Episcleritis and scleritis
Peer reviewed by Dr Colin Tidy, MRCGPLast updated by Dr Doug McKechnie, MRCGPLast updated 8 Jun 2023
Meets Patient’s editorial guidelines
- DownloadDownload
- Share
- Language
- Discussion
- Audio Version
In this series:Eye problemsInfective conjunctivitisAllergic conjunctivitisDry eyesUveitisSubconjunctival haemorrhage
Episcleritis and scleritis are inflammatory conditions which affect the eye. Both cause redness, but scleritis is much more serious (and rarer) than episcleritis.
In this article:
Video picks for Eye conditions
Key points
Episcleritis is a mild eye condition that causes redness and irritation in the outer layer of the white part of the eye. It often gets better on its own or with simple treatments like lubricating eye drops.
Scleritis is a serious eye condition that causes deep, aching pain, redness, and sometimes blurred vision. It affects the deeper layers of the eye and often requires anti-inflammatory or immunosuppressive treatment.
The exact cause of both conditions is unknown, but they can be linked to underlying health issues such as rheumatoid arthritis or other autoimmune diseases.
Continue reading below
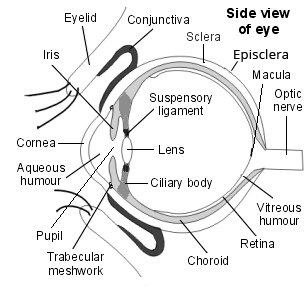
The anatomy of the eye
The diagram shows the eye including the sclera. The episclera lies between the sclera and the conjunctiva.
The sclera is the white part of the eye. The episclera lies directly on top of the sclera.
Side view of the structure of the eye
What is episcleritis?
Back to contentsEpiscleritis affects only the episclera, which is the layer of the eye's surface lying directly between the clear membrane on the outside (the conjunctiva) and the firm white part beneath (the sclera). It causes redness and inflammation of the eye, often with discomfort and irritation but without other significant symptoms.
Continue reading below
What is scleritis?
Back to contentsScleritis affects the sclera and, sometimes, the deeper tissues of the eye. It is much less common than episcleritis. It causes a painful red eye and can affect vision, sometimes permanently. Scleritis is a more serious condition than episcleritis.
Can episcleritis turn into scleritis?
Back to contentsEpiscleritis and scleritis are mainly seen in adults. Episcleritis does not cause scleritis, although scleritis can lead to associated episcleritis. They can initially look similar but they do not feel similar and they do not behave similarly. Both are slightly more common in women than in men. Both can be associated with other conditions such as rheumatoid arthritis and systemic lupus erythematosus (SLE), although this is more likely in the case of scleritis.
Continue reading below
Episcleritis vs scleritis
Back to contentsEpiscleritis is a fairly common condition. It tends to come on quickly. It causes redness - often in a wedge shape over the white of the eye - and mild discomfort. A lot of people might have it and never see a doctor about it. It can occasionally be a little more painful than this and can cause inflamed bumps to form on the surface of the eye. The inflamed bumps are called nodules.
However, it is generally a mild condition with no serious consequences. It usually settles down by itself over a week or so with simple treatment. Episcleritis is often recurrent and can affect one or both eyes.
Episcleritis

© Asagan, CC BY-SA 3.0, via Wikimedia Commons
By Asagan (own work), CC BY-SA 3.0, via Wikimedia Commons
Scleritis is much less common and more serious. It tends to come on more slowly and affects the deep white layer (sclera) of the eye. It can spread to affect the adjacent layers around the sclera, including the episclera and the cornea.
Scleritis tends to be very painful, causing a deep 'boring' kind of pain in or around the eye: that's how it is distinguished from episcleritis which is uncomfortable but not that painful. The eye is likely to be watery and sensitive to light and vision may be blurred.
Scleritis can affect vision permanently. It may involve one or both eyes and is often associated with other inflammatory conditions such as rheumatoid arthritis.
Scleritis eye inflammation
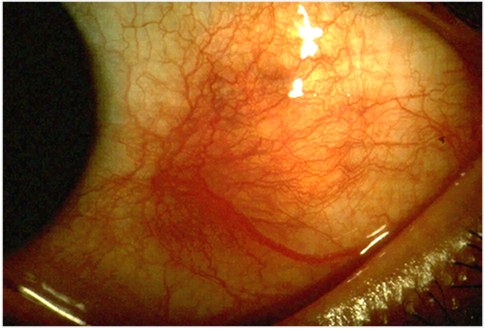
© Kribz, CC BY-SA 3.0, via Wikimedia Commons
By Kribz (Own work), CC BY-SA 3.0, via Wikimedia Commons
What causes episcleritis and scleritis?
