Cirrhosis
Peer reviewed by Dr Toni Hazell, MRCGPLast updated by Dr Philippa Vincent, MRCGPLast updated 24 May 2023
Meets Patient’s editorial guidelines
- DownloadDownload
- Share
- Language
- Discussion
- Audio Version
In this series:Liver function testsGilbert's syndromeJaundiceLiver failurePrimary biliary cholangitisWilson's disease
Cirrhosis is a serious condition where normal liver tissue is replaced by scar tissue (fibrosis). It tends to progress slowly and often does not cause symptoms in its early stages. However, as the function of the liver gradually becomes worse, serious problems can develop.
In the UK, the two commonest causes of cirrhosis are alcohol drinking above recommended limits and hepatitis C infection. Treatments may vary, depending on the cause. If cirrhosis becomes severe, a liver transplant may be the only option.
In this article:
Video picks for Liver and gallbladder
Continue reading below
What is cirrhosis of the liver?
Cirrhosis is a condition where normal liver tissue is replaced by scar tissue (fibrosis).
The 'scarring' tends to be a gradual process. The scar tissue affects the normal structure and regrowth of liver cells. Liver cells become damaged and die as scar tissue gradually develops. Therefore, the liver gradually loses its ability to function well.
The scar tissue can also affect the blood flow through the liver, which can cause back pressure in the blood vessels which bring blood to the liver. This back pressure is called portal hypertension.
What does the liver do?
Back to contentsLiver function
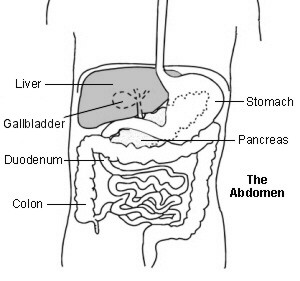
The liver is in the upper right part of the tummy (abdomen). It has many functions which include:
Storing fuel for the body (glycogen) which is made from sugars. When required, glycogen is broken down into glucose which is released into the bloodstream.
Helping to process fats and proteins from digested food.
Making proteins that are essential for blood to clot (clotting factors).
Processing many medicines that you may take.
Helping to remove or process alcohol, poisons and toxins from the body.
Making bile which passes from the liver to the gut and helps to digest fats.
Continue reading below
Cirrhosis symptoms
Back to contentsIn the early stages of the condition, there are often no symptoms of cirrhosis. Livers can continue to function with a reduced number of working liver cells. However, as more and more liver cells die and more and more scar tissue (fibrosis) builds up, the liver:
Fails to make enough proteins such as albumin that help to regulate the fluid composition in the bloodstream and body.
Fails to make enough chemicals needed for blood clotting.
Is less able to process waste chemicals in the body, such as bilirubin, leading these to build up in the body.
Is less able to process medicines, toxins and other chemicals which may then build up in the body.
Therefore, the symptoms that may develop include:
Tiredness and weakness.
Fluid which leaks from the bloodstream and builds up in the legs (oedema) and tummy (abdomen) - this is called ascites.
Loss of appetite, feeling sick (nausea) and being sick (vomiting).
Losing weight (although it is possible to gain weight if a lot of fluid is being retained).
A tendency to bleed and bruise more easily.
Yellowing of the skin or of the whites of the eyes (jaundice) due to a build-up of bilirubin.
Itchiness due to a build-up of toxins.
Mental health changes - these can develop in severe cases as toxins build up in the bloodstream and affect the brain. This can cause changes to personality and behaviour, confusion, forgetfulness and difficulty concentrating. Eventually it can lead to loss of consciousness and hepatic coma. These changes are known as hepatic encephalopathy.
The scar tissue restricts the flow of blood through the liver and, as the cirrhosis becomes worse, this causes back pressure in the portal vein (known as portal hypertension). The portal vein is the vein that takes blood from the gut to the liver - this is rich in nutrients and also carries any toxins that the liver should be removing from the body.
