Visual field defects
Peer reviewed by Dr Hayley Willacy, FRCGP Last updated by Dr Colin Tidy, MRCGPLast updated 23 Dec 2024
Meets Patient’s editorial guidelines
- DownloadDownload
- Share
- Language
- Discussion
Medical Professionals
Professional Reference articles are designed for health professionals to use. They are written by UK doctors and based on research evidence, UK and European Guidelines. You may find the Visual problems article more useful, or one of our other health articles.
In this article:
Continue reading below
What is a visual field defect?
The visual field is the portion of the subject's surroundings that can be seen at any one time. The normal extent of field of vision is 50° superiorly, 60° nasally, 70° inferiorly and 90° temporally. A visual field defect is a loss of part of the usual field of vision, so it does not include severe visual impairment of either one eye or both. The lesion may be anywhere along the optic pathway; retina to occipital cortex.
Causes of visual field defects (aetiology)1
Back to contentsThere are many causes of visual field loss. Some more common ones are included here.
Central field loss results from degeneration of the fovea and occurs with:
Age-related macular degeneration.
Optic neuropathy.
Leber's optic atrophy.
Macular holes.
Cone dystrophies.2
Retinal artery occlusion.
A number of rare conditions like Best's disease, Stargardt's disease and achromatopsia.
Peripheral field loss occurs with:
Glaucoma (angle-closure glaucoma and open-angle glaucoma).
Retinal detachment.
Retinitis pigmentosa.
Chorioretinitis.
Branch retinal artery occlusion.
Continue reading below
History
Back to contentsThe following need to be established:
Was the onset sudden, rapid or slow?
Where is the field loss? It is often helpful to say to the patient: "If what you see is like a television screen then where is the bit that is missing?"
Does it affect one eye or both? If the patient thinks that it affects only one eye, it is worth asking them to close or cover the affected eye and to note again if there is any visual loss. If it is much more marked in one eye than the other, the loss in the less affected eye may be overlooked.
What does the visual defect look like to the patient? It may, for example, be a black spot, a blur or the picture may look normal, If the lesion is cortical or onset has been insidious, the patient may fail to notice any defect.
Looking for evidence of 'asymptomatic' visual field loss
Does the patient tend to bump into people or things?
Has the patient been involved in any motor vehicle accidents? Patients who drive whilst unaware of significant field loss may fail to judge parking, negotiate obstacles or notice other vehicles at road junctions. There can be denial or lack of insight despite numerous such accidents.
Are there any associated neurological or ophthalmic symptoms?
Examination
Back to contentsVisual acuity tests the eye's greatest power of resolution, whereas visual field testing measures the peripheral sensitivity.
Remember that the image on the retina is upside down and inverted. Hence, a lesion of the top right of the retina or in the pathway beyond will cause a defect in the bottom left of the visual field. Assessing for visual field defects can be via:
Screening tests (easily carried out in a surgery) which include confrontational visual field testing and use of an Amsler grid.
Quantitative measurements using manual or automated perimetry (specialist equipment is needed).
Types of visual field loss include:
Central or peripheral
Loss may be central/foveal (eg, an optic disc or nerve problem) or peripheral (along the visual pathways from the optic chiasm back).
Scotoma
This is a defect surrounded by normal visual field. It may begin as a gradual enlargement of the blind spot and may pass unnoticed by the patient until quite large.
Relative scotoma - an area where objects of low luminance cannot be seen but larger or brighter ones can.
Absolute scotoma - nothing can be seen at all within that area.
Hemianopia
This is a binocular visual defect in each eye's hemifield.
Bitemporal hemianopia - the two halves lost are on the outside of each eye's peripheral vision, effectively creating a central visual tunnel.
Homonymous hemianopia - the two halves lost are on the corresponding area of the visual field in both eyes, ie either the left or the right half of the visual field.
Altitudinal hemianopia - the dividing line between loss and sight is horizontal, with visual loss either above or below the line.
Quadrantanopia - this is an incomplete hemianopia referring to a quarter of the schematic 'pie' of visual field loss.
Sectoral defect - this is another term for incomplete hemianopia.3
Confrontation visual field testing
This is a simple (but approximate) qualitative method of assessing visual field loss. It is a good starting point and can easily be carried out in the surgery. Traditionally a pin with a coloured end has been used to define the visual field. A red or a white head is used and it may be moved across the visual field to ascertain where it disappears and hence to define a scotoma.
Sit approximately 1 metre from the patient, facing the patient. Make sure that they have the acuity to see the intended target. Remove the patient's glasses if worn, as the rims get in the way.
Look at the patient's nose and ask the patient to look at yours.
Test each eye separately; cover the other eye. You can ask the patient to cover or close one eye and you close the eye opposite.
Make sure the target is equidistant between you and the patient.
Starting at the top outer quadrant, move the target object (eg, fingers or hatpin) in from the side and ask the patient to tell you when they first see the object and, as you move towards the centre, whether they disappear.
Repeat the process in each quadrant and for each eye separately.
If you detect a defect, re-examine that area and define it further.
Assess the blind spot (if you can't find it, then it's probably not enlarged).