Back to contentsEpiscleritis and scleritis are inflammatory conditions. It's not known what triggers the inflammation, which seems to start in the small blood vessels running on the surface of the eye.
Both conditions are more likely to occur in people who have other inflammatory conditions, although this is particularly true of scleritis. Scleritis can occasionally be caused by infection with germs such as bacteria, viruses or, rarely, fungi.
Who develops episcleritis and scleritis?
Back to contentsEpiscleritis is most common in adults in their 40s and 50s. It is slightly more common in women than in men, and in people who have connective disease such as rheumatoid arthritis.
About 40 people per 100,000 per year are thought to be affected. However, this is difficult to estimate accurately because many people do not go to a doctor if they have mild episcleritis.
Scleritis is less common, affecting only about 4 people per 100,000 per year. It affects a slightly older age group, usually the fourth to sixth decades of life. It is also slightly more common in women. It is more likely than episcleritis to be associated with an underlying inflammatory condition like rheumatoid arthritis.
Episcleritis symptoms
Back to contentsThere are two types of episcleritis.
The most common type is called diffuse episcleritis and it makes the surface of the eye evenly red, sometimes all over and sometimes in a wedge shape.
The less common type is called nodular episcleritis. It comes on more slowly and causes inflamed swollen bumps or nodules in the episclera. It is more likely than diffuse episcleritis to be associated with an underlying inflammatory condition.
Both forms of episcleritis cause mild discomfort in the eye. The eyes may water a little and the eye may be a little tender when pressure is applied over the red area. However, vision is unaffected and painkillers are not generally needed.
The diffuse type tends to be less painful than the nodular type.
Episcleritis is often a recurrent condition, with episodes occurring typically every few months. Most attacks last 7-10 days, although in the case of nodular episcleritis this can be a little longer.
Scleritis symptoms
Back to contentsScleritis causes redness of the eye. It tends to come on more slowly than episcleritis.
As the redness develops the eye becomes very painful. This is a deep boring kind of pain inside and around the eye. It is typically much more severe than the discomfort of episcleritis.
Sometimes the white of the eye has a bluish or purplish tinge.
Vision may be blurred, the eye may be watery (although there is no discharge) and you may find it difficult to tolerate light (photophobia).
There are several types of scleritis, depending on what part of the eye is affected and how inflamed the tissues are:
Anterior scleritis is divided into:
Non-necrotising type (most common). This is divided into:
Diffuse anterior scleritis in which the eye is uniformly red.
Nodular anterior scleritis in which tender nodules develop.
Necrotising type:
With inflammation: this is the most severe form of scleritis. It causes severe pain and tenderness and often causes permanent damage to the eye.
Without inflammation: this rare condition is called scleromalacia perforans and is only seen in patients with long-standing rheumatoid arthritis. The eye is not red or painful but the sclera is gradually thinned.
Posterior scleritis is rare and is also painful although your eye may not be red. Eye movements may be painful and there may be loss of vision.
Episcleritis treatment
Back to contentsEpiscleritis does not necessarily need any treatment. If symptoms are mild it will generally settle by itself.
Lubricating eye drops or ointment may ease the discomfort whilst symptoms settle.
If the eye is very uncomfortable, episcleritis may be treated with non-steroidal anti-inflammatory drugs (NSAIDs) in the form of eye drops.
If this isn't enough (more likely in the nodular type) steroid eye drops are sometimes used, although only under the care of an eye specialist (ophthalmologist).
If episcleritis does not settle over a week or if the pain becomes worse and your vision is affected, you should see a doctor in case you have scleritis.
Scleritis treatment
Back to contentsIf you develop scleritis you should be urgently referred to an eye specialist (ophthalmologist). You will usually need to be seen on the same day.
The management will depend on what type of scleritis this is and on its severity.
The non-necrotising types are usually treated with oral NSAID medication. If this isn't effective, oral steroids are needed.
Some doctors treat scleritis with injections of steroid medication into the sclera or around the eye.
