Liver function tests
Peer reviewed by Dr Toni Hazell, MRCGPLast updated by Dr Rosalyn Adleman, MRCGPLast updated 3 Aug 2024
Meets Patient’s editorial guidelines
- DownloadDownload
- Share
- Language
- Discussion
- Audio Version
In this series:Gilbert's syndromeJaundiceCirrhosisLiver failurePrimary biliary cholangitisWilson's disease
Liver function tests are a set of blood tests commonly done to check on the health of your liver. Changes in liver function tests give a clue as to whether your liver is under strain, inflamed, infected or diseased, and how badly. The pattern of the liver function tests can give a clue to the cause and can allow early detection of unsuspected problems, and monitoring of known problems.
In this article:
Video picks for Blood tests
Continue reading below
What is a liver function test?
Liver function tests are a type of blood test. A small amount of blood is taken from a vein in your arm. Liver function tests measure a series of chemicals which relate to the way the liver works. They include substances that are made in the liver or affected by the health of the liver cells, chemicals which are processed or excreted by the liver, and hormones that the liver makes in order to do its work.
What are liver function tests used for?
Back to contentsLiver function tests are aimed at giving a picture of the 'state' of your liver. They are a sensitive way of looking for liver strain or liver damage, as they often show this well before you get any symptoms or problems with your liver. This means that the cause of liver strain or damage can be diagnosed and, often, reversed.
Liver function tests are also used for monitoring in cases of known liver inflammation, injury or disease.
Continue reading below
What are the main liver function tests?
Back to contentsThe usual liver function tests typically include the following:
Bilirubin.
Albumin.
Total protein.
Transferases (AST or SGOT and ALT or SGPT).
Gamma GT.
Creatine kinase.
Prothrombin time or International Normalised Ratio (INR).
Each of these is discussed below. The liver performs hundreds of different functions, so there are many other possible tests that look at its health. These would normally be done if an abnormality is found with the basic liver function tests described here, or if a specific problem is suspected. They might include:
Virus tests - for example, for hepatitis A, B or C - to look for the cause of disease.
Autoantibody tests (to detect and monitor immune diseases).
Immunoglobulins (antibodies made in response to various challenges including allergies, infections, some blood disorders and some cancers).
Serum ferritin and transferrin saturation (measures of iron storage and management by your body).
Alpha-fetoprotein (maternal levels help look at the health of the baby during pregnancy, and levels are also raised in some cancers).
Copper/caeruloplasmin (measures of copper management by the body).
Alpha-1 antitrypsin (a hormone involved in protecting liver and lung cells from injury).
Clotting factors (particularly if there is a suspicion that your blood is not clotting well or you have severe liver disease).
Enhanced liver fibrosis score (ELF) -this is a set of three tests that can indicate if there is fibrosis (inflammation and scarring) of the liver.
Where and what is the liver, and what does it do?
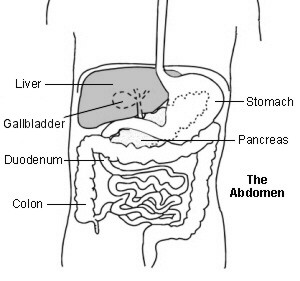
Back to contentsThe liver is your largest internal organ. It sits in the tummy (abdomen), under your diaphragm on the right-hand side. It is usually tucked under the ribs, which protect it, although in some people the edge of the liver protrudes slightly. If the liver is swollen, through inflammation or disease, it can swell out from under the ribs and make your tummy swollen.
Liver function
The liver is a factory for the production and breakdown of carbohydrates, fats, proteins, hormones and other essential body chemicals, and helps dispose of waste products. This work is mainly carried out by liver cells (hepatocytes). Some of the most important functions include:
Production of these substances
Glycogen (a carbohydrate energy store), which it makes from glucose.
Glucose, made and released into the blood from glycogen, proteins and fats.
Many essential proteins and amino acids (building blocks of proteins).
Many of the clotting factors that help your blood to clot normally.
Plays a part in red blood cell production.
Albumin, one of the main proteins in your blood, which bulks out your serum and enables it to carry essential substances around the body.
Angiotensinogen, which plays a role in blood pressure control.
Thrombopoietin, which regulates some of the work of your bone marrow.
Cholesterol, triglycerides, lipoproteins and fats - as part of the management of fat stores in your body.
Bile, excreted into the intestine for absorbing fats and vitamin K.
