Lumps in the groin and scrotum
Peer reviewed by Dr Hayley Willacy, FRCGP Last updated by Dr Colin Tidy, MRCGPLast updated 7 Feb 2024
Meets Patient’s editorial guidelines
- DownloadDownload
- Share
- Language
- Discussion
Medical Professionals
Professional Reference articles are designed for health professionals to use. They are written by UK doctors and based on research evidence, UK and European Guidelines. You may find the Lumps in the groin article more useful, or one of our other health articles.
In this article:
Lumps in the groin and scrotum can occur at any age. Clinical assessment is needed to detect those which need urgent investigation or treatment. Usually a working diagnosis can be made clinically, and ultrasound is often helpful.
Continue reading below
Causes of lumps in the groin and scrotum (aetiology)
Groin lumps
Painful lumps:
Tender lymph nodes.
Strangulated femoral hernia.
Strangulated inguinal hernia.
Psoas abscess.
Painless lumps:
Skin swellings - eg, epidermal (sebaceous) cyst, contact dermatitis.
Non-tender nodes.
Inguinal hernia.
Vascular:
Saphena varix (varicosity of saphenous vein at the junction with the femoral vein).
Scrotal lumps1
Painful lumps:
Torsion of a testicular or epididymal appendage.
Haematocele/haematoma.
Painless lumps:
Inguinal hernia (may sometimes be painful).
Spermatocele (feels similar to epididymal cyst but is filled with semen).
Skin swellings (as for groin lumps).
Less common causes of scrotal swelling include:
Idiopathic scrotal oedema (mainly children).
Infections:
Syphilitic gumma of the testis (round, hard, insensitive mass, indistinguishable from a tumour).
Tuberculous epididymitis.2
Pancreatitis (fluid may track down the retroperitoneal compartment into the inguinal canal and scrotal sac).
Complications of peritoneal dialysis and ventriculoperitoneal shunts.
Crohn's disease manifestations: erythema nodosum and pyoderma gangrenosum.
Metastases (mainly from penile lesions).
Congenital abnormalities of lymphatic vessels (Milroy's disease).
Generalised oedema.
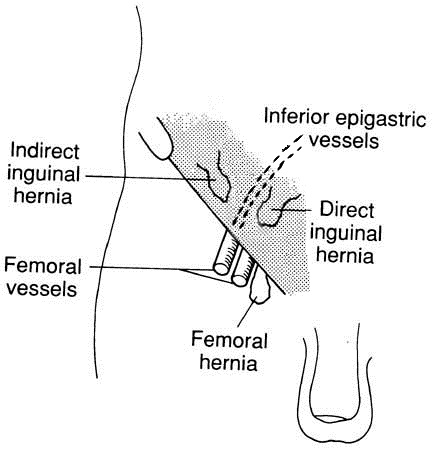
Anatomy of structures in the groin and scrotum
Back to contentsCross-section view
Inguinal hernia
Continue reading below
Assessment1
Back to contentsHistory
Pain.
Duration and speed of onset (sudden in testicular torsion, more gradual in epididymo-orchitis).
Change in size.
Trauma.
Note whether it reduces (eg, on lying down).
Previous episodes. (Those with testicular torsion may have had previous self-limiting episodes.)
Associated symptoms:
Urethral discharge or dysuria (suggests epididymo-orchitis).
Abdominal pain, nausea and vomiting (can occur with testicular torsion).
Back pain, weight loss, dyspnoea (can occur with metastatic testicular cancer).
Parotid swelling (mumps orchitis).
Examination1 3
This should be carried out with the patient both standing and supine - hernias, varicoceles and saphena varix are more prominent when the patient is standing.
Check the normal structures and landmarks, which are:
Inguinal ligament.
Femoral artery.
Pubic tubercle.
Testis.
Epididymis.
Spermatic cord.
When examining the lump, note:
Tenderness: suggests infection or ischaemia, so think of testicular torsion, a strangulated hernia, epididymo-orchitis or psoas abscess.
Consistency of swelling: firm or solid for malignancy, soft and fluctuant for a cyst or hernia.
Location relative to landmarks. Femoral hernias are below and lateral to the pubic tubercle but, in practice, it is not always possible to distinguish inguinal and femoral hernias.
Note whether you can you 'get above' the swelling (ie feel the upper border of it). You cannot 'get above' a hernia.
Testis:
Note whether the lump is separate from the testis.
Testicular lie (may be transverse or high-riding in testicular torsion).
Cremasteric reflex. In the normal reflex, light stroking of the inner thigh causes contraction of the cremasteric muscle and therefore the testis on that side is pulled up. If absent, and there is acute scrotal pain or swelling, suspect testicular torsion.
A cough impulse suggests hernia or saphena varix.
Transillumination: cystic swellings such as hydroceles transilluminate well; solid tumours and most hernias don't. Inguinal hernias in infants may transilluminate.
Skin changes - a raised papule, plaque, or ulcer suggests scrotal cancer (rare).
Presence or absence of lymphadenopathy.
It is not necessary to distinguish between direct and indirect inguinal hernias.
Varicoceles typically feel like a 'bag of worms' and are more often left-sided.
Scrotal swellings - urgent problems not to miss1
Testicular torsion
Requires a low threshold of suspicion and immediate referral:
May be difficult to exclude on clinical grounds; may mimic epididymo-orchitis.
Common in teenagers; rare >30 years of age.
Sudden or gradual onset; may have had previous self-limiting pain episodes.