If these treatments don't work then immunosuppressant drugs such as methotrexate and cyclophosphamide may be used. They can take several weeks to work.
Some of the new 'biological agents' such as rituximab can also be effective.
Sometimes surgery is needed to treat the complications of scleritis.
Necrotising scleritis is treated with oral steroids and immunosuppressants as early as possible.
Scleromalacia perforans does not respond well to treatment - research continues to find the best way to manage this rare condition.
What are the possible complications of episcleritis and scleritis?
Back to contentsEpiscleritis does not usually lead to any complications: your eyesight shouldn't be affected at all.
Scleritis can lead to permanent damage to the structure of the eye, including:
Thinning of the sclera.
Many of these conditions can permanently threaten sight and some will require surgical treatment.
What is the long-term outlook (prognosis) for episcleritis and scleritis?
Back to contentsEpiscleritis does not usually have any significant long-term consequences unless it is associated with an underlying disease such as rheumatoid arthritis.
The non-necrotising forms of scleritis do not usually permanently affect vision unless the patient goes on to develop uveitis.
Necrotising scleritis with inflammation is the most severe and distressing form of scleritis. It is common for vision to be permanently affected.
When either episcleritis or scleritis occurs in association with an underlying condition like rheumatoid arthritis then its progress tends to mirror that of the underlying disease.
Posterior scleritis is also associated with systemic disease and has a high likelihood of causing visual loss.
It can help to meet and talk to people who have had a similar experience with their eyes: search online for scleritis and episcleritis support groups.
How do I prevent episcleritis and scleritis?
Back to contentsThese inflammatory conditions cannot be directly prevented. For people with systemic inflammatory diseases such as rheumatoid arthritis, good control of the underlying disease is the best way of preventing this complication from arising.
Dr Mary Lowth is an author or the original author of this leaflet.
Frequently asked questions
Back to contentsCan children get episcleritis?
Yes, children can develop episcleritis, although it is more common in adults. It usually causes mild redness and irritation in one eye and often clears up on its own, but a healthcare professional should check any red eye to rule out more serious conditions.
How long does scleritis last?
leritis can last for several weeks to months, depending on its severity and underlying cause. Prompt treatment by an eye specialist is important to reduce pain, prevent complications, and protect your vision.
Patient picks for Eye conditions
Eye health
Acute angle-closure glaucoma
Acute angle-closure glaucoma is a serious eye condition that occurs when the fluid pressure inside the eye rises quickly, leading to sudden, severe eye pain, a red eye and reduced or blurred vision. It is a medical emergency.
by Dr Philippa Vincent, MRCGP

Eye health
Uveitis
Uveitis is a general term describing inflammation of the part of the eye called the uveal tract. This consists of the iris, ciliary body and choroid - although uveitis can additionally involve other parts of the eye.
by Dr Colin Tidy, MRCGP
Further reading and references
- Jabs DA, Mudun A, Dunn JP, et al; Episcleritis and scleritis: clinical features and treatment results. Am J Ophthalmol. 2000 Oct;130(4):469-76.
- Berchicci L, Miserocchi E, Di Nicola M, et al; Clinical features of patients with episcleritis and scleritis in an Italian tertiary care referral center. Eur J Ophthalmol. 2014 May-Jun;24(3):293-8. doi: 10.5301/ejo.5000394. Epub 2013 Nov 12.
- Al-Amry M; Nodular episcleritis after laser in situ keratomileusis in patient with systemic lupus erythematosus. Oman J Ophthalmol. 2013 Jan;6(1):65-6. doi: 10.4103/0974-620X.111938.
- Sambhav K, Majumder PD, Biswas J; Necrotizing scleritis in a case of Vogt-Koyanagi-Harada disease. Oman J Ophthalmol. 2015 Sep-Dec;8(3):216. doi: 10.4103/0974-620X.169909.
Continue reading below
Article history
The information on this page is written and peer reviewed by qualified clinicians.
Next review due: 12 May 2028
8 Jun 2023 | Latest version

Ask, share, connect.
Browse discussions, ask questions, and share experiences across hundreds of health topics.

Feeling unwell?
Assess your symptoms online for free
Sign up to the Patient newsletter
Your weekly dose of clear, trustworthy health advice - written to help you feel informed, confident and in control.
By subscribing you accept our Privacy Policy. You can unsubscribe at any time. We never sell your data.