Middle ear infection (otitis media)
Peer reviewed by Dr Rachel Hudson, MRCGPLast updated by Dr Philippa Vincent, MRCGPLast updated 21 Sept 2023
Meets Patient’s editorial guidelines
- DownloadDownload
- Share
- Language
- Discussion
In this series:EaracheEustachian tube dysfunctionOuter ear infection (otitis externa)Fungal ear infectionBoil in the ear canalBarotrauma to the ear
Ear infection is very common in children although it can occur in people of any age. The main symptoms are earache and feeling unwell. Painkillers are the main treatment. Antibiotics are not usually helpful but are prescribed in some cases. The infection usually clears within a few days.
In this article:
Video picks for Ear infections
What is an ear infection?
What are ear infections?
Ear infections are usually divided into those which occur in the ear canal (otitis externa) and those which occur in the small space behind the eardrum (the middle ear). An infection of the middle ear may be referred to as 'acute otitis media'.
This leaflet deals with infections of the middle ear.
How common is an ear infection?
Back to contentsEar infections are very common in children. Middle ear infections are much less common in adults. They are most common between the ages of six months and 2 years. Most children will have two or more episodes of otitis media before they are five years' old. 9 out of 10 children will have had an ear infection before they start school. Some children seem more prone to ear infections and get them more frequently.
Continue reading below
Ear infection symptoms
Back to contentsEar pain (earache) is common but does not always occur. It is caused by having a tense, inflamed eardrum.
Dulled hearing may be present for a few days.
High temperature (fever) is common.
Children may feel sick or be sick (vomit) and be generally unwell.
Young babies may be hot and irritable. A hot, crying baby may have an ear infection.
Sometimes the eardrum bursts (perforates). This lets out the infected fluid (mucus) and often relieves pain quite suddenly. The ear becomes runny, sometimes for a few days. Most perforations are small. A perforated eardrum usually heals within a few weeks after the infection clears.
A note about earache
Earache is a common symptom of ear infection. However, not all earaches are caused by an ear infection. If a child has earache but is otherwise well, an ear infection is unlikely.
Mild earache is often due to a build-up of mucus in the middle ear after a cold. This usually clears within a few days. Pain in the ear can also be referred pain from other causes such as tooth problems or the jaw joint.
The National Institute for Health and Care Excellent (NICE) recommends that a health care professional should review the ear if the symptoms have not improved after a week or if they are getting worse. Sometimes ear drops with a local anaesthetic and painkillers might be prescribed instead of antibiotics.
How does an ear infection occur?
Back to contentsOtitis media
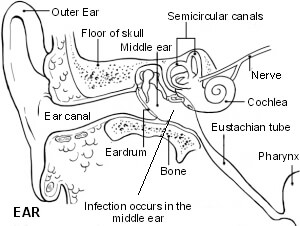
The small space behind the eardrum in the middle ear is normally filled with air. It is connected to the back of the throat by a tiny channel called the Eustachian tube. It also contains the three tiny 'hearing bones' which pass sound through from the eardrum to the inner ear.
The middle ear space should contain air but it may become filled with fluid (mucus), which typically occurs during a cold. The mucus may then become infected by germs (bacteria or viruses). This may then lead to otitis media.
Children with glue ear have mucus permanently trapped behind their eardrum and they are more prone to ear infections. Sometimes an ear infection occurs 'out of the blue' for no apparent reason.
Continue reading below
Diagnosing an ear infection
Back to contentsAn ear infection normally presents with pain and fever. These symptoms should be treated with anti-inflammatory painkillers for at least 48 hours before seeking medical help in an otherwise well child over the age of two years. If medical advice is sought, a clinician will use a torch to look into the ear and see if the ear drum is red or bulging. Antibiotics will sometimes be recommended if the symptoms have been persistent for more than 48 hours. Sometimes a prescription for antibiotics will be given to be started if the symptoms have not resolved in another three days.
Ear infection treatment
Back to contentsMost ear infections get better without any treatment. Recovery usually takes place within three days but can take up to a week. Paracetamol or ibuprofen might be needed to treat fever or pain symptoms. Most ear infections don't need antibiotics.
The immune system can usually clear germs (bacteria or viruses) that cause ear infections. Treatments that may be advised to help with the symptoms include the following:
Painkillers
If the ear infection is causing pain then painkillers can be used regularly until the pain eases. For example, paracetamol (eg, Calpol®) or ibuprofen (eg, Calprofen®). These medicines will also lower a raised temperature, which can make a child feel better. If antibiotics are prescribed (see below), the painkillers should still be given as well until the pain eases.
Research studies have found that a few drops of a local anaesthetic medication (lidocaine) placed into the ear may help to ease pain. NICE now recommends this as a possible treatment option.
Antibiotics - are prescribed in some cases only
Antibiotics are not advised in most cases. This is because the infection usually clears within three days on its own and antibiotics make little or no difference to the speed of this. There are many good reasons not to take antibiotics.
Antibiotics may cause side-effects such as runny stools (diarrhoea) or rash. They also eradicate 'friendly bacteria' from the gut, which can temporarily upset the digestive balance. Many children feel less well whilst taking antibiotics. Overuse of antibiotics encourages resistant bugs to breed.
Antibiotics are unlikely to be helpful or justified if:
The child is 2 years old or more with a temperature of 39°C or less.