Increased pressure in this vein can cause swellings (varices) to develop in the branches of the vein in the lining of the gullet (oesophagus) and stomach. These varices have a tendency to bleed easily into the gut. If a bleed occurs, this may cause vomiting of blood or passing altered blood with your stools (faeces) - this tends to make the stools black, tarry and offensive (melaena).
What causes cirrhosis?
Back to contentsThere are many causes of 'scarring' of the liver (cirrhosis). In the UK the most common causes are alcohol and infection with the hepatitis C virus.
Alcoholic cirrhosis
Liver cells break down alcohol but too much alcohol can damage the liver cells. As a rule, the heavier the drinking, the more the risk of developing cirrhosis. However, alcoholic cirrhosis is not just a condition of people who have alcohol dependency. People who are drink socially but above recommended limits also develop cirrhosis.
About 1 in 10 people drinking above the recommended alcohol limits will eventually develop cirrhosis. It tends to occur after 10 or more years of excessive drinking. It is not clear why some people are more prone to their liver cells becoming damaged by alcohol and to developing cirrhosis. There may be an inherited (genetic) tendency. Women seem to be more prone than men to cirrhosis although it is still a disease more common in men.
Hepatitis C and cirrhosis
Persistent (chronic) infection with the hepatitis C virus causes long-term inflammation in the liver. This can eventually lead to liver 'scarring' and cirrhosis. Up to 1 in 5 people with chronic hepatitis C develop cirrhosis but this usually takes about 20 years or even longer from the initial infection.
Other causes of cirrhosis
Causes which are less common in the UK include:
Chronic infection with the hepatitis B virus. Worldwide, this is the most common cause of cirrhosis.
Autoimmune hepatitis. The immune system normally makes antibodies to attack bacteria, viruses and other germs. In people with autoimmune diseases, the immune system makes antibodies against part(s) of the body. Something triggers the immune system to make these autoantibodies but the trigger is not known. In autoimmune hepatitis, the immune system makes antibodies against liver cells, which can lead to damage and cirrhosis.
Diseases that cause blockage of the bile ducts can cause back pressure and damage to the liver cells., for example, primary biliary cirrhosis, sclerosing cholangitis, and congenital problems of the bile ducts.
Non-alcoholic steatohepatitis (NASH), now called non-alcoholic fatty liver disease (NAFLD) This is a condition which causes fat to build up in the liver. This can lead to scarring and cirrhosis. Being overweight/obese increases the risk of developing NASH.
Severe reactions to certain medicines.
Certain poisons and environmental toxins.
Certain infections caused by bacteria and parasites which are usually found only in tropical countries. Parasites are living things (organisms) that live within, or on, another organism.
Severe heart failure which can cause back pressure of blood and congestion in the liver.
Some rare inherited diseases which can cause damage to liver cells. For example:
Haemochromatosis. This is a condition which causes an abnormal build-up of iron in the liver and other parts of the body.
Wilson's disease. This is a condition which causes an abnormal build-up of copper in the liver and other parts of the body.
Other rare disorders.
Continue reading below
How common is cirrhosis?
Back to contentsThere are an estimated 30,000 people living with cirrhosis in the UK and at least 7,000 new cases being diagnosed each year. The numbers of people living with both alcoholic cirrhosis and non-alcohol-related cirrhosis seem to be rising.
How is cirrhosis diagnosed?
Back to contentsA doctor may suspect, from symptoms and a physical examination, that there is 'scarring' of the liver (cirrhosis). A doctor may especially think of cirrhosis as a cause of these symptoms if you have a history of heavy alcohol drinking or have had a previous episode of hepatitis.
Blood tests may show abnormal liver function. See the separate leaflet called Liver Function Tests for more details. An ELF blood test can give a good estimation of the degree of fibrosis in the liver and whether further tests for cirrhosis are needed. An ultrasound scan (or a computerised tomography (CT) scan or a magnetic resonance imaging (MRI) scan) may show a damaged liver. To confirm the diagnosis, a small sample (biopsy) of the liver may be taken to be looked at under the microscope. See the separate leaflet called Liver Biopsy for more details. The scarring of the liver and the damage to liver cells can be seen on a biopsy.
