Microvascular angina
Cardiac Syndrome X
Peer reviewed by Dr Colin Tidy, MRCGPLast updated by Dr Hayley Willacy, FRCGP Last updated 20 Nov 2023
Meets Patient’s editorial guidelines
- DownloadDownload
- Share
- Language
- Discussion
- Audio Version
In this series:AnginaCoronary artery spasm
There is no agreed definition for CSX. The underlying cause may be sudden narrowing (spasm) of normal coronary arteries without any evidence of atheromatous fatty plaques.
In this article:
Video picks for Heart disease
Continue reading below
What is cardiac syndrome X?
Cardiac syndrome X (CSX) is thought to be a type of angina. In CSX chest pain is felt when the heart works harder but the heart arteries appear to be normal on coronary angiography.
The term CSX is often used to describe microvascular angina. The larger blood vessels in the heart (that show up in investigations) are normal. However, much smaller vessels (the microvasculature) are thought to be where there is narrowing. Therefore, a better name for CSX would perhaps be 'microvascular angina'.
How common is cardiac syndrome X?
Back to contentsBecause doctors have not been able to decide exactly what CSX is, there are no precise numbers of how many people have the condition. Each year about 20,000 people in the UK develop angina for the first time. Of these people, about 1 woman in 5 and 1 man in 10 will have CSX. Unlike the more common type of angina, CSX is more common in women than in men. Certain factors make CSX more likely to develop - for example:
Having mild arthritis.
Continue reading below
What are the symptoms of microvascular angina?
Back to contentsThe common symptom is a pain, ache, discomfort or tightness that is felt across the front of the chest during exertion - such as walking up a hill or against a strong, cold wind. Pain may also be felt in the arms, jaw, neck or stomach.
An angina pain does not usually last long. It will usually ease within 10 minutes after rest. Angina pain may also be triggered by other causes of a faster heart rate. For example, having a vivid dream or an argument. The pains also tend to develop more easily after meals.
CSX pain can be quite severe and disabling.
How is microvascular angina diagnosed?
Back to contentsThe doctor will want to know all about the pain and when it happens. Angina-type pains have a pattern. They will also use this information to rule out other causes of pain, such as pain from the gullet (oesophagus) or from your muscles and joints.
A doctor may also:
Ask about lifestyle (smoking and drinking habits).
Ask about typical diet and exercise patterns.
Take a blood pressure reading.
They may recommend a blood test to check cholesterol levels.
Continue reading below
Tests for microvascular angina
Back to contentsHeart tracing test
A 'heart tracing' (electrocardiogram, or ECG) is often done. However, this is usually normal when not exerting yourself. Having an ECG whilst exercising (sometimes called a stress test) may reveal a typical pattern (a downward-sloping ST segment) to the doctor. This helps to make the diagnosis.
Angiogram test
Typical angina can be confirmed by an angiogram test. A special dye is injected into the arteries or the heart (coronary arteries). X-ray equipment shows up the structure of the arteries and can also show the location and severity of any narrowing caused by atheroma.
The angiogram is usually normal in people with CSX. However, the angiogram may show narrowing when certain chemicals (for example, acetylcholine) are injected. The injection of these chemicals causing abnormalities in the angiogram helps to diagnose CSX.
Coronary flow reserve
Guidelines now suggest measuring the blood flow in the coronary arteries whilst provoking a spasm. This is called the coronary flow reserve. It is a useful guide to what treatments should be used and the level of risk the spasm creates for other events, such as a heart attack. The measurements can either be made invasively (through a guide wire inserted into a major vein) or non-invasively by an imaging technique; echocardiography, MRI or PET scan.
How to treat microvascular angina
Back to contentsCSX can be difficult to treat but a range of different treatments can help. The treatments include reducing risk factors as listed above. It is particularly important to have regular exercise.
Several different medicines may also be helpful, including calcium-channel blockers, beta-blockers, angiotensin-converting enzyme (ACE) inhibitors, ranolazine and statins. Nitrates such as GTN may be effective for symptom relief in addition to the longer-acting nitrates for overall control. An anti-platelet medicine (such as aspirin) may also be used to reduce the risk of clots forming which could lead to a heart attack.
Glyceryl trinitrate (GTN) spray or tablets
If angina is likely, it is usual to be prescribed a glyceryl trinitrate (GTN) spray or tablets. A dose is taken under the tongue when the angina pain develops. GTN is absorbed quickly into the bloodstream, from under the tongue, and should ease the pain within a few minutes.
It works by relaxing the blood vessels. This reduces the workload on the heart. It also helps to widen the coronary arteries and increase the flow of blood to the heart muscle.
A dose of GTN may cause a headache and/or flushing for a short while. If this medicine does not relieve the pain quickly, tell your doctor. Further tests may be needed.
Other treatments for microvascular angina
Other treatments that have been tried include a piece of equipment called a transcutaneous electrical nerve stimulation (TENS) machine or a spinal cord stimulator. They help manage the pain and increase exercise tolerance.
Sometimes other medicines may also be advised, if there is high blood pressure or a high cholesterol level. These are to lower your overall risk of cardiovascular problems.
What can I do to help myself?
Back to contentsCertain factors increase the risk of more fatty patches or plaques (atheroma) forming, which can make any type of angina worse. These are discussed in more detail in a separate leaflet called Preventing Cardiovascular Diseases.
Is microvascular angina serious?
Back to contentsCSX symptoms may improve over time. Unfortunately, in about 1 out of 5 people, their symptoms become worse. The pain can become difficult to relieve and this affects the quality of life for people with CSX.
Patient picks for Heart disease

