Spinal stenosis
Peer reviewed by Dr Caroline Wiggins, MRCGP Last updated by Dr Rosalyn Adleman, MRCGPLast updated 24 Jul 2025
Meets Patient’s editorial guidelines
- DownloadDownload
- Share
- Language
- Discussion
- Audio Version
In this series:Back and spine painLower back painSlipped discCauda equina syndromeThoracic back painBack pain in children
Spinal stenosis is a term used to describe a narrowing of your spinal canal. The narrowing may not cause any symptoms. However, the narrowing may progress to cause squeezing (compression) of your spinal nerves or compression of your spine. Spinal stenosis causes back pain and leg pain. Most often it occurs when you walk. Weakness of the legs may make you feel unsteady. This may affect both legs or just one leg. Spinal stenosis affecting the cervical spine in your neck may also cause pain and weakness in the shoulders and arms.
Spinal stenosis can often be treated by simple measures such as medicines for pain relief, keeping as active as you can and losing weight if you are overweight. Sometimes steroid injections or surgery are suggested if simple measures are not successful.
In this article:
Video picks for Back and spine
Continue reading below
What is spinal stenosis?
Spinal stenosis is a term used to describe a narrowing of your spinal canal. The narrowing may not cause any symptoms. However, the narrowing may progress to cause squeezing (compression) of your spinal nerves or compression of your spine. Narrowing that affects your spinal cord is sometimes called a myelopathy. More than one level of your spine may be affected. The blood supply to the nerves in your spine may also be temporarily reduced by the compression.
The lower end of your spinal cord is at the level of the first or second lumbar bone (vertebra). The nerves from your spinal cord then form a structure called the conus medullaris. The spinal nerves continue to branch out below the conus medullaris to form the cauda equina.
Pressure on your cauda equina causes cauda equina syndrome. Cauda equina syndrome may cause low back pain and problems with your bowel and bladder function, numbness in your saddle area, which is around the back passage (anus), and weakness in one or both legs. Cauda equina syndrome needs urgent investigation and treatment to prevent the nerves to your bladder and bowel from becoming permanently damaged.
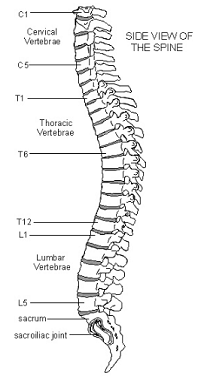
Understanding the back
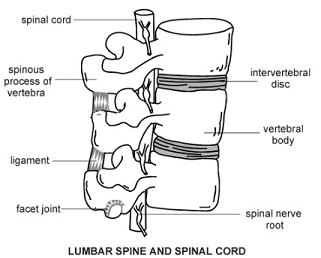
Your spine is made up of many bones called vertebrae. These are roughly circular and between each vertebra is a disc. The discs are made of strong rubber-like tissue which allows your spine to be fairly flexible. A disc has a stronger fibrous outer part and a softer jelly-like middle part called the nucleus pulposus.
Your spinal cord, which contains the nerves that come from your brain, is protected by your spine. Nerves from your spinal cord come out from between your vertebrae to relay messages to and from various parts of your body.
Spinal cord
Close-up diagram lumbar spinal cord
Spinal stenosis causes
Back to contentsAs you get older, degenerative changes occur in your spine, especially in your lower back and neck. Sometimes this causes partial compression (stenosis) of the nerve tunnel within your spine. This is called central stenosis. Sometimes there is a constriction to the smaller side tunnels within your spine. This is called foraminal stenosis.
Continue reading below
How common is spinal stenosis?
Back to contentsSpinal stenosis is common, especially in older people. However, it can also rarely affect younger people. Spinal stenosis most often affects your lower (lumbar) spine. The next most commonly affected part of your spine is the cervical spine in your neck. Stenosis of the spine at the back of your chest (thoracic spine) is much less common.
Spinal stenosis symptoms
Back to contentsSymptoms of spinal stenosis include back pain and leg pain. This often occurs when you walk. Weakness of the legs may make you feel unsteady. This may affect both your legs or just one leg. Spinal stenosis affecting your cervical spine may also cause pain and weakness in your shoulders and arms.
Claudication is the term used to describe pain, weakness or numbness of your legs that becomes worse specifically on walking. Claudication is caused either by narrowing of the blood vessels supplying the leg or because of spinal stenosis.
Usually spinal stenosis prevents you from walking beyond a certain distance. You then have to stop because of increasing pain and numbness in one or both of your legs. The symptoms can also occur when standing. Usually the symptoms reduce if you sit down or lean forwards. There is usually no pain when you are resting.
Walking usually only aggravates your leg symptoms. The back pain caused by spinal stenosis does not increase with walking.
Continue reading below
What tests are used to diagnose spinal stenosis?
Back to contentsIf your doctor thinks that you may have spinal stenosis then an MRI scan may be needed to confirm the diagnosis.
What is the treatment for spinal stenosis?
Back to contentsHow you can help to improve your own symptoms
Maintain activity as much as you can. Try to gradually increase the distance you walk if you can.
Massage and heat treatments.
Physiotherapy. You may be able to self-refer for this, or your doctor may refer you. There is evidence from scientific trials that manual therapy and exercise is an effective treatment.
Pain relief. Using over-the-counter medication such as paracetamol or ibuprofen may be sufficient.
Other medicines prescribed by your doctor can be used if over-the-counter medicines do not provide enough pain relief. Some medicines can be used specifically to help the nerve pain in your legs - for example, amitriptyline, gabapentin or pregabalin.
Other available treatments
Spinal injections: injections of a steroid with local anaesthetic given into your spinal root canal or given by epidural injections can be helpful.
Surgery: if symptoms still do not improve then one option is surgery. The most commonly used operation is called a decompression. The bone that is compressing the nerves is removed so that the nerves have more room. The two bones (vertebrae) may also be fused together (this is called spinal fusion).
There is very limited evidence for surgery to treat spinal stenosis. The success of surgery for spinal stenosis is variable. Although your symptoms may improve just after the operation, the medium-term and long-term results can be disappointing.
Interspinous distraction: this procedure involves placing an implant between the spinous processes of the affected vertebrae (usually the fourth and fifth lumbar vertebrae) in order to limit you extending your back. This helps to prevent or reduce the pain in your legs when standing or walking.
What is the outcome (prognosis)?
Back to contentsThe outcome is variable and, without treatment, the symptoms usually gradually become worse. Although treatments for spinal stenosis are often effective at reducing symptoms, the symptoms don't always completely resolve. Many people can cope with their symptoms, as time can allow the nerves to adapt.
Patient picks for Back and spine