Hormones that help children grow and that build muscle in adults.
Breakdown of these substances
Excess hormones, including insulin.
Bilirubin, which is a waste product from worn-out blood cells.
Many waste products.
A wide range of toxic substances and medicines, including alcohol.
Foreign proteins that reach it from the digestive system (trapped and destroyed by specialised immune cells in the liver).
Storage of these (and other) substances
Glucose (as glycogen).
Vitamin A (1-2 years' supply).
Vitamin D (1-4 months' supply).
Vitamin B12 (3-5 years' supply).
Vitamin K.
Iron and copper.
Continue reading below
What can cause liver function tests to be abnormal?
Back to contentsYour liver function tests can be abnormal because:
There is a build-up of fat in the liver, due to being overweight or obese (called non-alcoholic fatty liver disease, or NAFLD). However this does not always cause abnormal liver function tests, and can also be picked up on an ultrasound scan of the liver. If NAFLD is diagnosed, further blood tests including NAFLD score, and ELF (enhanced liver fibrosis) test, and a fibroscan (a special type of ultrasound to look for more advanced signs such as fibrosis/cirrhosis) may be done to assess the severity of the condition.
Your liver is inflamed (for example, by infection, toxic substances like alcohol and some medicines, or by an immune condition).
Your liver cells have been damaged (for example, by toxic substances, such as alcohol, paracetamol, poisons).
Your liver is having to work harder to process medicines or toxic substances (for example, alcohol, paracetamol, poisons).
The bile drainage from your liver is blocked - for example, by a gallstone.
There is a swelling inside your liver (for example, an abscess or a tumour).
You have an underlying condition that affects the liver's production and storage abilities (for example, Wilson's disease, haemochromatosis, Gilbert's syndrome). In these cases the abnormality of your liver tests will be a feature of your condition, and may be normal for you.
Your liver is physically injured (for example, trauma).
You fall just outside the normal limits (see below).
What does the 'normal range' mean in liver function tests?
Back to contentsThe 'normal range' is a range of values given by the local laboratory for liver function tests. The range varies slightly between laboratories according to the measurement methods that they use.
The 'normal' limits are defined by laboratories as the range of levels inside which 19 of every 20 people with healthy livers will fall. This means that, for any one liver function test, around 1 in 20 people with healthy livers will have a result that is slightly abnormal. There will, in the majority of cases, be nothing wrong with their liver; having a liver function test that's just over the edge usually means nothing, as long as - crucially - there is only one slight abnormality out of the whole range of tests. You should always discuss even a slightly abnormal result with your doctor.
It is important to remember that having normal liver function test results doesn't mean you aren't at risk of liver problems. For instance, if you are involved in harmful behaviour, such as drinking excess alcohol, you could have normal liver function test results but still be putting your liver under strain.
What should I do if my liver function tests are abnormal?
You are likely to find out that your liver function tests are abnormal from your healthcare provider, who will tell you what you need to do next. However, if you obtain your liver function test results without explanation, you should contact your healthcare provider to discuss them.
Doctors consider a slightly abnormal liver function test as one that is less than twice the upper limit of the 'normal' value. Doctors consider a very abnormal liver function test as one that is more than two or three the upper limit of the 'normal' value.
Your doctor is also likely to be looking at the rate of change of your liver function tests - if a test has increased very rapidly, it may be of more concern even though it is not that high.
If the liver function tests are very mildly abnormal, only one or two tests are affected and you are perfectly well, this would not normally need an urgent consultation. However, you should speak to a health professional for advice within a few days (in case more tests or monitoring need to be done).
If you have multiple abnormalities on your liver function tests, if some of the tests are very abnormal or if you are also unwell or in pain then you should seek medical advice more urgently.
If you have known liver disease and your liver function tests have altered significantly since the last time they were checked, you should seek medical advice the same day unless you have a standing instruction to do something different.
Sometimes an abnormal liver function test is normal for you. If you already know this is the case then it may be that no action is needed. A common example of this is Gilbert's syndrome, when you have a naturally raised level of bilirubin but other liver function tests are normal and you are well. Your doctor will tell you if you have Gilbert's syndrome.
What will my doctor do if I have abnormal liver function tests?
Back to contentsAll abnormal liver function tests need explanation, even if that explanation is that you are one of the 5% who fall outside the 'normal' range.