If the underlying cause of the cirrhosis is not clear, further tests may be done to clarify the cause. This might involve checking for antibodies to hepatitis viruses, checking for autoantibodies that may have attacked liver cells, looking in a blood sample for excess iron or copper, etc.
Cirrhosis treatment
Back to contents'Scarring' of the liver (cirrhosis) tends to become progressively worse if the underlying cause persists and is not treated. In general, once the damage is done the scarring is not reversible. Therefore, the aim of treatment is, if possible, to prevent further liver scarring or to slow the progression of the scarring process. Treatments that may be advised include the following.
Stop drinking alcohol
Whatever the cause of cirrhosis, alcohol should be stopped completely. Drinking alcohol will increase the rate of progression of cirrhosis from whatever cause.
Be cautious when taking medicines
It is important that a doctor or pharmacist is aware of the diagnosis of cirrhosis before taking any prescribed or over-the-counter medicines. Some medicines that are processed in the liver may need their dose adjusted and some should not be used at all.
Treatment for underlying causes
Some of the underlying causes of cirrhosis can be treated. This may slow down, or halt, the progression of cirrhosis. For example:
Not drinking alcohol if alcohol is the cause.
Interferon and other medication may be used to treat viral hepatitis.
Steroid medicines or other immunosuppressant medicines may be used to treat autoimmune diseases causing liver damage.
Regular removal of a pint or so of blood can remove excess iron which occurs in haemochromatosis.
Treatment to ease symptoms and prevent complications
Various treatments may be advised, depending on the severity of the cirrhosis and the symptoms that develop. For example:
Adequate food intake (including calories and protein) and regular exercise are important to prevent excessive weight loss and muscle wasting.
A low-sodium diet or 'water' tablets (diuretics) to reduce fluid accumulating in the body.
Medicines to reduce itchiness.
Zinc deficiency is common in cirrhosis and zinc supplements may be used.
Vaccination to protect against hepatitis A, influenza and pneumococcal infections.
'Thinning' of the bones (osteoporosis) may occur and so prevention and treatment of osteoporosis are important.
Medicines that may help to reduce portal hypertension.
Drainage of fluid that builds up in the tummy (abdomen) - called ascites.
Treatment of bleeding varices
A bleed from swellings (varices) - described above - is a medical emergency. Seek medical help immediately if you have cirrhosis and:
You bring up (vomit) blood; or
You pass blood in your stools (faeces); or
Your stools become black.
Various surgical techniques can be used to stop the bleeding and to help reduce the risk of further bleeds.
Liver transplant
In severe cases, where the scarring is extensive and the liver can barely function, then a liver transplant may be the only option.
The future
Up until recently, the scarring process of cirrhosis was thought to be irreversible. However, recent research has led to a greater understanding of the scarring process. Some research suggests that medicines may be able to be developed that can reverse the scarring process.
Stem cell or liver cell transplantation aimed at restoring liver function is also being investigated. This research continues.
Can cirrhosis be prevented?
Back to contentsAlcohol
The most common cause of 'scarring' of the liver (cirrhosis) in the UK is alcohol drinking above recommended limits. The most important way to prevent cirrhosis from developing is to drink within the recommended safe limits. That is:
Men should drink no more than 14 units of alcohol per week, no more than four units in any one day and have at least two alcohol-free days a week.
Women should drink no more than 14 units of alcohol per week, no more than three units in any one day and have at least two alcohol-free days a week.
Pregnant women. Advice from the Department of Health states that: "Pregnant women or women trying to conceive should not drink alcohol at all. If they do choose to drink, to minimise the risk to the baby, they should not drink more than 1-2 units of alcohol once or twice a week and should not get drunk."
Where do these recommendations come from?
The Department of Health guidelines on alcohol limits were updated in January 2016. These recommendations come from their guidelines.
Some would argue that the upper limits of the recommendations are too high. For example, one study found that drinking more than two units a day for men and more than one unit a day for women significantly increases the risk of developing certain cancers.