Repeat for the fellow eye.
Then systematically assess:
Pupils and optic nerve function (visual acuity, relative afferent pupillary defect, colour impairment and brightness sensitivity).
Fundus.
Neurological examination (if a systemic problem is suspected).
Difficulties
The most common is the patient's (or your) eye drifting away from the nose. You may need to remind them throughout the test to keep fixing on your nose.
This technique compares the patient's visual field with yours, so it assumes normal examiner visual fields.
Visual fields in infants can be crudely assessed by making use of their involuntary fixational reflexes. First the child's attention is held in a frontal gaze; then, while the child is watching the examiner's face, the examiner silently brings an interesting toy in from the periphery. This is difficult to do well and eyes cannot be tested individually.
Amsler grid testing
This assesses the central 10° of the visual field. It detects central and paracentral scotomas. See the separate Examination of the eye article for details on performing this easy test.
Other examinations in a GP surgery
Visual field defects may stem from neurological or ophthalmic problems. Depending on what the history and findings so far suggest, a full neurological examination or further tests on the eye may be warranted. The Examination of the eye article offers further details.
Quantitative measurements
There are a number of techniques used in specialist practice. They fall into one of two categories: static or kinetic perimetry.
Static perimetry
This is the most commonly used assessment. An 'on/off' light signal is presented throughout the patient's potential visual field and the patient clicks every time they see the signal. These automated machines can assess various amounts of the visual field (10° to full field).
These are sensitive tests but are difficult to perform: they take time and can be very tiring for the patient. Frailer patients who may tire easily, patients unable to sit still for long or those unable to follow the instructions will deliver unreliable results. Even a temporary loss of concentration can affect the results. Pupil size, refractive error and artefacts (drooping eyelid, spectacle rim) may also affect the result if not taken into consideration.
Kinetic perimetry
This is based on presenting a moving stimulus from a non-seeing area to a seeing area. It is repeated at various points around a 'clock-face' chart of the field of vision; a mark is made as soon as the point is seen. These points are then joined by a line (an isoptre). The process is repeated with a point of lesser luminescence and another isoptre is created. Thus, a number of isoptres are plotted to produce a chart showing maximal peripheral vision for each (decreasing) level of brightness.
The most commonly used kinetic test is called Goldmann's perimetry. It tends to be used for neurological conditions. It is also used where there is suspicion of functional rather than organic problems, when a characteristic pattern of spiralling isoptres may be seen. Goldmann's perimetry can be affected by ptosis, refractive errors, tremor and inadequate operator skills.
Continue reading below
Interpretation
Back to contentsUnderstanding the pathological process relating to visual field defects requires an understanding of the anatomical arrangement of the visual pathway.
Visual pathway 1
The visual image is projected through the lens on to the retina upside down, and laterally reversed.
The macula (and, within the macula, the fovea) is responsible for central vision. Fibres from the macula feed into the temporal part of the optic nerve at the level of the retina and gradually migrate to the central part of the optic nerve at the optic chiasm.
The information from each eye is split at the chiasm, with the medial fibres (lateral visual field) crossing to the opposite side and the lateral fibres (nasal visual field) passing to the ipsilateral optic tract. This ensures that information from both eyes concerning the same part of the visual field passes to the same part of the visual cortex (left half of visual field in right optic tract) via the optic tract, geniculate body and optic radiation.
Visual Field Defects
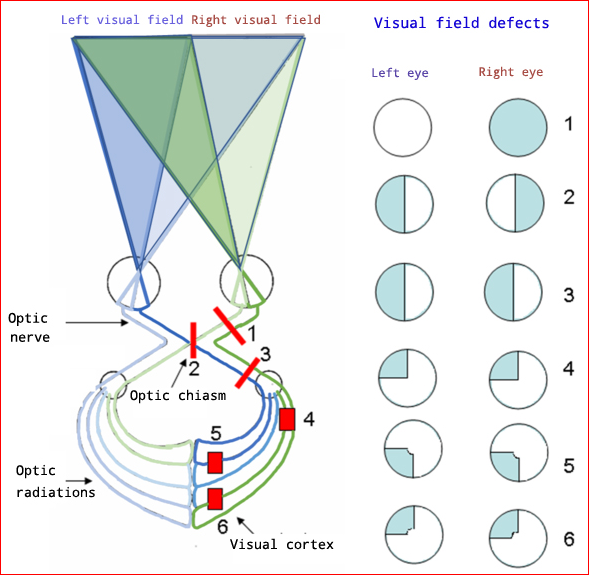
As eo, CC BY-SA 4.0, via Wikimedia Commons
Lesions at the level of the retina
These affect one eye only.
Retinal detachment and occlusion of blood vessels at a level smaller than the central retinal artery or vein, give defects with boundaries in the horizontal meridian.
Retinal detachment tends to be fairly rapid in onset. It may be preceded by floaters and flashes before the patient notices 'a curtain' coming across the visual field. A crescentic reddish slip of detachment may be apparent at the periphery of the retina.
Central retinal artery occlusion tends to be a sudden and complete loss of vision in one eye but, if occlusion is at the level of one of the four arteries to the retina, there will be loss of just a quadrant of field. The affected area will look pale and poorly supplied with blood vessels.