In many cases, a single, isolated, slightly abnormal liver function test in a well patient will not signify an underlying problem. However, some liver disorders, including early signs of overuse of alcohol, can produce slight changes (especially at first), so it's important to be sure.
Your doctor will want to do further liver tests and to see, question and examine you, to determine the reason for the blood test abnormality. If you are otherwise well, this will initially be done in primary care. Options include:
Repeating the blood test.
Further blood tests in order to discover or rule out particular causes.
An ultrasound scan of your liver and gallbladder.
Depending on the severity and suspected cause, referral to a liver specialist for advice, more specialist tests and liver biopsy.
If you are very unwell, you may need referral or admission to hospital.
Can my doctor make a diagnosis from my liver function test?
Sometimes. Single abnormalities in the liver function tests do not give diagnoses on their own but the pattern of abnormalities can point to the most likely cause of the problem. When this is combined with speaking to and examining you, your doctor may be able to make a clear diagnosis.
Once the cause of the abnormality has been determined, your doctor will discuss what you need to do next.
What do unusually low levels on my liver function tests mean?
Note that in most cases (except albumin and calcium) it is a raised (rather than a lowered) level in the liver function test which may indicate a problem. In the following descriptions, where low levels can be significant for your health they are also described.
What does an abnormal bilirubin level mean?
Back to contentsBilirubin comes from the breakdown of red blood cells in the body. The liver processes (conjugates) bilirubin so that it can be excreted via the kidneys. A high bilirubin level can make you appear jaundiced (with a yellow tinge to the skin and to the whites of the eyes).
The most likely cause of raised bilirubin depends on whether the rise is in bilirubin that the liver has already processed (conjugated bilirubin), in the bilirubin that the liver has not yet processed (unconjugated bilirubin), or in both.
A rise in both types of bilirubin
Conjugated bilirubin tends to rise if the flow of bile in the tiny tubes within the liver is blocked, and unconjugated bilirubin tends to rise if the liver cells cannot do their work (or there is too much work for them to do). If the liver is both damaged (not working properly) and swollen or scarred (blocking the drainage system) then both types of bilirubin will tend to rise.
An isolated rise in unconjugated bilirubin
Unconjugated bilirubin may increase because the liver can't process the bilirubin, or because the body is making an excess of bilirubin by breaking down too many blood cells, and the liver is normal but can't keep up.
In adults, the most common causes are breakdown of blood cells (haemolysis) and Gilbert's syndrome.
Haemolysis is a condition of the blood. Further tests will be needed to identify the cause and you may need to see a haematologist. Causes can include reactions to medicines, lifelong (congenital) blood cell abnormalities such as hereditary spherocytosis and, in babies, breast milk jaundice, severe infection (sepsis) and haemolytic disease of the newborn.
An isolated rise in conjugated bilirubin
Increased conjugated bilirubin suggests that the liver is conjugating the bilirubin properly (the job of liver cells) but not excreting it properly via the bile ducts. Causes include:
Reactions to some medicines, including common ones such as blood pressure tablets, hormones (for example, oestrogen), antibiotics (particularly erythromycin and flucloxacillin), tricyclic antidepressants and anabolic steroids.
Some autoimmune diseases that affect bile excretion.
Blockage of the bile ducts - for example, by a gallstone.
Dubin-Johnson syndrome and Rotor's syndrome.
In babies a rise in conjugated bilirubin can signify rare but serious problems with the development of the bile drainage system in the liver, such as biliary atresia.
What does an abnormal albumin level mean?
Albumin is the main protein in your serum, and its level is a good guide to long-term liver health. Albumin levels that are abnormally low have the greatest significance for the liver.
Low levels of albumin
This can be due to:
Severe liver disease.
Poor nutrition.
Malabsorption of protein (for example, in Crohn's disease or in coeliac disease).
Bowel conditions which result in leakage of protein (for example, severe bowel inflammation or infection such as cholera).
Protein loss through kidney problems (for example, nephrotic syndrome).
Failure of protein manufacture through severe liver inflammation.
Albumin levels also fall if you lose protein through your skin (for example, in extensive skin inflammation and widespread burns).
Albumin levels decrease during pregnancy, when your blood is more dilute.
High levels of albumin
This is usually due to having the tourniquet on for too long before your blood sample is taken. Sometimes it can be due to a very high-protein diet, as in bodybuilders, or to lack of fluid in the body (dehydration), when the blood is more concentrated.
What does an abnormal total protein level mean?
