Acute pancreatitis
Peer reviewed by Dr Colin Tidy, MRCGPLast updated by Dr Philippa Vincent, MRCGPLast updated 5 Jan 2024
Meets Patient’s editorial guidelines
- DownloadDownload
- Share
- Language
- Discussion
In this series:GallstonesCholecystitisERCP
Acute pancreatitis is an inflammation of the pancreas that develops quickly. The main symptom is abdominal pain. It usually settles in a few days but sometimes it becomes severe and very serious. The most common causes of acute pancreatitis are gallstones and drinking alcohol above recommended limits.
In this article:
Video picks for Other digestive conditions
What is acute pancreatitis?
Pancreatitis means inflammation of the pancreas. Acute pancreatitis is inflammation that develops quickly, over 48 hours to a few days. It often goes away completely and leaves no permanent damage. Sometimes it can have longer lasting effects.
(In chronic pancreatitis, the inflammation is persistent - it tends to cause less intense symptoms than acute pancreatitis but has longer lasting symptoms).
How common is acute pancreatitis?
Back to contentsBetween 13-45 in 100,000 people have acute pancreatitis each year in the UK. Acute pancreatitis has become more common in recent years. This is partly due to an increase in the incidence of obesity.
Continue reading below
Acute pancreatitis symptoms
Back to contentsPeople with acute pancreatitis tend to experience the following symptoms:
Abdominal pain, just below the ribs, is the usual main symptom. It usually builds up quickly (over a few hours) and may last for several days. The pain can become severe and often spreads through to the back. The pain may be sudden and intense, or it may begin as a mild pain that is aggravated by eating and slowly grows worse. It is occasionally possible to have acute pancreatitis without any pain; this is more common in people with diabetes or kidney problems.
Being sick (vomiting).
A high temperature (fever) and generally feeling very unwell are common.
Swollen abdomen.
If the pancreatitis becomes severe and other organs become involved (for example, the heart, lungs or kidneys) then various other symptoms may develop. Dehydration and low blood pressure may develop.
Acute pancreatitis can cause people to become extremely unwell and can be life-threatening.
Causes of acute pancreatitis
Back to contentsGallstones or alcohol cause more than 8 in 10 cases of acute pancreatitis. Other causes of acute pancreatitis are relatively rare.
Gallstones
Gallstones are the most common cause of acute pancreatitis in the UK. A gallstone can pass through the bile duct and out into the duodenum (the part of the gut just after the stomach). This usually does not cause a problem.
However, in some people the gallstone becomes stuck in the bile duct or where the bile duct and pancreatic duct open into the duodenum. This can affect the chemicals (enzymes) in the pancreatic duct or even block them completely, and this can trigger acute pancreatitis.
Alcohol
About a third of cases of acute pancreatitis are associated with alcohol, although the relationship is not clear. It seems that, whilst alcohol itself does not damage the cells of the pancreas, it makes them more sensitive to damage from other causes such as smoking, high fat content in the blood or infections. Many patients with chronic alcoholic pancreatitis have a history of recurrent acute pancreatitis triggered by alcohol abuse.
High blood fat levels
This is known as hypertriglyceridaemia. It is reported to cause 1-4% of all cases of acute pancreatitis and up to 56% of pancreatitis cases during pregnancy.
Less common causes
These include the following:
Viral infections (for example, the mumps virus, HIV).
A rare side-effect to some medicines.
Injury or surgery around the pancreas.
Infections with parasites (parasites are living things (organisms) that live within (or on) another organism).
High levels of blood calcium.
Abnormal structure of the pancreas.
There is also a rare form of pancreatitis which can be inherited from a parent (hereditary).
Autoimmune
This is where the body's own immune system attacks the pancreas. This can be associated with other autoimmune diseases - for example, Sjögren's syndrome and primary biliary cirrhosis.
Unknown
This is where no cause is found and occurs in about 1 in 10 cases. However, a number of these cases are probably due to tiny gallstones or 'gallstone sludge' which passes through the bile duct but is too small to be seen on scans or other tests.
Continue reading below
What happens in acute pancreatitis?
