Bronchoscopy
Peer reviewed by Dr Colin Tidy, MRCGPLast updated by Dr Toni Hazell, MRCGPLast updated 12 Jun 2023
Meets Patient’s editorial guidelines
- DownloadDownload
- Share
- Language
- Discussion
In this series:Chest infectionAcute bronchitisPneumoniaAspiration pneumoniaPost-operative chest infection
A bronchoscopy is a test which can help to diagnose and treat conditions of your breathing. It involves a doctor sliding a flexible camera-tube into your lungs.
Note: The information below is a general guide only. The arrangements and the way tests are performed often vary between different hospitals.
In this article:
Continue reading below
What is a bronchoscopy?
A bronchoscopy is a test where a doctor looks into your lungs with a thin, plastic camera tube.
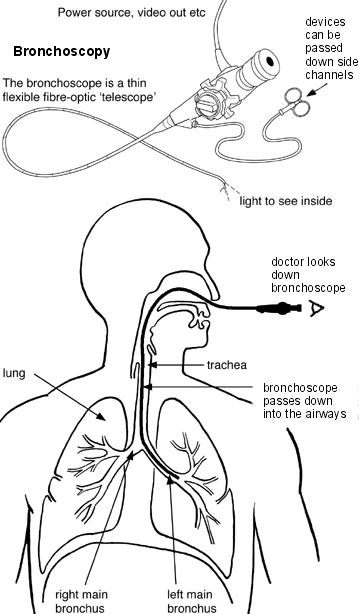
Diagram showing how a bronchoscopy is performed
This photo shows a bronchoscope:
Bronchoscope

© Håkon Olav Leira (Own work) via Wikimedia Commons
By Håkon Olav Leira (Own work) via Wikimedia Commons
A fibre-optic bronchoscope is the device usually used. This is a thin, flexible, telescope (shown in the diagram). It is about as thin as a pencil. You are usually awake during a bronchoscopy, but usually are sedated and made very sleepy. It may be uncomfortable but is not painful.
The bronchoscope is passed through your nose or mouth, down the back of your throat, into your windpipe (trachea), and down into your bronchi. The fibre-optics allow light to shine around bends in the bronchoscope and so the doctor can see clearly inside your airways.
A rigid bronchoscope (not shown in diagram) is used much less often. It is like a thin, straight telescope. It may be needed for some procedures and in children. It requires a general anaesthetic. (A fibre-optic bronchoscopy only requires sedation.)
Both types of bronchoscopes have a side channel down which thin instruments can pass. For example, a thin grabbing instrument can pass down to take a small sample (biopsy) from the inside lining of an airway, or from structures next to the airways.
Who has a bronchoscopy?
Back to contentsTo help diagnose a problem
There are various reasons for having a bronchoscopy. For example, to help make a diagnosis if you have a persistent cough or cough up blood and the cause is not clear. If you have a shadow on a chest X-ray or the doctor sees a growth or a strange-looking area in a bronchus, the doctor may take a small sample (a biopsy) during a bronchoscopy.
The sample is then looked at under the microscope to help decide whether problems such as inflammation, infection or cancer might be responsible for your symptoms. Bronchial lavage (described below) is also sometimes done during a bronchoscopy to help diagnose certain lung conditions.
To treat various problems
As mentioned, thin instruments can be passed down the side channel of a bronchoscope. Different instruments can do different things - for example:
To remove a small object (such as an inhaled peanut) that has been lodged in an airway.
To insert a small tube called a stent to open a blocked airway.
To remove a growth that is blocking an airway.
To take a small biopsy of a growth to see what it is.
Continue reading below
What happens during a bronchoscopy?
Back to contentsBronchoscopy using a flexible bronchoscope
This is usually done as an outpatient or day case. The doctor will numb the inside of your nose and the back of your throat by spraying on some local anaesthetic. This may taste a bit unpleasant. Also, you will normally be given a sedative to help you to relax.
This is usually given by an injection into a vein in the back of your hand or your arm. The sedative can make you drowsy but it is not a general anaesthetic and does not make you go to sleep.