Back to contentsTotal protein measures the total of albumin and globulins. It is usually normal in liver disease even if albumin levels are low, as globulin levels tend to increase as albumin levels fall.
High values of total protein are seen in chronic active hepatitis and alcoholic hepatitis.
High values of total protein are also seen in conditions outside the liver which increase globulins (such as myeloma) and conditions involving overactivity of the immune system (such as severe infection and chronic inflammatory disease).
Low levels of total protein can sometimes be seen in severe liver disease, in conditions of severe protein loss (such as widespread burns) and in severe malnutrition.
What does an abnormal ALT (SGPT), AST (SGOT) or creatine kinase level mean?
Back to contentsThese substances are also called transferases. They are liver enzymes (proteins which help do the work of the liver) which are normally found inside liver cells rather than in the blood.
ALT stands for alanine transaminase and is also called SGPT (serum glutamic-pyruvic transaminase).
AST stands for aspartate transaminase and is also called SGOT (serum glutamic oxaloacetic transaminase).
Creatine kinase is sometimes checked along with AST and ALT.
If blood levels of transaminases go up this suggests leakage from damaged liver cells due to inflammation or cell death. AST and ALT tend to be high in liver disease and very high in liver inflammation.
ALT is mainly found in the liver. AST is also found in muscle and red blood cells.
ALT rises more than AST in acute liver damage eg, viral hepatitis.
In chronic liver disease (for example, alcoholic cirrhosis), AST is higher than ALT.
Lower-than-normal levels of transaminases do not signify disease.
Creatine kinase comes mainly from muscle, so if it is raised alongside AST and ALT it suggests that the liver may not be the main source of the problem.
Causes of mild rises in transferases
These include:
Non-alcoholic fatty liver disease (the most common cause).
Chronic hepatitis C infection.
Haemochromatosis (a genetic condition that tends to come on in your 40s or 50s).
Causes of marked increases in transferases
Marked increases are usually caused by acute injury to the liver by viruses, shortage of oxygen (ischaemia) or toxic substances. Causes include:
Viral (hepatitis A, hepatitis B, hepatitis C, hepatitis D or hepatitis E). Hepatitis A and B tend to have the greatest increases.
Very high levels (>75 times upper reference limit) suggest ischaemic or toxic (poison or medicine-related) injury to the liver.
Ischaemic liver damage is mostly seen in patients with other serious illnesses such as septicaemia or collapse.
What does an abnormal gamma-glutamyl transferase level mean?
Back to contentsGamma-glutamyl transferase (GGT) levels increase in most liver diseases. This liver function test is very sensitive, although it also goes up in some heart, lung and kidney conditions.
The most common reason for GGT increasing as a single abnormality is drinking more alcohol than your liver can easily cope with. GGT levels can be 10 times normal. The rise is a sign your liver is under strain and is at risk of being damaged by alcohol.
GGT rises to 2-3 times the upper limit of normal in non-alcoholic fatty liver disease (NAFLD). This condition is increasingly common and can progress to scarring or inflammation of the liver. Transaminase levels also tend to rise in NAFLD.
Some prescribed and over-the-counter medicines can increase GGT levels.
GGT rises in some patients with chronic hepatitis C infection.
In chronic liver disease, a rise in GGT suggests bile duct damage and scarring.
What does an abnormal alkaline phosphatase level mean?
Back to contentsAlkaline phosphatase (ALP) comes mainly from the cells lining bile ducts and from bones - particularly growing bones. Therefore it is commonly raised during childhood and puberty. It rises if there is slow or blocked flow in the bile ducts, if the bile ducts are damaged and in bone disorders.
If the cause is in the liver, the GGT is also abnormal, whereas if it's the bone, the GGT is usually normal. ALP is also raised during the third trimester of pregnancy.
Common causes of raised ALP with other abnormalities on your liver function tests include:
Hepatitis of any cause.
Bile duct blockage of any cause.
Isolated raised ALP can occur in:
Bone fractures.
Cancer in bones or in the liver.
What do abnormal prothrombin time and INR mean?
Back to contentsProthrombin time (PT) or International Normalised Ratio (INR) are sometimes measured as a part of standard liver function tests.
PT and INR are ways of measuring the ability of your blood to clot. Conditions which impair this clotting (prolonging the PT and increasing the INR) include:
Acute and severe liver disease (including liver failure and severe paracetamol overdose).