Back to contentsThe digestive chemicals (enzymes) that are made in the pancreas become activated and start to 'digest' parts of the pancreas. These enzymes are normally only activated after they reach the part of the duodenum.
This leads to a range of chemical reactions that cause inflammation in the pancreas. How the above causes actually trigger this sequence of events is not clear.
In most pancreatitis cases (about 4 in 5), the inflammation is mild and settles within a week or so. Symptoms may be bad for a few days but then settle and the pancreas fully recovers.
In some pancreatitis cases (about 1 in 5), the inflammation quickly becomes severe. Parts of the pancreas and surrounding tissues may die (necrose). Pancreatic enzymes and chemicals may get into the bloodstream and cause inflammation and damage to other organs in the body. This can lead to shock and organ failure such as respiratory failure, kidney failure and other complications. This is a very serious situation which can be fatal.
What happens if acute pancreatitis is suspected?
Back to contentsAnyone with suspected acute pancreatitis will be admitted to hospital for tests to rule out other problems (as many conditions can cause similar symptoms) and to confirm the diagnosis.
Blood tests can check the blood level of amylase and/or lipase (these are digestive enzymes made by the pancreas). Although not 100% reliable, a high blood level of these enzymes would strongly suggest that pancreatitis is the cause of the symptoms.
An ultrasound scan may be done to look for a gallstone if this is the suspected underlying cause. Other types of scans such as CT scans may be needed if an ultrasound scan does not give a clear answer.
When should I call a doctor?
Back to contentsMedical advice should always be sought for persistent new severe abdominal pain.
Acute pancreatitis treatment
Back to contentsThe treatment depends on how bad the attack of acute pancreatitis is. There is no specific treatment that will take the inflammation away. However, in most cases the pancreatitis settles over a few days, although symptoms can get worse before they get better.
Strong painkillers by injection are usually needed to ease the pain.
A nasogastric tube (a feeding tube passed through the nose into the stomach) may occasionally also be passed to suck out the fluid from the stomach. This can be useful in someone who is being sick (vomiting) a lot.
A nasogastric tube may also be passed to provide food as people with acute pancreatitis are unable to eat properly.
A 'drip' is needed to give fluid into the body until symptoms settle.
A catheter - a thin tube going into your bladder to drain urine - is likely to be inserted so the doctors can monitor accurately the amount of urine being passed.
Less commonly, complications develop and the situation can become very serious. Other treatments that may then be needed include the following:
Intensive care treatment. Someone with a severe attack of pancreatitis will be monitored very closely in the intensive care unit.
A procedure to remove a blocked gallstone if this is found to be the cause.
Antibiotics if the pancreas or surrounding tissue becomes infected.
Surgery is sometimes needed to remove infected or damaged tissue.
Can pancreatitis be prevented?
Back to contentsAn attack of acute pancreatitis may be a one-off event. However, if there is an underlying cause, then it may happen again (recur) unless the cause is corrected. One of the following may be relevant to prevent a recurrence, depending on the cause:
An operation to remove the gallbladder is usually advised if a gallstone was the cause.
A high blood fat level (hyperlipidaemia) is sometimes the cause. This may need treating with medication.
A side-effect from some medication is a rare cause of acute pancreatitis. A change in medication may be needed if this is the cause of pancreatitis.
Alcohol-related concerns:
Alcohol should be completely avoided for at least several months after a bout of acute pancreatitis, even if alcohol was not the cause of the pancreatitis.
If alcohol is the cause of pancreatitis, alcohol should be stopped altogether permanently.
Sometimes a pancreatitis is the first indication of an alcohol dependency problem. Further help, advice and counselling may be offered if this is the case. It can be very difficult to stop drinking without some extra support.
What is the outlook (prognosis) for acute pancreatitis?
Back to contentsAcute pancreatitis is classified as mild if no complications develop (about 4 in 5 cases). In these cases the outlook is very good and full recovery is usual.
Severe acute pancreatitis (about 1 in 5 cases) means that one or more complications develop. Despite intensive care treatment, the mortality rate of people with severe acute pancreatitis is around a quarter.