Heart health and blood vessels
Acute coronary syndrome
The term 'acute coronary syndrome' (ACS) covers a range of disorders, including a heart attack (myocardial infarction) and unstable angina, that are caused by a sudden reduction of blood flow to part of the heart muscle. This is usually caused by a blood clot.
by Dr Rosalyn Adleman, MRCGP
Heart health and blood vessels
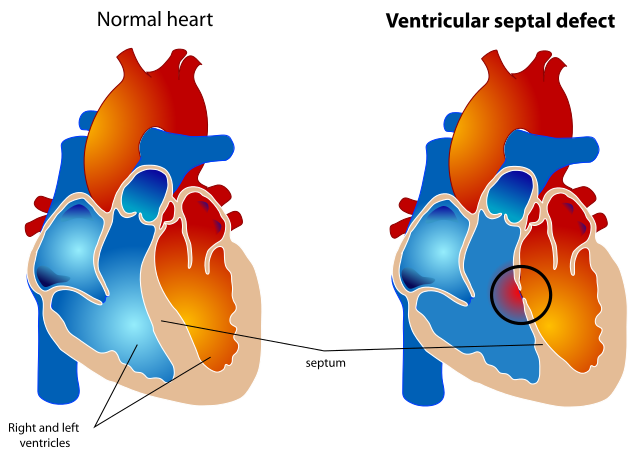
Ventricular septal defect
Ventricular septal defect (VSD) is a gap or defect in the septum between the heart's two lower chambers (ventricles). The septum is a wall that separates the heart's right and left side of the heart. Septal defects are sometimes called a 'hole' in the heart. It is the most common heart problem that babies are born with. Many defects in the ventricular septum close themselves and cause no problems. Otherwise, medicines or surgery can help. Most babies born with a defect in the septum have normal survival.
by Dr Hayley Willacy, FRCGP
Further reading and references
- Mahtani AU, Padda IS, Johal GS; Cardiac Syndrome X.
- Knuuti J, Wijns W, Saraste A, et al; 2019 ESC Guidelines for the diagnosis and management of chronic coronary syndromes. Eur Heart J. 2020 Jan 14;41(3):407-477. doi: 10.1093/eurheartj/ehz425.
- Jarczewski J, Jarczewska A, Boryczko A, et al; Microvascular angina (Cardiac Syndrome X) from a historical overview, epidemiology, pathophysiology to treatment recommendations - a minireview. Folia Med Cracov. 2021 Sep 29;61(3):95-114. doi: 10.24425/fmc.2021.138954.
- Elsayed EA; Non-invasive Evaluation of Coronary Flow Reserve in Cardiac Syndrome X Patients. Eur Cardiol. 2023 Apr 25;18:e24. doi: 10.15420/ecr.2023.18.PO7. eCollection 2023.
Continue reading below
Article history
The information on this page is written and peer reviewed by qualified clinicians.
Next review due: 18 Nov 2028
20 Nov 2023 | Latest version

Ask, share, connect.
Browse discussions, ask questions, and share experiences across hundreds of health topics.

Feeling unwell?
Assess your symptoms online for free
Sign up to the Patient newsletter
Your weekly dose of clear, trustworthy health advice - written to help you feel informed, confident and in control.
By subscribing you accept our Privacy Policy. You can unsubscribe at any time. We never sell your data.