However, you are unlikely to remember anything about the bronchoscopy if you have a sedative. You may be connected to a monitor to check your heart rate and blood pressure during the procedure.
A device called a pulse oximeter may also be put on a finger. This does not hurt. It checks the oxygen content of the blood and will indicate if you need extra oxygen during the bronchoscopy. You may have soft plastic tubes placed just inside your nostrils to give you oxygen during the procedure.
The doctor will insert the tip of the bronchoscope into one of your nostrils and then gently guide it round the back of your throat into your windpipe (trachea). (It is sometimes passed via your mouth rather than via your nose if you have narrow nasal passages). The bronchoscope may make you cough.
The doctor looks down the bronchoscope and inspects the lining of your trachea and main bronchi (the main airways). Bronchoscopes transmit pictures through a camera attachment on to a TV monitor for the doctor to look at.
The bronchoscope is then gently pulled out. Sometimes other procedures are done, these can include:
Biopsy
The doctor may take one or more samples (biopsies) of parts of the inside lining of the airways - depending on why the test is done and what they see. This is painless. The biopsy samples are sent to the laboratory for testing and to be looked at under the microscope.
Bronchial lavage
Sometimes bronchial lavage is done. This is a procedure where some fluid is squirted into a section of the lung and then syringed back. The fluid is then examined in the laboratory to look for abnormal cells and other particles that may be present in certain diseases.
Bronchoscopy using a rigid bronchoscopy
This requires a general anaesthetic, similar to that for minor operations. So, after receiving the anaesthetic, the next thing you know is when you wake up in a recovery room.
How long does a bronchoscopy take?
Back to contentsThe bronchoscopy itself usually takes about 20-30 minutes. However, you should allow at least two hours for the whole appointment, to prepare, give time for the sedative to work, for the bronchoscopy itself and to recover.
Continue reading below
Preparing for a bronchoscopy
Back to contentsYou may be advised not to take any medicines that affect blood clotting, such as aspirin and warfarin, for one week before the bronchoscopy. You will need to discuss your medication with your hospital doctor if you take such medicines for other conditions. It is up to the hospital doctor who has requested the test to decide whether you need to stop any medications in advance of the test, and you should not be directed back to the GP to make this decision. You will usually be asked to sign a consent form to indicate that you agree to have the test and have been counselled about the risks and benefits. You should have the opportunity to ask any questions that you want to, and you can bring someone with you if you feel that you need support.
In addition to this, you should receive instructions from the hospital before the test. These usually include:
That you should not eat or drink for several hours before the bronchoscopy. (Small sips of water may be allowed up to two hours before the test.)
That you will need somebody to accompany you home, as you will be drowsy with the sedative.
What can I expect after a flexible bronchoscopy?
Back to contentsIf you have a sedative, you may take an hour or so before you are ready to go home after the bronchoscopy is finished. The sedative will normally make you feel quite pleasant and relaxed. However, you should not drive, operate machinery or drink alcohol for 24 hours after having the sedative.
You should not eat or drink anything for two hours after the bronchoscopy because your throat will still be numb. You will need somebody to accompany you home and to stay with you for 24 hours until the effects have fully worn off. Most people feel able to resume normal activities after 24 hours.
The doctor may tell you what they saw before you leave. However, if you have had a sedative you may not remember afterwards what they said. Therefore, you may wish to have a relative or close friend with you who may be able to remember wha
What is a bronchoscopy?
Back to contentsA bronchoscopy is a test where a doctor looks into your lungs with a thin, plastic camera tube.
This photo shows a bronchoscope:
By Håkon Olav Leira (Own work) via Wikimedia Commons
A fibre-optic bronchoscope is the device usually used. This is a thin, flexible, telescope (shown in the diagram). It is about as thin as a pencil. You are usually awake during a bronchoscopy, but usually are sedated and made very sleepy. It may be uncomfortable but is not painful.
The bronchoscope is passed through your nose or mouth, down the back of your throat, into your windpipe (trachea), and down into your bronchi. The fibre-optics allow light to shine around bends in the bronchoscope and so the doctor can see clearly inside your airways.