Central retinal vein occlusion presents in a fairly similar way to arterial occlusion but the retina looks hyperaemic. Haemorrhages are scattered throughout the fundus in a typical blood-storm pattern with cotton-wool spots. With incomplete blockage, sparse scattered haemorrhages occur.
Age-related macular degeneration affects the macular area; the periphery is spared until very late.
Drugs can cause disturbance of visual fields. This tends to be bilateral - eg:
Lesions before the chiasm
These produce a field deficit in the ipsilateral eye. Field defects from damage to the optic nerve tend to be central, asymmetrical and unilateral; visual acuity is often affected.
Possible causes include:
Trauma (incomplete damage, transection or blunt trauma).
Lesions just before the chiasm can also produce a small defect in the upper temporal field of the other eye as the decussating fibres loop back into the optic nerve after crossing (anterior chiasmal syndrome - eg, meningioma).
Lesions at the chiasm
These classically produce a bitemporal hemianopia.
If they spread up from below (for example, pituitary tumours), the defect is worse in the upper field.
If they spread down from above (for example, craniopharyngioma), the lesion is worse in the lower quadrants.
Lesions at the optic chiasm may show a phenomenon where two identical coloured objects are shown to one eye in the left and right halves of the visual field but one appears to be brighter and sharper than the other. For example, with a right hemianopia the left hemifield is brighter than the right.
Lesions after the chiasm
These produce homonymous (matching) field defects; because of image reversal, a lesion in the right optic tract produces a left visual field defect. Fibres in the optic tracts gradually rotate until the fibres reach the geniculate body, so lesions in the tract before the geniculate body may produce incongruous defects.
Lesions in the main optic radiation or optic peduncle cause complete (left or right) homonymous hemianopia without macular sparing. This is seen in stroke and middle cerebral artery lesions.
Lesions in the temporal radiation cause upper quadrantic homonymous hemianopia, commonly with macular sparing - eg, tumours.
Lesions in the parietal radiation cause inferior quadrantic homonymous hemianopia without macular sparing.
Lesions in the anterior visual cortex (common) produce a contralateral homonymous hemianopia with macular sparing - eg, posterior cerebral artery occlusion.
Lesions in the macular cortex produce homonymous macular defect - eg, blunt injury to the occiput.
Lesions of the intermediate visual cortex produce an homonymous arc scotoma, with sparing of both macula and periphery. This is seen in a distal posterior cerebral artery occlusion.
Occipital lobe lesions
If both occipital lobes are injured then the patient is in a state of cortical visual impairment. The patient is unable to process visual information and behaves in a similar fashion to someone who develops a peripheral visual loss. However, some patients still try to behave as if they have vision. This state of unawareness of cortical visual loss is called Anton's syndrome.
Lesion of the primary visual perception area of the right or left occipital lobe will produce a clear loss of visual perception from the contralateral visual field. Patients are usually aware of the deficit and do not neglect that side of the visual field.
Ventral stream damage; this area is involved with recognition; damage here does not tend to produce visual field defects.
Safety to drive and DVLA
Back to contentsPatients with a newly diagnosed significant visual field defect should not drive until this has been formally assessed. Patients must inform the DVLA which will then organise for them to have a very specific visual field test (Estermann's visual field test), carried out by one of their approved optometrists. The approved optometrist then reports back to their medical officers, who make the final decision regarding whether a person is safe to drive.
Dr Mary Lowth is an author or the original author of this leaflet.
Further reading and references
- Assessing fitness to drive: guide for medical professionals; Driver and Vehicle Licensing Agency
- Howard C, Rowe FJ; Adaptation to poststroke visual field loss: A systematic review. Brain Behav. 2018 Aug;8(8):e01041. doi: 10.1002/brb3.1041. Epub 2018 Jul 13.
- Broadway DC, Kyari F; Examining visual fields. Community Eye Health. 2019;32(107):58-59. Epub 2019 Dec 17.
- Gupta M, Bordoni B; Neuroanatomy, Visual Pathway. StatPearls, Jan 2024.
- Michaelides M, Hunt DM, Moore AT; The cone dysfunction syndromes. Br J Ophthalmol. 2004 Feb;88(2):291
- Goodwin D; Homonymous hemianopia: challenges and solutions. Clin Ophthalmol. 2014 Sep 22;8:1919-27. doi: 10.2147/OPTH.S59452. eCollection 2014.
- Almony A, Garg S, Peters RK, et al; Threshold Amsler grid as a screening tool for asymptomatic patients on hydroxychloroquine therapy. Br J Ophthalmol. 2005 May;89(5):569
- Constable S, Pirmohamed M; Drugs and the retina. Expert Opin Drug Saf. 2004 May;3(3):249
Continue reading below
Article history
The information on this page is written and peer reviewed by qualified clinicians.
Next review due: 22 Dec 2027
23 Dec 2024 | Latest version

Ask, share, connect.
Browse discussions, ask questions, and share experiences across hundreds of health topics.

Feeling unwell?
Assess your symptoms online for free