
Are fertility apps a reliable form of contraception?
Peer reviewed by Dr Sarah Jarvis MBE, FRCGPLast updated by Sarah GrahamLast updated 1 Mar 2018
Meets Patient’s editorial guidelines
- DownloadDownload
- Share
- Language
- Discussion
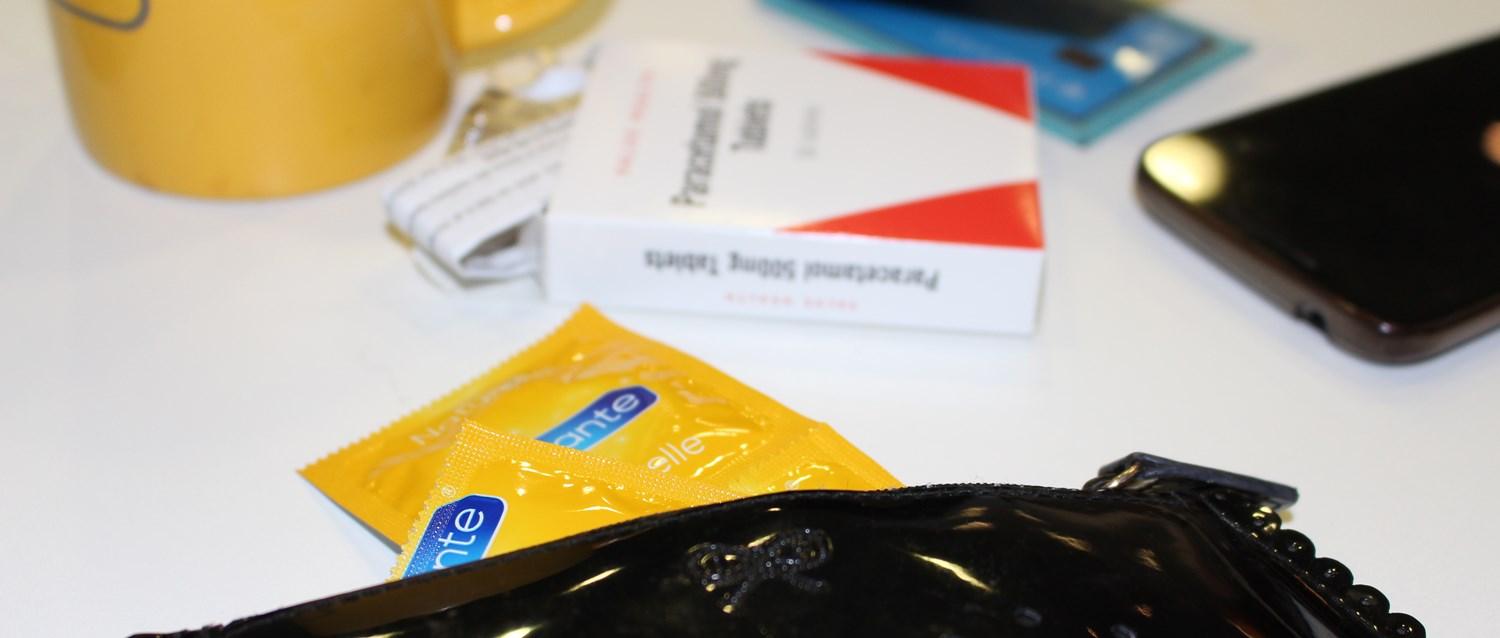
Hormonal contraception has had a bad press in recent years, with studies linking it to breast cancer and mental health side effects such as depression and anxiety. All that, combined with the rise of so-called 'fem tech', and the burgeoning trend for all things natural - from organic beauty products to 'clean' and plant-based diets - has led to an increased interest in more natural family planning options. But do any of them really work?
In this article:
Continue reading below
How worried should we be about hormonal contraception?
Holly Grigg-Spall is author of Sweetening the Pill, or how we got hooked on hormonal birth control. She came off the pill when she was 27, after experiencing a range of physical and mental health side effects, including "frequent urinary tract infections, headaches, really bad fatigue, lots of colds and infections ... depression symptoms, really bad anxiety, panic attacks, and worrying about social situations of leaving the house," she says.