A rigid bronchoscope (not shown in diagram) is used much less often. It is like a thin, straight telescope. It may be needed for some procedures and in children. It requires a general anaesthetic. (A fibre-optic bronchoscopy only requires sedation.)
Both types of bronchoscope have a side channel down which thin instruments can pass. For example, a thin grabbing instrument can pass down to take a small sample (biopsy) from the inside lining of an airway, or from structures next to the airways.
Who has a bronchoscopy?
Back to contentsTo help diagnose a problem
There are various reasons for having a bronchoscopy. For example, to help make a diagnosis if you have a persistent cough or cough up blood and the cause is not clear. If you have a shadow on a chest X-ray or the doctor sees a growth or a strange-looking area in a bronchus, the doctor may take a small sample (a biopsy) during a bronchoscopy.
The sample is then looked at under the microscope to help decide whether problems such as inflammation, infection or cancer might be responsible for your symptoms. Bronchial lavage (described below) is also sometimes done during a bronchoscopy to help diagnose certain lung conditions.
To treat various problems
As mentioned, thin instruments can be passed down the side channel of a bronchoscope. Different instruments can do different things - for example:
To remove a small object (such as an inhaled peanut) that has been lodged in an airway.
To insert a small tube called a stent to open a blocked airway.
To remove a growth that is blocking an airway.
To take a small biopsy of a growth to see what it is.
What happens during a bronchoscopy?
Back to contentsBronchoscopy using a flexible bronchoscope
This is usually done as an outpatient or day case. The doctor will numb the inside of your nose and the back of your throat by spraying on some local anaesthetic. This may taste a bit unpleasant. Also, you will normally be given a sedative to help you to relax.
This is usually given by an injection into a vein in the back of your hand or your arm. The sedative can make you drowsy but it is not a general anaesthetic and does not make you go to sleep.
However, you are unlikely to remember anything about the bronchoscopy if you have a sedative. You may be connected to a monitor to check your heart rate and blood pressure during the procedure.
A device called a pulse oximeter may also be put on a finger. This does not hurt. It checks the oxygen content of the blood and will indicate if you need extra oxygen during the bronchoscopy. You may have soft plastic tubes placed just inside your nostrils to give you oxygen during the procedure.
The doctor will insert the tip of the bronchoscope into one of your nostrils and then gently guide it round the back of your throat into your windpipe (trachea). (It is sometimes passed via your mouth rather than via your nose if you have narrow nasal passages). The bronchoscope may make you cough.
The doctor looks down the bronchoscope and inspects the lining of your trachea and main bronchi (the main airways). Bronchoscopes transmit pictures through a camera attachment on to a TV monitor for the doctor to look at.
The bronchoscope is then gently pulled out. Sometimes other procedures are done, these can include:
Biopsy
The doctor may take one or more samples (biopsies) of parts of the inside lining of the airways - depending on why the test is done and what they see. This is painless. The biopsy samples are sent to the laboratory for testing and to be looked at under the microscope.
Bronchial lavage
Sometimes bronchial lavage is done. This is a procedure where some fluid is squirted into a section of the lung and then syringed back. The fluid is then examined in the laboratory to look for abnormal cells and other particles that may be present in certain diseases.
Bronchoscopy using a rigid bronchoscopy
This requires a general anaesthetic, similar to that for minor operations. So, after receiving the anaesthetic, the next thing you know is when you wake up in a recovery room.
How long does a bronchoscopy take?
Back to contentsThe bronchoscopy itself usually takes about 20-30 minutes. However, you should allow at least two hours for the whole appointment, to prepare, give time for the sedative to work, for the bronchoscopy itself and to recover.
Preparing for a bronchoscopy
Back to contentsYou may be advised not to take any medicines that affect blood clotting, such as aspirin and warfarin, for one week before the bronchoscopy. You will need to discuss your medication with your hospital doctor if you take such medicines for other conditions. It is up to the hospital doctor who has requested the test to decide whether you need to stop any medications in advance of the test, and you should not be directed back to the GP to make this decision. You will usually be asked to sign a consent form to indicate that you agree to have the test and have been counselled about the risks and benefits. You should have the opportunity to ask any questions that you want to, and you can bring someone with you if you feel that you need support.
