-163. doi: 10.5152/eurjrheumatol.2014.140048. Epub 2014 Dec 1.
- Orengo I, Robbins K, Marsch A; Pathology of the ear. Semin Plast Surg. 2011 Nov;25(4):279-87. doi: 10.1055/s-0031-1288920.
- Salah H, Urso B, Khachemoune A; Review of the Etiopathogenesis and Management Options of Chondrodermatitis Nodularis Chronica Helicis. Cureus. 2018 Mar 26;10(3):e2367. doi: 10.7759/cureus.2367.
- Wagner G, Liefeith J, Sachse MM; Clinical appearance, differential diagnoses and therapeutical options of chondrodermatitis nodularis chronica helicis Winkler. J Dtsch Dermatol Ges. 2011 Apr;9(4):287-91. doi: 10.1111/j.1610-0387.2011.07601.x. Epub 2011 Jan 31.
- Chondrodermatitis nodularis helicis; Primary Care Dermatology Society (PCDS)
- Kuen-Spiegl M, Ratzinger G, Sepp N, et al; Chondrodermatitis nodularis chronica helicis - a conservative therapeutic approach by decompression. J Dtsch Dermatol Ges. 2011 Apr;9(4):292-6. doi: 10.1111/j.1610-0387.2010.07572.x. Epub 2010 Nov 23.
- Sanu A, Koppana R, Snow DG; Management of chondrodermatitis nodularis chronica helicis using a 'doughnut pillow'. J Laryngol Otol. 2007 Nov;121(11):1096-8. Epub 2007 May 24.
- Ali FR, Healy C, Mallipeddi R; Hemorrhoid cushions for chondrodermatitis nodularis helicis (CNH): Piling off the pressure. J Am Acad Dermatol. 2016 Aug;75(2):e65-6. doi: 10.1016/j.jaad.2016.03.014.
- Juul Nielsen L, Holkmann Olsen C, Lock-Andersen J; Therapeutic Options of Chondrodermatitis Nodularis Helicis. Plast Surg Int. 2016;2016:4340168. doi: 10.1155/2016/4340168. Epub 2016 Jan 27.
- Flynn V, Chisholm C, Grimwood R; Topical nitroglycerin: a promising treatment option for chondrodermatitis nodularis helicis. J Am Acad Dermatol. 2011 Sep;65(3):531-6. doi: 10.1016/j.jaad.2010.06.012. Epub 2011 May 6.
- Rex J, Ribera M, Bielsa I, et al; Narrow elliptical skin excision and cartilage shaving for treatment of chondrodermatitis nodularis. Dermatol Surg. 2006 Mar;32(3):400-4.
Continue reading below
Article history
The information on this page is written and peer reviewed by qualified clinicians.
Next review due: 9 Feb 2028
10 Feb 2023 | Latest version

Ask, share, connect.
Browse discussions, ask questions, and share experiences across hundreds of health topics.

Feeling unwell?
Assess your symptoms online for free