For her, coming off hormonal contraception after a decade on the pill was genuinely life-changing, and she felt "100% better within six months". But, despite the scare stories that make it into the press, most women don't experience such extreme side effects. In fact, for many, the benefits of hormonal contraception far outweigh any downsides.
26-year-old Irene suffers from polycystic ovary syndrome (PCOS) and has been taking the pill for almost eight years. "For me, taking the pill is not a lifestyle choice; it's a medical necessity. PCOS causes very irregular or non-existent periods, which is associated with an increased risk of womb cancer; by taking the pill, I get a withdrawal bleed every month, eliminating that risk," Irene explains. "It's also really helped with other symptoms of PCOS like acne, and reduced my anxiety about being pregnant," she adds.
Another PCOS sufferer, 33-year-old Lizzie, says: "I've been on the 'mini pill' for nine years and it's the best thing - zero side effects [for me], massive positives. I'm not straight, so I don't take it as birth control, literally only for the non-reproductive positives like the joy of never having a period after years of really awful periods."
Clearly, a big part of the problem is that it's difficult to predict how individual women's bodies will react to different types of hormonal contraception - there's no one size fits all. But only you can decide whether the contraception you're on is having a positive or negative impact on your health. "There is no one right choice except the one that's right for that one particular woman," says Clare Murphy from the British Pregnancy Advisory Service (bpas).
Amy, 30, works as a contraceptive-trained midwife at bpas, and says she's tried all the hormonal types of contraception over the years. She's now on the contraceptive implant, and says the side effects she's experienced - including slight weight gain and erratic bleeding for the first few months - are, "a very small price to pay to know that I have the most reliable form of contraception." Professionally, she adds: "I'm so thankful that I am able to offer women a range of contraception types to suit their needs."
Of course, if hormonal contraception doesn't agree with you, there are alternatives. "If you're experiencing a side effect that you're not happy about, don't suffer in silence," says Bekki Burbidge, Deputy Chief Executive for the sexual health charity the Family Planning Association (fpa). "There are many different methods of contraception available - both hormonal and non-hormonal - so you should never feel like you have to keep using a method you're not happy with."
What's the natural alternative?
Back to contentsThe Fertility Awareness Method (FAM) is an increasingly popular option, and involves identifying biological signs of fertility (usually based on a temperature reading at the same time every day), and then abstaining or using condoms during the fertile period of each cycle. It's this that popular new contraceptive apps and devices such as Natural Cycles and Daysy are based on, and is up to 99% effective when used absolutely perfectly. But, as we'll explore later, 'perfect' use can be quite tricky for many women to attain.
Women's health practitioner Maisie Hill has been using FAM for more than ten years - including to plan a pregnancy - and now uses fertility calculator Daysy. "Daysy makes things easy because you don't have to learn the rules of FAM, although I still think it's wise to be educated about it. Instead, it learns your cycle for you and gives you a red or green light to indicate if it's a non-fertile time or not," she explains.
For Holly, the growing popularity of FAM is down to women feeling more empowered about knowing and understanding their own bodies. "What we used to see was women would come off [hormonal contraception] and use the [not reliable!] withdrawal method, or pullout method," she says. "Now we're seeing women taking more of an interest in getting to know their bodies and wanting to learn more about how our cycles naturally work."
Continue reading below
How effective is it?
Back to contentsBut fertility apps have not been without controversy either. Natural Cycles is currently the only app certified for contraception in Europe, yet sparked concerns last year after being linked to 37 unplanned pregnancies in Sweden.
A statement released by Natural Cycles in the aftermath of these reports, says: "With typical use, Natural Cycles has an efficacy of 93%. This means 7 out of 100 women become pregnant in a year due to all possible reasons (eg, having unprotected intercourse on red days, failure of the contraceptive method used on red days, etc). With perfect use, Natural Cycles has an efficacy of 99%."
Compared to the pill, they point out, that failure rate is similar - and it's important to remember that no form of contraception is 100% effective. However, the same study referred to by Natural Cycles also found a discontinuation rate of 54% after one year - perhaps because, even when using an app, the Fertility Awareness Method is more complex and involved than other forms of contraception.