The child is not severely distressed.
The child has been unwell for three days or less.
Despite all this there are occasions when antibiotics are needed. Antibiotics are more likely to be prescribed if:
The child is under 2 years old and has an infection in both ears (as the risk of complications is greater in babies).
The child or young adult has a discharge coming from the ear.
The infection is severe.
The infection is not settling within three days.
Complications develop.
The child has another medical condition (for example, diabetes) which might increase the risk of infection.
When an ear infection first develops it is common to use a 'wait and see' approach for three days. This means just using painkillers to ease the pain and to see if the infection clears. In most cases, the infection does clear. However, if it doesn't clear then, following a review by a doctor, an antibiotic may be advised.
Complications of ear infections
Back to contentsHearing loss causes by fluid (mucus) remaining behind the eardrum after the infection clears.
Glue ear.
Repeated ear infections (for example, due to having several colds in a row).
Burst (perforated) eardrum.
Seek medical advice if dulled hearing persists for more than a few days after an ear infection has gone or if a child is suspected to be having difficulty hearing.
If the eardrum bursts (perforates) then it usually heals over within a few weeks once the infection clears. Occasionally the perforation remains long-term and may need treatment to fix it.
If a child is normally healthy then the risk of other serious complications developing from an ear infection is very small. Rarely, a serious infection of the bone behind the ear develops from an ear infection. This is called mastoiditis.
Very rarely, the infection spreads deeper into the inner ear, brain or other nearby tissues. This can cause various symptoms that can affect the brain and nearby nerves, including abscess and meningitis. Medical advice should always be sought if a child with earache:
Becomes suddenly or significantly more ill.
Has an illness which seems severe.
Does not improve over three days.
Has a temperature above 39°C. A fever like this is not generally considered a danger to your child. Children develop high temperatures in many common illnesses, including ear infections, urinary tract infections, roseola (a common childhood virus) and flu. However, when the temperature is above 39°C a child is more likely to have an illness or infection that needs your doctor's help. (If a child is under 3 months old then medical advice should be sought if their temperature is above 38°C).
Develops any symptoms that seem unusual.
Preventing ear infections
Back to contentsThere is generally nothing that can be done to prevent the infection from occurring. However, there is some evidence to suggest that an ear infection is less likely to develop:
In breastfed children.
In children who live in a smoke-free home. (Passive smoking of babies and children can increase the risk of developing ear infections.)
In babies and young children who do not use dummies. However, research studies have shown that the use of a dummy in young babies when settling to sleep possibly reduces the risk of cot death. Some experts advise using a dummy at the start of any sleep period in babies under the age of 6-12 months once breastfeeding has been well established (approximately one month of age). However not all experts agree that the evidence is good enough to advise the use of dummies.
Recurring ear infections
Back to contentsOccasionally, some children have recurring bouts of ear infections close together. If this occurs, a specialist may advise a long course of antibiotics to prevent further bouts from occurring.
If infections are very frequent, a specialist may advise the insertion of a grommet into the eardrum. This is the same treatment that is used to treat some cases of glue ear. A grommet is a tiny drainage pipe that helps to let fluid escape from the middle ear, and that lets air in. Some research suggests that this may reduce the number of ear infections that occur. See the separate leaflet called Glue Ear for more details.
Most children have at least two bouts of ear infection before they are 5 years old. These are caused by common viral infections which circulate in the general population and against which a child is not immune.
Dr Mary Lowth is an author or the original author of this leaflet.
Patient picks for Ear infections
Ear, nose and throat
Fungal ear infection
Fungal ear infection is an infection of the ear with a fungus. It normally involves the ear canal that runs from the ear hole to the eardrum (the external auditory canal). The medical term for it is otomycosis.
by Dr Surangi Mendis, MRCGP
/og.png)
Ear, nose and throat
Outer ear infection (otitis externa)
Otitis externa, more commonly known as an outer ear infection, is an inflammation of the ear canal. The inflammation is usually caused by infection, although it can sometimes be due to allergy or irritation. Treatment with ear drops is usually effective. Further episodes of the condition can often be prevented using the tips given below. Otitis externa usually clears within a week or so. When it is short-lasting, this is described as 'acute otitis externa'. However, occasionally it may persist for three months or more - this is described as 'chronic otitis externa'.
by Dr Colin Tidy, MRCGP
Further reading and references
- Otitis media (acute): antimicrobial prescribing; NICE Guideline (2018, updated March 2022)
- Meherali S, Campbell A, Hartling L, et al; Understanding Parents' Experiences and Information Needs on Pediatric Acute Otitis Media: A Qualitative Study. J Patient Exp. 2019 Mar;6(1):53-61. doi: 10.1177/2374373518771362. Epub 2018 Apr 24.
- Danishyar A, Ashurst JV; Acute Otitis Media
Continue reading below
Article history
The information on this page is written and peer reviewed by qualified clinicians.
Next review due: 19 Sept 2028
21 Sept 2023 | Latest version

Ask, share, connect.
Browse discussions, ask questions, and share experiences across hundreds of health topics.

Feeling unwell?
Assess your symptoms online for free
Sign up to the Patient newsletter
Your weekly dose of clear, trustworthy health advice - written to help you feel informed, confident and in control.
By subscribing you accept our Privacy Policy. You can unsubscribe at any time. We never sell your data.