In general, the more alcohol is drunk above these limits, the more harmful alcohol is likely to be.
A unit of alcohol is about equal to:
A half pint of normal-strength beer, cider or lager.
A pub measure of spirits (25 ml) or of fortified wine such as sherry (50 ml).
A small glass (125 ml) of wine containing 8% alcohol by volume.
Note: using the above guide, it is easy to underestimate how much alcohol is in a drink. This is because many beers are now strong and wines are often served in 175 ml glasses. Many wines are also stronger than standard (some contain 12-14% alcohol by volume).
However, it is important not to drink alcohol at all if cirrhosis has already developed or with a diagnosis of chronic hepatitis or certain other liver problems.
Infectious diseases
Some causes of cirrhosis are due to infectious diseases which can often be prevented. For example, people who inject street drugs are at risk of hepatitis B and C if they use unclean needles or other injection equipment. These infections may also be passed on through unprotected sex. Hepatitis B can be prevented by immunisation which is offered to those at risk such as healthcare workers, drug users and people with multiple sexual partners.
What is the outlook?
Back to contentsThe outlook (prognosis) depends on factors such as the underlying cause, how early the condition is diagnosed, and how early treatment is given. Many people who have cirrhosis which is not too extensive live a normal life for a number of years.
In some cases, the progression of the cirrhosis can be halted or slowed by treatment. The outlook is not so good if there is a lot of liver damage, especially in alcoholic cirrhosis whilst continuing to drink alcohol.
Cirrhosis can cause death due to bleeding from swellings (varices) or by going into a coma from liver failure. People with cirrhosis are also at increased risk of developing serious infections.
People with cirrhosis have an increased risk of developing cancer of the liver (hepatocellular carcinoma). The risk varies according to the cause of cirrhosis. The greatest risk is with cirrhosis caused by hepatitis C infection, followed by cirrhosis caused by hereditary haemochromatosis.
The risk of developing liver cancer is lower in those with alcoholic cirrhosis. People with cirrhosis should have regular checks to make sure that there are no signs of liver cancer developing.
Patient picks for Liver and gallbladder

Digestive health
Non-alcoholic fatty liver disease
Non-alcoholic fatty liver disease (NAFLD) describes a range of conditions caused by a build-up of fat within liver cells.
by Dr Doug McKechnie, MRCGP

Digestive health
Primary sclerosing cholangitis
Primary sclerosing cholangitis is an uncommon condition affecting the bile ducts and liver. Inflammation and scarring of the bile ducts can lead to liver damage and cirrhosis - a condition where normal liver tissue is replaced by scar tissue (fibrosis). Different treatments are available to control symptoms that may develop and also to manage any complications which may occur. The outlook for people with primary sclerosing cholangitis can be very variable.
by Dr Colin Tidy, MRCGP
Further reading and references
- Tsochatzis EA, Bosch J, Burroughs AK; Liver cirrhosis. Lancet. 2014 May 17;383(9930):1749-61. doi: 10.1016/S0140-6736(14)60121-5. Epub 2014 Jan 28.
- Cirrhosis in over 16s - assessment and management; NICE Guideline (July 2016 - last updated September 2023)
- Liver disease; NICE Quality standard, June 2017
- Premkumar M, Anand AC; Overview of Complications in Cirrhosis. J Clin Exp Hepatol. 2022 Jul-Aug;12(4):1150-1174. doi: 10.1016/j.jceh.2022.04.021. Epub 2022 May 14.
- Cirrhosis; NICE CKS, June 2018 (UK access only)
Continue reading below
Article history
The information on this page is written and peer reviewed by qualified clinicians.
Next review due: 12 May 2028
24 May 2023 | Latest version

Ask, share, connect.
Browse discussions, ask questions, and share experiences across hundreds of health topics.

Feeling unwell?
Assess your symptoms online for free
Sign up to the Patient newsletter
Your weekly dose of clear, trustworthy health advice - written to help you feel informed, confident and in control.
By subscribing you accept our Privacy Policy. You can unsubscribe at any time. We never sell your data.