"There's a lot more to think about; you've got to be really good at remembering to track your temperature and other fertility signs on a daily basis, and you can't really use it effectively for at least the first three months," warns Dr Diana Mansour, vice president of the Faculty of Sexual and Reproductive Healthcare (FSRH) for Clinical Quality. "You also must use barrier methods or abstain during the times when it's suggested you might be fertile, and you've got to have regular cycles," she adds.
For this reason, FAM is not much good for women affected by PCOS or irregular periods - and can in fact lead to more anxiety and uncertainty. 29-year-old Alex says: "I have been irregular all my life, and it's been a cause of great distress due to pregnancy fears. I use Natural Cycles, but I found I was habitually a week or so late, which would cause me a lot of stress."
Having been put off hormonal contraception, Alex turned to the internet for alternatives and discovered a community of women turning to traditional herbal remedies - using substances sold as 'natural supplements', such as rutin, dong quai, and high doses of vitamin C - to regulate their cycles.
"Although untested in the medical world, many of these methods have generations upon generations of wisdom behind them. They do work, even if somewhat unpredictably," Alex says. "When I take them, I don't feel sick, unbalanced, in pain, depressed, or any of the other things that morning after and contraceptive pills make me feel."
These kinds of herbal remedies were traditionally used as contraceptives, to induce miscarriages, or to treat menopausal symptoms, but they're not medically tested and Dr Mansour warns women could be putting themselves at risk by relying on them to prevent pregnancy.
"There really isn't any evidence they actually work as a contraceptive, and I do worry that people are going to either get pregnant using these things or come to some harm. Dong quai, for example, can cause bruising or put you at risk of bleeding," she explains.
Balancing the risks with the benefits
Back to contents"I think people often confuse natural with safe, [and vice versa]," Dr Mansour says. "There are huge positives to hormonal contraception that we don't hear so much about. With the combined pill, everyone worries about blood clot risks, but it's a very useful option in reducing symptoms from conditions like endometriosis," she explains.
"It has a protective effect against ovarian and uterine cancer, and there's also some evidence linking it to a reduction in colorectal cancer," Dr Mansour adds. "Recent work also suggested that Mirena® - the intrauterine system - is associated with a reduction in endometrial cancer, and it has reduced hysterectomy rates in the UK by 15%, which has to be good for women."
For women who are seeking a more 'natural' option, FAM can offer good protection against unwanted pregnancy when it's used perfectly, and many women like Maisie do find it empowering to learn more about the inner workings of their reproductive systems.
Alternatively, there are obviously barrier methods, such as condoms and diaphragms, as well as the non-hormonal coil or intrauterine device (IUD), which Dr Mansour says is an increasingly popular choice. "If pregnancy would be a disaster, the copper IUD is a very effective option for women who like the idea of not using hormones. It's very straightforward, it's there for between five and ten years, and it's immediately reversible," she says.
Ultimately, adds Clare: "What women need is evidence-based information and access to the services they need to make their own choices. A fit and forget method such as an implant may be perfect for some, while others may be very happy with a fertility app on their phone. Women who have made their own decision about their own contraception tend to use it in a pretty effective way."
Patient picks for Contraception
Sexual health
Which types of condoms are best for preventing pregnancy?
There are many different condoms to choose from, in a variety of colours, shapes and sizes. A condom helps to prevent sexually transmitted infections (STIs) and, when used correctly, helps protects against pregnancy 98% of the time. But the figures are often not as good in practice because condoms aren't always used correctly.
by Victoria Raw

Sexual health
Secret shoppers: Are women given the best contraception advice?
If you are sexually active and living in the UK today, you are fortunate to have a great variety of contraception available to you. Whether it’s a condom, pill or a longer-acting contraceptive such as an implant or intrauterine contraceptive device (sometimes known as the IUCD or coil), there are many different options. But are women always given the best advice? We sent four undercover shoppers, aged 16 to 30, to test the market and record their experiences.
by Dr Anna Cantlay, MRCGP
Continue reading below
Article history
The information on this page is peer reviewed by qualified clinicians.
1 Mar 2018 | Latest version

Ask, share, connect.
Browse discussions, ask questions, and share experiences across hundreds of health topics.

Feeling unwell?
Assess your symptoms online for free
Sign up to the Patient newsletter
Your weekly dose of clear, trustworthy health advice - written to help you feel informed, confident and in control.
By subscribing you accept our Privacy Policy. You can unsubscribe at any time. We never sell your data.