Painful; usually severe pain, which may radiate to the abdomen; may have vomiting.
Cremasteric reflex is almost always absent.
Testis is often elevated or lying transversely.
Neonates - testis is hard, non-tender, and usually haemorrhagic.
Testicular cancer
Most common in men aged 20-40 years; can occur in older men (usually lymphoma).
Usually presents with testicular enlargement.
Often painless and non-tender; there may be a dragging sensation. Pain is present in 20-30%.
May have back or flank pain, dyspnoea, supraclavicular lymphadenopathy, abdominal mass (enlarged para-aortic lymph nodes), weight loss, gynaecomastia, epididymo-orchitis, or hydrocele.
On palpation, solid/firm swelling involving all or part of the testis.
Inguinal hernias in infants, or if strangulated/obstructed
May enlarge with Valsalva-type manoeuvres, and disappear on lying down (if reducible).
Positive cough impulse; bowel sounds on auscultation.
May be features of strangulation or obstruction (abdominal pain and/or intestinal obstruction symptoms).
Cannot get above the swelling.
Squamous cell carcinoma of the scrotum
Extremely rare; usually only in men aged >50 years.
Raised papule, plaque, or ulcer on the scrotal wall; often purulent.
Inguinal lymphadenopathy may be present (due to metastases or infection).
The National Institute for Health and Care Excellence (NICE) guidance on suspected cancer recognition and referral for testicular cancer states:4
Consider a suspected cancer pathway referral for testicular cancer in men if they have a non-painful enlargement or change in shape or texture of the testis.
Consider a direct access ultrasound scan for testicular cancer in men with unexplained or persistent testicular symptoms.
Diagnosing lumps in the groin and scrotum(investigations)
Back to contentsClinically suspected testicular cancer: do not wait for investigations, but refer urgently to be seen within two weeks by a urologist. Alpha-fetoprotein (AFP) and beta human chorionic gonadotrophin (beta-hCG) are tumour markers for testicular cancer - can arrange a blood test while awaiting appointment.
Where diagnosis is unclear, request urgent ultrasound of the scrotum and/or groin (almost 100% sensitive for testicular tumours). This is useful, for example, where the body of the testis cannot be distinguished or where it is not clear whether the swelling is testicular or extratesticular, and for hydroceles in adults (to exclude testicular cancer).
Tests as appropriate for sexually transmitted infections where there is epididymo-orchitis.
Acute lymphadenopathy may need investigation for limb or genital/sexually transmitted infection.
Persistent unexplained lymphadenopathy needs biopsy.
Inguinal hernias in baby girls probably merit investigation for androgen insensitivity syndrome.5
Continue reading below
Management of lumps in the groin and scrotum
Back to contentsThis depends on the diagnosis, but note that:
Immediate referral is necessary for:
Suspected torsion of the testis.
Strangulated or obstructed hernia.
Urgent referral/investigation is needed for:
Femoral hernias:
These are more likely to strangulate than inguinal hernias; if suspected, they should be referred for surgery to be considered.
Hydroceles:
In infants, these usually resolve spontaneously.
Hydroceles occurring in adults may be secondary to testicular tumour or infection and should be investigated - request urgent ultrasound for hydrocele in men aged 20-40 years.1
Prevention of lumps in the groin and scrotum
Back to contentsTesticular cancer may present as a painless testicular swelling, and is often curable if treated early. Testicular self-examination may have a role in the early detection of testicular cancer. As for any lump, early consultation for testicular swellings should be encouraged.
Further reading and references
- Tiemstra JD, Kapoor S; Evaluation of scrotal masses. Am Fam Physician. 2008 Nov 15;78(10):1165-70.
- Walker NA, Challacombe B; Managing epididymo-orchitis in general practice. Practitioner. 2013 Apr;257(1760):21-5, 2-3.
- Acute scrotal pain or swelling, Clinical practice guidelines; The Royal Childrens Hospital Melbourne, January 2013
- Guidelines on Testicular Cancer; European Association of Urology (2025)
- United Kingdom BASHH national guideline for the management of epididymo-orchitis; British Association for Sexual Health and HIV (2019)
- Scrotal pain and swelling; NICE CKS; August 2024 (UK access only)
- Viswaroop BS, Kekre N, Gopalakrishnan G; Isolated tuberculous epididymitis: a review of forty cases. J Postgrad Med. 2005 Apr-Jun;51(2):109-11, discussion 111.
- Jenkins JT, O'Dwyer PJ; Inguinal hernias. BMJ. 2008 Feb 2;336(7638):269-72.
- Suspected cancer: recognition and referral; NICE guideline (2015 - last updated May 2025)
- Deeb A, Hughes IA; Inguinal hernia in female infants: a cue to check the sex chromosomes? BJU Int. 2005 Aug;96(3):401-3.
- Wang KS; Assessment and management of inguinal hernia in infants. Pediatrics. 2012 Oct;130(4):768-73. doi: 10.1542/peds.2012-2008. Epub 2012 Sep 24.
- Rosenberg J; Pediatric inguinal hernia repair-a critical appraisal. Hernia. 2008 Apr;12(2):113-5. Epub 2007 Nov 30.
Continue reading below
Article history
The information on this page is written and peer reviewed by qualified clinicians.
Next review due: 5 Feb 2029
7 Feb 2024 | Latest version

Ask, share, connect.
Browse discussions, ask questions, and share experiences across hundreds of health topics.

Feeling unwell?
Assess your symptoms online for free