Use of anticoagulant medicines (in this case, lengthening the prothrombin time and increasing the INR is the intention).
How do I keep my liver function healthy?
Back to contentsThere is a difference between what you need to do to keep your liver healthy most of the time and what you need to do if your liver is damaged or inflamed .
The liver does not need a detox diet, which will not help it and will often (if it is very low-calorie, for instance) make it work harder. The liver is a digesting, storage and detoxing organ. If you are well, the way to look after your liver is by:
A balanced diet with a good fibre content.
Regular exercise.
Keeping your weight within healthy limits.
Avoiding 'fad' diets (which can challenge the kidneys and liver hard).
Avoiding unnecessary medicines and supplements including paracetamol
Stopping smoking.
Saying within the recommended limits for alcohol (both daily and weekly).
If your liver is inflamed and injured (for example, you have hepatitis and are jaundiced) or you have advanced liver disease (for example, cirrhosis) then, depending on the severity, you may be advised to have a special diet. This involves using carbohydrates as your major source of calories, eating fat moderately and cutting down on protein. You may be advised to take vitamin supplements, and if you are retaining fluid you should reduce your salt consumption to less than 1500 milligrams per day.
A few things to remember about abnormal liver function tests
Liver function tests are not a diagnosis; they are a set of clues which help doctors make a diagnosis.
Liver function tests are a sensitive early warning system for problems in the liver and, in some cases, elsewhere.
Because 'normal ranges' used by laboratories are the levels between which about 19 out of 20 of people's tests will fall, about 1 person in 20 will have an abnormal test without cause. About half of these people will have slightly high tests and about half will have slightly low tests, but their levels either way should not be extreme.
The most likely cause of any particular pattern of abnormal liver function tests varies between patients (because of difference in age and sex) and between populations (because of variations in genetics and because different things are more common in different parts of the world).
Almost any pattern of liver function test abnormality can be caused by medicines (including over-the-counter medications), by herbal remedies and traditional medicines from other cultures, and by poisonous substances.
Many liver conditions cause no symptoms, at least at first; so, if you have several abnormal tests (or one test is markedly abnormal), it is very important to follow this up.
Although single, mildly abnormal tests are not usually significant, any unexplained abnormality generally needs a check that you are well and may need a repeat test.
Abnormal liver function tests in a person who is also sick are more worrying than those in a person who is well.
Dr Mary Lowth is an author or the original author of this leaflet.
Patient picks for Blood tests

Tests and investigations
Hyponatraemia
Hyponatraemia is a low level of sodium in the blood. Sodium levels in the blood have to be tightly controlled. Various chemical messengers (hormones) and organs are involved in this process. For example, hormones involved include antidiuretic hormone and cortisol, and organs involved include the brain and kidneys. There is a very close relationship between body sodium and body fluid levels.
by Dr Hayley Willacy, FRCGP

Tests and investigations
Synacthen test
A synacthen test checks the function of the adrenal glands. It can help to see whether the adrenal glands are producing enough steroid hormone (cortisol). Note: the information below is a general guide only. The arrangements, and the way tests are performed, often vary between different hospitals. Always follow the instructions given by your doctor or local hospital.
by Dr Philippa Vincent, MRCGP
Further reading and references
- Cirrhosis in over 16s - assessment and management; NICE Guideline (July 2016 - last updated September 2023)
- Liver disease; NICE Quality standard, June 2017
- Non-alcoholic fatty liver disease (NAFLD); NICE CKS, October 2023 (UK access only)
- Non-alcoholic fatty liver disease (NAFLD): Risk factors; NICE CKS, October 2023 (UK access only)
- Autoimmune Hepatitis Association
- Hepatitis C; NICE CKS, September 2022 (UK access only)
- Hepatitis A; NICE CKS, May 2021 (UK access only)
- Hepatitis B; NICE CKS, April 2024 (UK access only)
Continue reading below
Article history
The information on this page is written and peer reviewed by qualified clinicians.
Next review due: 3 Aug 2027
3 Aug 2024 | Latest version

Ask, share, connect.
Browse discussions, ask questions, and share experiences across hundreds of health topics.

Feeling unwell?
Assess your symptoms online for free
Sign up to the Patient newsletter
Your weekly dose of clear, trustworthy health advice - written to help you feel informed, confident and in control.
By subscribing you accept our Privacy Policy. You can unsubscribe at any time. We never sell your data.