Bones, joints and muscles
Cervical spondylosis
This leaflet is aimed at people who have been told they have cervical spondylosis as a cause of their neck symptoms. Cervical spondylosis is a 'wear and tear' of the vertebrae and discs in the neck. It is a normal part of ageing and does not cause symptoms in many people. However, it is sometimes a cause of neck pain. Symptoms tend to come and go. Treatments include keeping the neck moving, neck exercises and painkillers. In severe cases, the degeneration may cause irritation or pressure on the spinal nerve roots or spinal cord. This can cause arm or leg symptoms (detailed below). In these severe cases, surgery may be an option.
by Dr Doug McKechnie, MRCGP

Bones, joints and muscles
Axial spondyloarthritis
Axial spondyloarthritis (also known as axSpA or axial SpA) is a painful, chronic arthritis that mainly affects the joints of the spine, and also the joints connecting each side of the base of the spine with the pelvis (sacroiliac joints). It can also affect other joints in the body, as well as tendons and ligaments. It is divided into: 1) Ankylosing spondylitis. 2) Non radiographic axial spondyloarthritis.
by Dr Philippa Vincent, MRCGP
Further reading and references
- Interspinous distraction procedures for lumbar spinal stenosis causing neurogenic claudication; NICE Interventional procedure guidance, November 2010
- Zaina F, Tomkins-Lane C, Carragee E, et al; Surgical versus non-surgical treatment for lumbar spinal stenosis. Cochrane Database Syst Rev. 2016 Jan 29;(1):CD010264. doi: 10.1002/14651858.CD010264.pub2.
- Kato S, Fehlings M; Degenerative cervical myelopathy. Curr Rev Musculoskelet Med. 2016 Sep;9(3):263-71. doi: 10.1007/s12178-016-9348-5.
- Bagley C, MacAllister M, Dosselman L, et al; Current concepts and recent advances in understanding and managing lumbar spine stenosis. F1000Res. 2019 Jan 31;8. doi: 10.12688/f1000research.16082.1. eCollection 2019.
- Raja A, Hoang S, Patel P, et al; Spinal Stenosis. StatPearls, Jan 2022.
- Ammendolia C, Hofkirchner C, Plener J, Bussières A, Schneider MJ, Young JJ, Furlan AD, Stuber K, Ahmed A, Cancelliere C, Adeboyejo A, Ornelas J. Non-operative treatment for lumbar spinal stenosis with neurogenic claudication: an updated systematic review. BMJ Open. 2022 Jan 19;12(1):e057724. doi: 10.1136/bmjopen-2021-057724.
Continue reading below
Article history
The information on this page is written and peer reviewed by qualified clinicians.
Next review due: 3 Jul 2028
24 Jul 2025 | Latest version
22 Feb 2017 | Originally published
Authored by:
Dr Colin Tidy, MRCGP

Ask, share, connect.
Browse discussions, ask questions, and share experiences across hundreds of health topics.

Feeling unwell?
Assess your symptoms online for free
Sign up to the Patient newsletter
Your weekly dose of clear, trustworthy health advice - written to help you feel informed, confident and in control.
By subscribing you accept our Privacy Policy. You can unsubscribe at any time. We never sell your data.