Dysphagia
Difficulty swallowing
Peer reviewed by Dr Caroline Wiggins, MRCGP Last updated by Dr Rachel Hudson, MRCGPLast updated 20 Mar 2023
Meets Patient’s editorial guidelines
- DownloadDownload
- Share
- Language
- Discussion
- Audio Version
In this series:Globus sensation
There are various causes of dysphagia (difficulty swallowing). See your doctor as soon as possible if you develop dysphagia. This is because a serious condition such as cancer of the gullet (oesophagus) can be the cause. As a general rule, the earlier a serious problem is diagnosed, the better the chance that treatment may improve the outlook (prognosis). This leaflet discusses the main causes of dysphagia.
In this article:
Video picks for Swallowing difficulty
Continue reading below
What is dysphagia?
Dysphagia is the medical word for difficulty swallowing. People with dysphagia have problems swallowing certain solid foods or liquids, while others cannot swallow at all. This symptom is usually due to a problem of the gullet (oesophagus). Less commonly, a problem at the back of the mouth, or something pressing on the oesophagus, can cause this symptom. There is a range of different causes of dysphagia - discussed below.
The severity of dysphagia can vary from mild to severe. When mild, it can mean a feeling of food just taking longer to pass through the oesophagus and it can be painless. Liquids may well cause no problem. When severe, it can mean both solids and liquids do not pass at all down the oesophagus and may cause you to vomit back (regurgitate) food and drink. When moderate, it can be somewhere in between these extremes.
Dysphagia symptoms
Back to contentsSymptoms that may also occur as part of dysphagia, alongside difficulty swallowing, include:
Regurgitation of food or drink (vomiting) during or after eating or drinking.
Coughing during eating or drinking.
Choking during eating.
Pain on swallowing (odynophagia).
These symptoms may not occur if the dysphagia is mild. Over time dysphagia can also cause weight loss.
Symptoms that may occur at the same time as dysphagia are being sick, coughing, choking and pain swallowing

