Peripheral vasodilators
Peer reviewed by Dr Philippa Vincent, MRCGPLast updated by Dr Surangi Mendis, MRCGPLast updated 28 Sept 2023
Meets Patient’s editorial guidelines
- DownloadDownload
- Share
- Language
- Discussion
Peripheral vasodilators are medicines that are used to treat conditions that affect blood vessels in outer (peripheral) parts of the body such as the arms and legs. For example, they are used to treat peripheral arterial disease and Raynaud's phenomenon. They ease the symptoms of these conditions by dilating the blood vessels, preventing them from becoming narrower (constricting). These medicines are usually only prescribed after self-help measures have been tried and symptoms do not improve.

Unsure about mixing medicines?
Check for possible interactions between medicines, supplements and foods before taking them together.
In this article:
Video picks for Heart and blood medicines
What are peripheral vasodilators?
Peripheral vasodilators are used in peripheral arterial disease (PAD) and intermittent claudication to try to open up (dilate) the arteries; this helps to increase the distance you can walk before pain develops.
In Raynaud's phenomenon they are used to dilate the small blood vessels and prevent them from constricting. This helps to maintain the blood supply to the fingers, etc.
The peripheral vasodilator medications all reduce 'vascular resistance'. This is the resistance that should be overcome to push blood through the vessels in the limbs, to allow blood to flow.
There are a number of different peripheral vasodilator drugs. They include, nifedipine, cilostazol, moxisylyte, naftidrofuryl and pentoxifylline. These medicines are available as tablets and capsules and each one may have various other brand names (see Generic Medicines vs Brand Names).
Inositol nicotinate and pentoxifylline are not considered effective for PAD. Pentoxifylline and moxisylyte are not considered effective for Raynaud's phenomenon.
When are peripheral vasodilators usually prescribed?
Back to contentsIn cases of intermittent claudication, a vasodilator is usually only prescribed if self-help measures such as exercise have not improved the symptoms and surgery is not being considered.
However, they do not work in all cases. Therefore, there is no point in continuing with these medicines if an improvement in symptoms is not seen within a few weeks. If symptoms do not improve, stopping treatment would usually be advised. If symptoms improve, the treatment can be continued. The treatment is usually reviewed regularly to ensure that it is still being of benefit.
In Raynaud's phenomenon, nifedipine is usually only prescribed after self-help measures (such as keeping the whole body warm, including the hands and feet, and stopping smoking) have been tried and the symptoms have not improved. Usually a short course of nifedipine is prescribed to begin with to see if it works..
Continue reading below
How do peripheral vasodilators work?
Back to contentsPeripheral vasodilators work in slightly different ways to one another.
Cilostazol and inositol nicotinate work by widening the arteries that supply blood to the legs. Cilostazol also improves circulation by keeping platelets in the blood from sticking together and clotting.
Naftidrofuryl works by blocking the effects of a chemical called serotonin on the blood vessels. As a serotonin receptor blocker, Naftidrofuryl widens blood vessels to improve blood flow and also by allowing the body to make better use of oxygen available in the blood.
Nifedipine is a type of medicine called a calcium-channel blocker. It is sometimes used to treat high blood pressure but it is also a peripheral vasodilator. It works by widening the blood vessels and stopping them from going into a spasm or narrowing.
Moxisylyte is a type of medicine called an alpha-blocker. It works by relaxing the blood vessels, which in turn maintains the supply of blood to the fingers, toes, ears or nose.
Pentoxifylline works by decreasing the thickness of the blood. Blood is then able to flow more easily, especially in the small blood vessels of the hands and feet.
Which peripheral vasodilator is usually prescribed?
Back to contentsPeripheral arterial disease (PAD):
national guidelines only recommend the use of naftidrofuryl for people with intermittent claudication caused by PAD. Other peripheral vasodilators are not normally prescribed because there is little evidence that any of the others work very well for this condition. However, cilostazol can sometimes be used for the treatment of PAD in selected patients who do not respond to other treatments.
Raynaud's phenomenon:
Nifedipine is recommended to reduce the number and severity of 'vasospastic' attacks - when the blood vessels become narrow (constrict). Other peripheral vasodilators are not normally prescribed, as there is not much evidence to show that they work very well for Raynaud's phenomenon.
Sometimes, if the side-effects of nifedipine cannot be tolerated, a doctor may consider prescribing a different calcium-channel blocker such as nicardipine, amlodipine or felodipine. These medicines are not licensed to treat Raynaud's disease. Rarely, naftidrofuryl or inositol nicotinate may also be prescribed by some doctors to treat Raynaud's phenomenon.
Continue reading below
How should peripheral vasodilators be taken?
Back to contentsHow nifedipine is taken will depend upon the pattern of symptoms and how well symptoms improve with treatment.
All other vasodilators are taken every day.
What are the possible side-effects?
Back to contentsMost people who take peripheral vasodilators have no side-effects, or only minor ones. It is not possible in this leaflet to list all the possible side-effects of these medicines. For more detailed information, see the leaflet that comes within the medicine packet.
