Liver disease and alcohol
Effects of alcohol abuse
Peer reviewed by Dr Colin Tidy, MRCGPLast updated by Dr Doug McKechnie, MRCGPLast updated 18 Feb 2023
Meets Patient’s editorial guidelines
- DownloadDownload
- Share
- Language
- Discussion
- Audio Version
In this series:Alcohol and sensible drinking - safe limits of alcoholAlcoholism and problem drinkingAlcohol withdrawal and alcohol detoxification Non-alcoholic fatty liver disease
Alcohol abuse can lead to three main types of liver diseases: fatty liver, hepatitis and 'scarring' of the liver (cirrhosis). It can also lead to other health problems. This leaflet also includes information about non-alcoholic fatty liver disease.
In this article:
Video picks for Alcohol advice
What is alcoholic liver disease?
Many of us enjoy an occasional alcoholic drink. It's been suggested that a small amount of alcohol might be good for health. People who drink 1-2 units a day are statistically at a slightly lower risk of heart attack than teetotallers - although it's debated as to whether this is due to a protective effect of alcohol, or something else.
However, drinking any amount of alcohol regularly increases the risk of cancer; this risk is small, but present, with low levels of alcohol consumption, and increases substantially with heavy alcohol use. Heavy alcohol use can also lead to liver disease.
Continue reading below
How much alcohol is too much?
It's debated as to whether any amount of alcohol is safe. The World Health Organization states that there is no safe level of alcohol consumption for health. However, for people who do drink, it's thought that sticking to the recommended maximum limits keeps the risks relatively low. Drinking above the recommended limits significantly increases the risk of health problems.
In the UK, the Chief Medical Officer recommends sticking to a maximum of 14 units a week, spread over three or more days, and with a few alcohol-free days each week.
You can see how many units you are drinking by using our alcohol units calculator.
Symptoms of liver disease
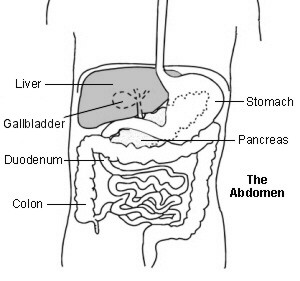
Back to contentsThe liver is in the upper right part of the tummy (abdomen), just below the ribs.
Liver function
Drinking too much alcohol leads to three main conditions which can seriously threaten your health:
Fatty liver.
Hepatitis.
'Scarring' of the liver (cirrhosis).
Any, or all, of these liver diseases can occur at the same time in the same person.
If you have early-stage liver disease (fatty liver or mild hepatitis), you may not get any symptoms. As the condition progresses, you may gradually develop symptoms such as:
Feeling sick (nausea), being sick (vomiting) and feeling generally unwell.
Abdominal pain and swelling.
Swelling of your ankles and lower legs.
Itchy skin.
Your urine becoming dark in colour.
Your stools (faeces) becoming pale or very dark/black because of bleeding into the upper part of your gut (bowel).
Continue reading below
Fatty liver
Back to contentsA build-up of fat occurs within liver cells in most people who regularly drink heavily. In itself, fatty liver is not usually serious and does not cause symptoms. Fatty liver will usually reverse if you stop drinking heavily. However, in some people the fatty liver progresses and develops into alcoholic hepatitis.
A similar condition can occur in people who don't drink a lot of alcohol. Read more about non-alcoholic fatty liver disease.
Alcoholic hepatitis
Back to contentsHepatitis means inflammation of the liver. The inflammation can range from mild to severe.
Mild hepatitis may not cause any symptoms. The only indication of inflammation may be an abnormal level of liver chemicals (enzymes) in the blood, which can be detected by a blood test. However, in some cases the hepatitis becomes persistent (chronic), which can gradually damage the liver and eventually cause cirrhosis (permanent scarring of the liver).
A more severe hepatitis tends to cause symptoms such as:
Feeling sick (nausea).
Yellowing of your skin or the whites of your eyes (jaundice), caused by a high level of bilirubin - a chemical normally metabolised in the liver.
Generally feeling unwell.
Sometimes, pain over the liver.
A very severe bout of alcoholic hepatitis can quickly lead to liver failure. This can cause deep jaundice, blood clotting problems, confusion, coma and bleeding into the guts. It is often fatal.
The main short-term treatment for alcoholic hepatitis is to provide adequate nutrition (this sometimes involves passing liquid feeds through a tube in the stomach) and, sometimes, steroids. In the longer term, avoiding alcohol completely is very important to prevent further liver damage.
Continue reading below
Alcoholic cirrhosis
Back to contentsCirrhosis is a condition where normal liver tissue is replaced by scar tissue (fibrosis). The scarring tends to be a gradual process. The scar tissue affects the normal structure and regrowth of liver cells. Liver cells become damaged and die as scar tissue gradually develops. So, the liver gradually loses its ability to function well. The scar tissue can also affect the blood flow through the liver which can cause back pressure in the blood vessels which bring blood to the liver.