You should report any degree of dysphagia to your doctor - no matter how mild. Dysphagia is a symptom that always needs to be explained and diagnosed correctly. For example, the first symptom of cancer of the oesophagus (oesophageal cancer) is often mild, painless dysphagia that then gradually becomes worse over time.
So, this often needs to be ruled out or confirmed as the cause of the problem as soon as possible. As a general rule, the earlier a serious problem is diagnosed, the better the chance that treatment may improve the outlook (prognosis).
Continue reading below
Causes of dysphagia
Back to contentsThere are many possible causes. Broadly they can be divided into problems starting at the top of the swallowing process (in the oropharynx) and those caused by problems lower down in the gullet (oesophagus).
Below is a brief overview of the more common causes in each type of dysphagia.
Oropharyngeal causes of dysphagia
Back to contentsThese are the causes which are problems high up in the swallowing process just below the mouth.
Neurological problems
There are many muscle and nerve disorders (neurological diseases) that can affect the nerves and muscles in the gullet (oesophagus) to cause dysphagia. Because the nerves and muscles are not working properly, the food can't be manoeuvred normally to the top of the gullet. Difficulty swallowing as a result of these conditions can be common in elderly people, in some disabled people and in people who have had strokes. Examples of these neurological conditions include:
Severe learning disability.
However, in general, in these situations dysphagia would not be the first symptom to develop and various other symptoms would usually also be present.
Infections
For short periods of time, severe infections can cause difficulty in swallowing. For example, very swollen tonsils (bad tonsillitis or quinsy), an abscess at the back of the throat or very swollen lymph nodes.
Tumours and swellings
Tumours or swellings which press on the oropharynx can cause problems swallowing. This includes cancers of the mouth and throat, lumps or cancer of the thyroid gland, or cancers which cause swelling of the lymph nodes in the neck.
Pharyngeal pouch
A pharyngeal pouch is an uncommon condition where a dead end pouch (diverticulum) forms coming off the lowest part of the throat (the lower pharynx). Most occur in people over the age of 70. It may not cause any symptoms but can cause symptoms such as dysphagia, a sense of a lump in the neck, food regurgitation, cough and bad breath.
Breathing problems
Conditions causing difficulty breathing, particularly chronic obstructive pulmonary disease (COPD) can have a knock-on effect on swallowing.
Globus sensation
This is not a true cause of dysphagia but is mentioned here for completeness. Globus sensation is the term used when a person has the feeling of a lump in the back of their throat when actually there is no lump present when the throat is examined. Some people with this condition may have a feeling or perception of difficulty swallowing.
However, in this condition there is no true dysphagia, as you can eat and drink normally. Many people with globus sensation notice the symptoms most when they are swallowing their saliva. See the separate leaflet called Globus Sensation for more information.
Continue reading below
Oesophageal causes of dysphagia
Back to contentsStricture due to severe oesophagitis
Oesophagitis means inflammation of the lining of the gullet (oesophagus). Most cases of oesophagitis are due to acid reflux. Acid reflux occurs when some acid leaks up (refluxes) into the oesophagus from the stomach. The acid irritates the inside lining of the lower oesophagus to cause inflammation.
Gastro-oesophageal reflux disease (GORD) is a general term which describes the range of situations - acid reflux, with or without oesophagitis and symptoms. A complication of severe long-standing oesophagitis is scarring and narrowing (a stricture) of the lower oesophagus. Oesophagitis due to acid reflux is common, but a stricture causing difficulty swallowing (dysphagia) is an uncommon complication of this problem.
Eosinophilic oesophagitis
This is another type of inflammation of the oesophagus with a different cause and different treatment. It is an increasingly common cause of difficulty swallowing. See the separate leaflet called Eosinophilic Oesophagitis to read more about it.
Oesophageal cancer
Cancer of the oesophagus (oesophageal cancer) is uncommon in the UK. Most cases occur in people over the age of 55, although younger people are sometimes affected. Those diagnosed at an early stage have the best chance of a cure. Dysphagia is often the first symptom and is caused by the cancer growing and narrowing the passage in the oesophagus.
Strictures due to other causes
Although oesophagitis and cancer are the most common causes of oesophageal narrowings (strictures) there are various other causes - for example, following surgery or radiotherapy to the oesophagus. Various medicines and chemicals can irritate the oesophagus and cause a stricture.
Oesophageal webs and rings
These are abnormal non-cancerous overgrowths (extensions) of normal oesophageal tissue. They are uncommon. Their cause is not clear although oesophageal webs sometimes develop in people who have iron-deficiency anaemia. Webs and rings may not cause any symptoms but they sometimes cause dysphagia.
Achalasia
Achalasia is a condition that affects both the muscles and the nerves that control the muscles of the oesophagus. Achalasia typically first affects the nerves that cause the sphincter between the oesophagus and stomach to relax. The muscles then do not contract properly to push food down.
In addition, the sphincter does not relax properly so food cannot pass through into your stomach easily. This makes it difficult for you to swallow food properly. It mainly affects adults aged between 20-40 years. In most cases, no underlying cause can be found and the reason why the nerves and muscles in the oesophagus do not work so well is not clear.
Muscle disorders
Conditions which affect the smooth muscle or connective tissues of the oesophagus, preventing it from working properly, can cause difficulty swallowing. Examples include scleroderma and myositis.
Pressure from outside the oesophagus
Pressure from structures next to the oesophagus can sometimes affect the function of the oesophagus to cause dysphagia. For example, cancer of the thyroid, lung, stomach or spine, or a large aortic aneurysm may press on the oesophagus. Again, other symptoms would normally have developed before the dysphagia.
Other causes
These include various rare conditions that cause inflammation or reduced function of the oesophagus; infections of the oesophagus or swallowing large objects that get stuck (more common in children).
What should I do if I have dysphagia?
Back to contentsSee a doctor promptly. It is very important to obtain a correct diagnosis as soon as possible.
What tests might be advised?
Back to contentsIt depends on the possible causes of the difficulty swallowing (dysphagia), which may be determined by a doctor talking to you (your history) and an examination. Two of the most common tests done when someone has dysphagia are endoscopy and barium swallow.
Endoscopy
This is a test where an operator (a doctor or nurse) looks into the upper part of your gut (the upper gastrointestinal tract). An endoscope is a thin, flexible telescope. It is about as thick as a little finger. The endoscope is passed through the mouth or nose, into the oesophagus and down towards the stomach and duodenum.
The tip of the endoscope contains a light and a tiny video camera so the operator can see inside your gullet (oesophagus), stomach and duodenum. The endoscope also has a side channel down which various instruments can pass. These can be manipulated by the operator. For example, the operator may take a small sample (biopsy) from the inside lining of the oesophagus by using a thin grabbing instrument which is passed down a side channel.
See the separate leaflet called Gastroscopy (Endoscopy) for more details.
Barium swallow
This is a test that helps to look for problems in the oesophagus. The oesophagus and other parts of the gut do not show up very well on ordinary X-ray pictures. However, if you drink a white liquid that contains a chemical called barium sulfate, the outline of the upper parts of the gut (oesophagus, stomach and small intestines) shows up clearly on X-ray pictures. This is because X-rays do not pass through barium.
See the separate leaflet called Barium Tests (Swallow, Meal, Follow Through) for more details.
Other tests
The following tests may be considered:
Oesophageal manometry - this is a test where a pressure-sensitive tube is passed via your nose or mouth into your oesophagus to measure the pressure of the muscle contractions in the oesophagus.
Videofluoroscopy - this is a bit like a barium swallow. Different drinks and foods are mixed with barium and you are asked to do various things like swallow, move your head, etc, after drinking or eating the mixture. X-ray pictures are taken and your swallowing can be examined.
pH monitoring - during this test, a thin tube is passed through your nose or mouth and into your oesophagus. A monitor that is attached to the tube can measure the pH (acid level) in your oesophagus.
Scans such as a magnetic resonance imaging (MRI) scan.
It is very important to obtain a correct diagnosis as soon as possible