Nifedipine - some people develop flushing and headache. Serious side-effects are rare.
Naftidrofuryl - the most commonly reported side-effects are feeling sick, skin rash, stomach pains and runny stools (diarrhoea). On rare occasions, some people taking naftidrofuryl have developed a liver disorder. If any yellowing of the skin or the whites of the eyes is seen, speak with a doctor straightaway.
Cilostazol - the most common side-effects include headache and diarrhoea. Less common side-effects include dizziness, weakness, feeling or being sick, indigestion, tummy (abdominal) pain, fast heartbeat, chest pain, runny nose, bruising, swollen ankles or feet, skin rash and itching.
Inositol nicotinate - side-effects are thought to be uncommon but may include flushing, dizziness, headache, feeling sick, being sick (vomiting), fainting and a rash.
Moxisylyte - the most common side-effects include mild nausea, diarrhoea, dizziness with a spinning sensation (vertigo), headache, facial flushing and a rash. On rare occasions, some people taking moxisylyte have developed a liver disorder. If any yellowing of the skin or the whites of the eyes is seen, speak with a doctor straightaway.
Pentoxifylline - the most common side-effects include nausea, vomiting, and dizziness which may occur. Uncommonly, some people experience a fast or irregular heartbeat.
Other considerations - nifedipine
Back to contentsDrinking grapefruit juice can interact with nifedipine and alter its effect. Therefore, grapefruit juice should be avoided by anyone taking this particular vasodilator.
Can I buy peripheral vasodilators?
Back to contentsNo, you cannot buy oral peripheral vasodilators; you need a prescription to obtain these medicines.
Who cannot take peripheral vasodilators?
Back to contentsMost people are able to take a peripheral vasodilator; however, in some cases these medicines are best avoided.
Nifedipine - should not be given to people who:
Have severe damage to the heart muscle (cardiogenic shock).
Have a valve in the heart that does not open fully (advanced aortic stenosis).
Are within one month of having had a heart attack.
Have acute attacks of angina.
Naftidrofuryl - should not be given to people with a history of kidney stones.
Cilostazol - should not be given to people with:
Severe kidney or liver problems.
Uncontrolled high blood pressure.
A history of having had surgery in the previous three months.
A history of having had a stroke in the previous six months.
Inositol nicotinate - should not be given to people who have had a recent heart attack (myocardial infarction) or stroke.
Moxisylyte - is safe to use in most people.
Pentoxifylline - should not be given to people who have had:
A stroke.
Extensive back of the eye (retinal) bleeding.
A heart attack.
Heart rhythm problems.
For more detailed information, see the leaflet that comes with the medicine packet.
Patient picks for Heart and blood medicines
Treatment and medication
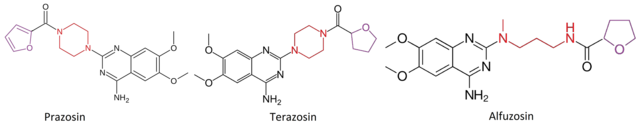
Alpha-blockers
Alpha-blockers are medicines that are mainly used to treat high blood pressure (hypertension) and problems with passing urine in men who have enlargement of the prostate gland. Prostate gland enlargement is also called benign prostatic hyperplasia (BPH).
by Dr Doug McKechnie, MRCGP
Treatment and medication
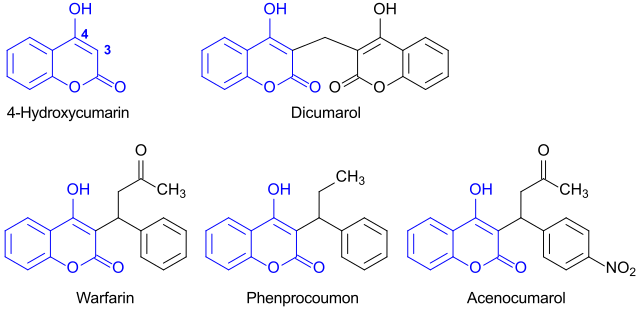
Anticoagulants
Anticoagulants are medicines that prevent the blood from clotting as quickly or as effectively as normal. Some people call anticoagulants blood thinners. However, the blood is not actually made any thinner - it just does not clot so easily whilst you take an anticoagulant. Anticoagulants are used to treat and prevent blood clots forming in blood vessels, such as in arteries or veins.
by Dr Doug McKechnie, MRCGP
Further reading and references
- Lower limb peripheral arterial disease; NICE Clinical Guideline (August 2012, updated December 2020)
- Aboyans V, Ricco JB, Bartelink MEL, et al; 2017 ESC Guidelines on the Diagnosis and Treatment of Peripheral Arterial Diseases, in collaboration with the European Society for Vascular Surgery (ESVS): Document covering atherosclerotic disease of extracranial carotid and vertebral, mesenteric, renal, upper and lower extremity arteriesEndorsed by: the European Stroke Organization (ESO)The Task Force for the Diagnosis and Treatment of Peripheral Arterial Diseases of the European Society of Cardiology (ESC) and of the European Society for Vascular Surgery (ESVS). Eur Heart J. 2017 Aug 26. doi: 10.1093/eurheartj/ehx095.
- Su KY, Sharma M, Kim HJ, et al; Vasodilators for primary Raynaud's phenomenon. Cochrane Database Syst Rev. 2021 May 17;5:CD006687. doi: 10.1002/14651858.CD006687.pub4.
- Raynaud's phenomenon; NICE CKS, November 2022 (UK access only)
- Peripheral Arterial Disease; NICE CKS, March 2024 (UK access only)
- Golledge J, Drovandi A; Evidence-Based Recommendations for Medical Management of Peripheral Artery Disease. J Atheroscler Thromb. 2021 Jun 1;28(6):573-583. doi: 10.5551/jat.62778. Epub 2021 Mar 21.
Continue reading below
Article history
The information on this page is written and peer reviewed by qualified clinicians.
Next review due: 26 Sept 2028
28 Sept 2023 | Latest version

Ask, share, connect.
Browse discussions, ask questions, and share experiences across hundreds of health topics.

Feeling unwell?
Assess your symptoms online for free
Sign up to the Patient newsletter
Your weekly dose of clear, trustworthy health advice - written to help you feel informed, confident and in control.
By subscribing you accept our Privacy Policy. You can unsubscribe at any time. We never sell your data.