About 1 in 10 heavy drinkers will eventually develop cirrhosis. It tends to occur after 10 or more years of heavy drinking. Cirrhosis can also develop in people who have never had alcoholic hepatitis.
Cirrhosis can happen from many causes other than alcohol. If you have another persistent liver disease and drink heavily, you are likely to increase your risk of developing cirrhosis.
Cirrhosis can lead to end-stage liver disease. End-stage liver disease is fatal. However, in the early stages of the condition, often there are no symptoms. You can get by with a reduced number of working liver cells. But, as more and more liver cells die and more and more scar tissue builds up, symptoms start to appear. The eventual symptoms and complications are similar to a severe episode of hepatitis (listed above). However, unlike a bout of severe hepatitis, the symptoms and complications tend to develop slowly. The scarring and damage of cirrhosis is usually permanent and cannot be reversed. Cirrhosis also increases the risk of developing liver cancer. See the separate leaflet called Cirrhosis for more details.
What happens when you drink alcohol?
Back to contentsWhen you drink alcohol, it is absorbed into the bloodstream from the stomach and intestines. All blood from the stomach and intestines first goes through the liver before circulating around the whole body. So, the highest concentration of alcohol is in the blood flowing through the liver.
Liver cells contain chemicals (enzymes) which process (metabolise) alcohol. The enzymes break down alcohol into other chemicals which in turn are then broken down into water and carbon dioxide. These are then passed out in the urine and from the lungs. The liver cells can process only a certain amount of alcohol per hour. So, if you drink alcohol faster than your liver can deal with it, the level of alcohol in your bloodstream rises.
What are the problems of drinking too much alcohol?
Back to contentsIt's thought that there is no level of alcohol consumption that is completely safe; drinking even a small amount regularly increases the risk of health problems like cancer. It's previously been suggested that moderate alcohol use might reduce the risk of heart disease, but more recent evidence has put this in doubt.
Drinking within the recommended maximum limits, though, is thought to have a low risk of significant health problems.
Drinking over the recommended limits can be harmful. In the UK, alcohol poisoning deaths (particularly liver disease) have risen considerably over a period of 20 years. Read more about alcoholism and problem drinking.
Signs of alcohol poisoning
Back to contentsThe symptoms and signs of alcohol poisoning are very variable but include:
Being sick (vomiting).
Confusion and reduced level of consciousness (may pass out).
Fits (seizures).
Irregular or slow breathing.
Low body temperature.
What tests will I need?
Back to contentsA doctor may suspect that you have liver problems from your symptoms and from a physical examination - for example, they may detect that your liver is enlarged, or that you are retaining fluid. They may especially think of liver problems as a cause of your symptoms if you have a history of heavy alcohol drinking. Some tests may be done:
Blood tests may show abnormal liver function
There are a number of liver function tests (LFTs) that look at levels of various chemicals in the liver. These tests show two different things: some show evidence of damage or inflammation in the liver, and others show if the liver is actually working properly. Signs of damage can be seen much earlier; the liver usually only stops working properly if there has been a lot of damage. Even though a number of different LFTs are tested, you only need to give one blood sample for all of them.
A blood test to check how well your blood clots
Helping your blood to clot is one of the functions of the liver. If the liver is no longer working properly, blood clotting abnormalities can been seen on this blood test. Abnormal blood clotting suggests advanced liver damage.
A blood test for anaemia
People with alcohol problems can be deficient in a vitamin called vitamin B12, which can lead to anaemia.
A blood test for liver scarring
A blood test called the Enhanced Liver Fibrosis (ELF®) test is sometimes done to look for signs of liver scarring (fibrosis). If the blood test is raised, it usually means that someone should be referred to a liver specialist for further tests.
Ultrasound scan
An ultrasound scan may show that you have a damaged liver. This painless test is the same type as pregnant women have when their baby is being checked. Some lubricating jelly is placed on the skin of the tummy over the liver, and a handheld ultrasound scanner is moved across the skin. This shows an image of the liver on a monitor and liver damage or enlargement can be seen. However, signs of cirrhosis on ultrasound may not be visible in the early stages.
People with cirrhosis may be offered regular surveillance (check-up) ultrasound scans to look for early signs of liver cancer.
FibroScan® (transient elastography)
This is a special type of ultrasound scan that measures the stiffness of the liver, and is a better way of detecting and measuring scarring and cirrhosis. In the UK, it's currently offered by liver specialists; the ELF® blood test can help to determine who should be referred for one of these scans.
A small sample (biopsy) of the liver
This may be taken to be looked at under the microscope and so confirm the diagnosis. The 'scarring' of the liver caused by liver damage (cirrhosis), or the typical features of liver cells with alcoholic hepatitis, can be seen on a biopsy sample. This is usually done by a liver specialist and involves freezing an area of the skin with a local anaesthetic above the liver and pushing a small needle into the liver to obtain a sample.