Dysphagia treatment
Back to contentsThe treatment for dysphagia depends on the cause. Follow the links to individual leaflets on the various diseases that can cause difficulty swallowing (dysphagia). Speech and language therapy assessment and treatment can be very useful, especially when treating patients who have had strokes, have dementia or who have other oropharyngeal causes for their dysphagia. Medication may need adjusting if it is difficult to swallow tablets. Often there is an alternative form, such as a liquid, patch or injection.
What are the complications of dysphagia?
Back to contentsSwallowing disorders may make it difficult to take in enough food and/or drink, resulting in malnutrition or lack of fluid in the body (dehydration). It may make it difficult to take necessary medication, which may go on to cause further medical problems. It leads to a risk of food 'going down the wrong way' (aspiration) towards the lungs instead of the stomach. This can cause choking or pneumonia.
Understanding swallowing
Back to contentsThe oropharynx and oesophagus
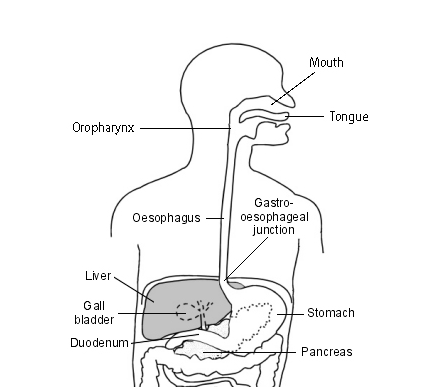
Swallowing is a complex process. The journey of our food from our plate to our tummy (stomach) starts in the mouth. The muscles of the tongue and mouth move the food to the back of the mouth, and then to the back of the throat. This area is the oropharynx. From here the food travels down to the upper gut.
The gullet (oesophagus) is part of the gut (gastrointestinal tract). When we eat, food goes down the oesophagus into the stomach.
The upper section of oesophagus lies behind the windpipe (trachea). The lower section lies between the heart and the spine.
There are layers of muscle in the wall of the oesophagus. These contract to push food down into the stomach. The inner lining of the oesophagus (the oesophageal mucosa and submucosa) is made up of layers of various types of cells and some tiny glands that make mucus. The mucus helps the food to pass through smoothly.
There is a thickened circular band of muscle (a sphincter) at the junction between the oesophagus and stomach. This relaxes to allow food down, but normally tightens up and stops food and acid leaking back up (refluxing) into the oesophagus. In effect, the sphincter acts like a valve.
Patient picks for Swallowing difficulty

Oral and dental care
Globus sensation
Globus sensation is the feeling of having a lump in the throat when in fact there is nothing there. The sensation can come and go and does not interfere with eating and drinking. The exact cause of globus sensation is uncertain. Examination and investigations may be carried out to exclude any other underlying problem. Reassurance that there is no serious underlying problem may be all that is needed in terms of treatment.
by Dr Philippa Vincent, MRCGP

Oral and dental care
Achalasia
Achalasia is an uncommon condition that affects the muscles of the gullet (oesophagus). It usually causes difficulty in swallowing both food and fluids. There are different treatments available which can improve symptoms.
by Dr Colin Tidy, MRCGP
Further reading and references
- Dysphagia; World Gastroenterology Organisation (WGO) guideline, Sept 2014
- Guideline on the medication management of adults with swallowing difficulties; Working party guideline, September 2015
Continue reading below
Article history
The information on this page is written and peer reviewed by qualified clinicians.
Next review due: 16 Feb 2028
20 Mar 2023 | Latest version
5 Nov 2012 | Originally published
Authored by:
Dr Tim Kenny, MRCGP

Ask, share, connect.
Browse discussions, ask questions, and share experiences across hundreds of health topics.

Feeling unwell?
Assess your symptoms online for free
Sign up to the Patient newsletter
Your weekly dose of clear, trustworthy health advice - written to help you feel informed, confident and in control.
By subscribing you accept our Privacy Policy. You can unsubscribe at any time. We never sell your data.