What is the pancreas?
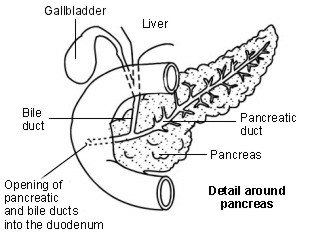
Back to contentsThe pancreas is in the upper abdomen and lies behind the stomach and guts (intestines). It makes a fluid that contains chemicals (enzymes) which are needed to digest food.
The enzymes are made in the pancreatic cells and are passed into tiny tubes (ducts). These ducts join together like branches of a tree to form the main pancreatic duct. This drains the enzyme-rich fluid into the part of the gut just after the stomach (called the duodenum). The enzymes are in an inactive form in the pancreas (otherwise they would digest the pancreas). They are 'activated' in the duodenum to digest food.
Groups of special cells called 'islets of Langerhans' are scattered throughout the pancreas. These cells make the hormones insulin and glucagon. The hormones are passed (secreted) directly into the bloodstream to control the blood sugar level.
The bile duct carries bile from the liver and gallbladder. This joins the pancreatic duct just before it opens into the duodenum. Bile also passes into the duodenum and helps to digest food.
Diagram showing detail around the pancreas
Patient picks for Other digestive conditions

Digestive health
Gastroparesis
Gastroparesis is now more commonly known as delayed gastric emptying. It is a chronic condition in which food passes through the stomach and into the gut (intestine) more slowly than usual. The nerves that usually trigger the stomach muscles to move food out of the stomach and into the intestine don't work as effectively as normal. This is not caused by an obstruction or structural abnormality but by a failure of the normal mechanisms.
by Dr Philippa Vincent, MRCGP

Digestive health
Mallory-Weiss tear
Mallory-Weiss syndrome (also called Mallory-Weiss tear) is the name given to bleeding and other symptoms caused by a tear in the lining of the upper part of the gut (gastrointestinal tract). It is usually diagnosed by having a test called a gastroscopy (endoscopy). This involves a tube being passed down through the gullet (oesophagus) into the stomach. In many cases, the bleeding has stopped by the time gastroscopy takes place and specific treatment is not needed. The tear usually heals by itself after a few days.
by Dr Philippa Vincent, MRCGP
Further reading and references
- Babu RY, Gupta R, Kang M, et al; Predictors of surgery in patients with severe acute pancreatitis managed by the step-up approach. Ann Surg. 2013 Apr;257(4):737-50. doi: 10.1097/SLA.0b013e318269d25d.
- Pancreatitis; NICE Guidance (Sept 2018 - last updated 16 December 2020)
- Clemens DL, Schneider KJ, Arkfeld CK, et al; Alcoholic pancreatitis: New insights into the pathogenesis and treatment. World J Gastrointest Pathophysiol. 2016 Feb 15;7(1):48-58. doi: 10.4291/wjgp.v7.i1.48.
- Ding N, Sun YH, Wen LM, et al; Assessment of prophylactic antibiotics administration for acute pancreatitis: a meta-analysis of randomized controlled trials. Chin Med J (Engl). 2020 Jan 20;133(2):212-220. doi: 10.1097/CM9.0000000000000603.
- Gapp J, Chandra S; Acute Pancreatitis. StatPearls, Jan 2020.
- Chatila AT, Bilal M, Guturu P; Evaluation and management of acute pancreatitis. World J Clin Cases. 2019 May 6;7(9):1006-1020. doi: 10.12998/wjcc.v7.i9.1006.
Continue reading below
Article history
The information on this page is written and peer reviewed by qualified clinicians.
Next review due: 2 Jan 2029
5 Jan 2024 | Latest version

Ask, share, connect.
Browse discussions, ask questions, and share experiences across hundreds of health topics.

Feeling unwell?
Assess your symptoms online for free
Sign up to the Patient newsletter
Your weekly dose of clear, trustworthy health advice - written to help you feel informed, confident and in control.
By subscribing you accept our Privacy Policy. You can unsubscribe at any time. We never sell your data.