What's the treatment for alcoholic liver disease?
Back to contentsIf you have alcoholic liver disease then you must stop drinking completely. Fatty liver and mild alcoholic hepatitis usually recover if you can manage this. Also, mild cirrhosis will often not progress if alcohol is avoided for life. In severe cases, however, where liver scarring is extensive, a liver transplant may be the only possible treatment option. Liver transplants are difficult to get, because there are not enough donor organs for everyone who needs them. Continuing to drink alcohol after a transplant can lead to the transplanted liver failing. Many centres therefore require people to have stopped using alcohol and drugs before they can be added to the transplant waiting list.
If you feel that you are drinking more alcohol than you should, or that you cannot stop drinking then treatment and support are available. Learn about treatment options for conditions caused by drinking too much alcohol. Remember that prevention is the best option.
What should I do if I have alcohol-related liver disease?
Back to contentsFor all types of liver disease caused by alcohol, you should stop drinking alcohol completely. Also, you may be referred to a dietician to review your diet. This is because many people who drink heavily do not eat properly and need advice on getting back into eating a healthy diet. Vitamin supplements may be prescribed for a while.
If you have fatty liver, or alcoholic hepatitis which is not severe, you should fully recover from these conditions if you stop drinking alcohol.
If you have severe hepatitis and require hospital admission, you may require intensive care treatment. Some people with severe hepatitis will die.
If you have 'scarring' of the liver (cirrhosis), stopping drinking alcohol can improve your outlook. It depends on how severe the cirrhosis has become. If cirrhosis is diagnosed when it is not too advanced and you stop drinking alcohol, the cirrhosis is unlikely to progress. However, the cirrhosis and symptoms will almost certainly get worse if you continue to drink alcohol. In severe cases where the scarring is extensive and the liver can barely function, a liver transplant may be the only option.
You are very unlikely to develop liver problems caused by alcohol if you drink within the recommended maximum limits.
If you're a heavy drinker and dependent on alcohol, it can be dangerous to stop drinking suddenly.
Signs of being physically dependent on alcohol include withdrawal symptoms if going too long without an alcoholic drink, such as feeling shaky, sweaty, anxious, and restless.
In severe cases, withdrawal can lead to hallucinations, confusion, and seizures, and can be life-threatening.
Seek medical advice if you think you might be physically dependent on alcohol; support can help you reduce and stop alcohol safely.
Do you need help to stop drinking?
Back to contentsHelp and treatment are available if you find that you cannot stop drinking alcohol. Counselling and support from a doctor, nurse, or counsellor are often all that is needed. A detox (detoxification) treatment may be advised if you are alcohol-dependent. Referral for specialist help may be best for some people. If you feel that you need, or a relative or friend needs, help about alcohol then speak with your doctor. Read more about alcohol withdrawal and detox.
Patient picks for Alcohol advice
Healthy living
Alcohol and sensible drinking - safe limits of alcohol
In the UK, almost half of adults drink alcohol once a week or more. About a quarter of all adults report drinking more than the recommended weekly limit of alcohol.
by Dr Doug McKechnie, MRCGP

Healthy living
Alcohol withdrawal and alcohol detoxification
Many people who regularly drink excessive quantities of alcohol become alcohol-dependent. This can cause the body serious harm. There is a great deal of help for people who are alcohol-dependent and want to stop drinking.
by Dr Hayley Willacy, FRCGP
Further reading and references
- Alcohol-use disorders: diagnosis, assessment and management of harmful drinking and alcohol dependence; NICE Clinical Guideline (February 2011 -last updated October 2014)
- Schutze M, Boeing H, Pischon T, et al; Alcohol attributable burden of incidence of cancer in eight European countries based on results from prospective cohort study. BMJ. 2011 Apr 7;342:d1584. doi: 10.1136/bmj.d1584.
- I J Beckingham and S D Ryder; ABC of diseases of liver, pancreas, and biliary system: Investigation of liver and biliary disease. BMJ 2001;322:33-36.
- Antenatal care; NICE guidance (August 2021)
- Guidelines on alcohol consumption; House of Commons Library, UK Parliament, June 2016
- Try Dry: the app to track your progress during Dry Jan and beyond; Alcohol Change UK
- No level of alcohol consumption is safe for our health; World Health Organization, 2023
Continue reading below
Article history
The information on this page is written and peer reviewed by qualified clinicians.
Next review due: 6 Jan 2028
18 Feb 2023 | Latest version

Ask, share, connect.
Browse discussions, ask questions, and share experiences across hundreds of health topics.

Feeling unwell?
Assess your symptoms online for free
Sign up to the Patient newsletter
Your weekly dose of clear, trustworthy health advice - written to help you feel informed, confident and in control.
By subscribing you accept our Privacy Policy. You can unsubscribe at any time. We never sell your data.