In addition to this, you should receive instructions from the hospital before the test. These usually include:
That you should not eat or drink for several hours before the bronchoscopy. (Small sips of water may be allowed up to two hours before the test.)
That you will need somebody to accompany you home, as you will be drowsy with the sedative.
What can I expect after a flexible bronchoscopy?
Back to contentsIf you have a sedative, you may take an hour or so before you are ready to go home after the bronchoscopy is finished. The sedative will normally make you feel quite pleasant and relaxed. However, you should not drive, operate machinery or drink alcohol for 24 hours after having the sedative.
You should not eat or drink anything for two hours after the bronchoscopy because your throat will still be numb. You will need somebody to accompany you home and to stay with you for 24 hours until the effects have fully worn off. Most people feel able to resume normal activities after 24 hours.
The doctor may tell you what they saw before you leave. However, if you have had a sedative you may not remember afterwards what they said. Therefore, you may wish to have a relative or close friend with you who may be able to remember what was said. The result from any sample (biopsy) may take a few days or weeks to come back.
Are there any bronchoscopy side-effects or complications?
Back to contentsMost are done without any problem. Your nose and throat may be a little sore for a day or so afterwards. You may feel tired or sleepy for several hours, caused by the sedative. There is a slightly increased risk of developing a throat or chest infection following a bronchoscopy.
If you had a biopsy taken, you may cough up a little blood a few times in the following day or so. Rarely, a bronchoscopy can cause damage to the lung. This is more likely to occur if a specialised sample (biopsy) of lung tissue is taken. Serious complications from a bronchoscopy are extremely rare, and only occur in around 1 in 1000 bronchoscopies.
t was said. The result from any sample (biopsy) may take a few days or weeks to come back.
Are there any bronchoscopy side-effects or complications?
Back to contentsMost are done without any problem. Your nose and throat may be a little sore for a day or so afterwards. You may feel tired or sleepy for several hours, caused by the sedative. There is a slightly increased risk of developing a throat or chest infection following a bronchoscopy.
If you had a biopsy taken, you may cough up a little blood a few times in the following day or so. Rarely, a bronchoscopy can cause damage to the lung. This is more likely to occur if a specialised sample (biopsy) of lung tissue is taken. Serious complications from a bronchoscopy are extremely rare, and only occur in around 1 in 1000 bronchoscopies.
Video picks for Endoscopy
Patient picks for Endoscopy

Surgery and procedures
Nasoendoscopy
A nasoendoscopy is a test to look inside the nose (nasal passage), the back of the throat (pharynx) and the voice box (larynx). It's sometimes called a flexible nasal endoscopy or FNE. Note: the information below is a general guide only. The arrangements and the way tests are performed may vary between different hospitals. Always follow the instructions given by your doctor or local hospital.
by Dr Doug McKechnie, MRCGP

Surgery and procedures
ERCP
ERCP is a procedure that uses an endoscope and X-rays to look at the bile duct and the pancreatic duct. ERCP can also be used to remove gallstones or take small samples of tissue for analysis (a biopsy). Note: the information below is a general guide only. The arrangements and the way tests are performed may vary between different hospitals. Always follow the instructions given by the doctor or local hospital.
by Dr Colin Tidy, MRCGP
Further reading and references
- Du Rand IA, Blaikley J, Booton R, et al; British Thoracic Society guideline for diagnostic flexible bronchoscopy in adults: accredited by NICE. Thorax. 2013 Aug;68 Suppl 1:i1-i44. doi: 10.1136/thoraxjnl-2013-203618.
Article history
The information on this page is written and peer reviewed by qualified clinicians.
Next review due: 12 May 2028
12 Jun 2023 | Latest version

Ask, share, connect.
Browse discussions, ask questions, and share experiences across hundreds of health topics.

Feeling unwell?
Assess your symptoms online for free
Sign up to the Patient newsletter
Your weekly dose of clear, trustworthy health advice - written to help you feel informed, confident and in control.
By subscribing you accept our Privacy Policy. You can unsubscribe at any time. We never sell your data.