Angina
Peer reviewed by Dr Toni Hazell, MRCGPLast updated by Dr Hayley Willacy, FRCGP Last updated 30 Jan 2023
Meets Patient’s editorial guidelines
- DownloadDownload
- Share
- Language
- Discussion
In this series:Microvascular anginaCoronary artery spasm
Angina is a pain that comes from the heart. It is usually caused by narrowing of the heart's blood vessels - the (coronary) arteries. Usual treatment includes a statin medicine to lower your cholesterol level, low-dose aspirin to help prevent a heart attack, and a beta-blocker medicine to help protect the heart and to prevent angina pains. An angiotensin-converting enzyme (ACE) inhibitor medicine is advised in some cases. Sometimes angioplasty or surgery are options to widen, or to bypass, narrowed arteries.
In this article:
What is angina?
Continue reading below
What is angina?
Angina is a pain that comes from the heart. Each year about 20,000 people in the UK develop angina for the first time. It is more common in people over the age of 50 years. It is also more common in men than in women. Sometimes it occurs in younger people.
This leaflet is about the common type of angina which is caused by narrowing in the coronary arteries of the heart. Sometimes angina can be caused by uncommon disorders of the heart valves or heart muscle.
What causes angina?
Heart with atheroma
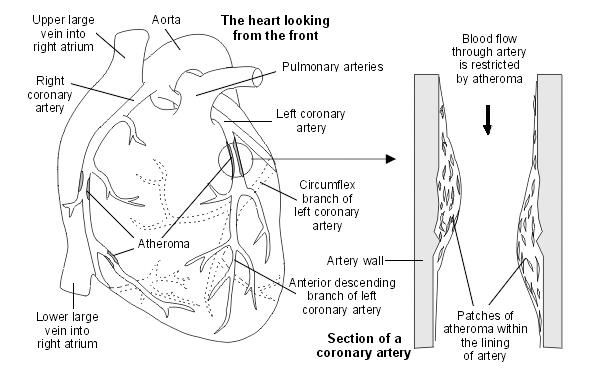
If you have angina, one or more of your heart (coronary) arteries are usually narrowed. This causes a reduced blood supply to a part, or parts, of your heart muscle.
The blood supply may be good enough when you are resting. When your heart works harder (when you walk fast or climb stairs and your heart rate increases) your heart muscle needs more blood and oxygen. If the extra blood that your heart needs cannot get past the narrowed coronary arteries, the heart responds with pain.
The narrowing of the arteries is caused by atheroma. See the separate leaflet called High Cholesterol for more information about atheroma.
Angina can also be caused by:
Spasm of the coronary arteries. Read more about coronary artery spasm.
Other problems with the blood supply to the heart. Read more about cardiac syndrome X (microvascular angina).
Continue reading below
Angina symptoms
Typical and common angina symptoms
Pain, ache, discomfort or tightness that you feel across the front of the chest.
The pain is usually worse when you exert yourself. For example, when you walk up a hill or against a strong, cold wind.
You may also, or just, feel the pain in your arms, jaw, neck or stomach.
An angina pain does not usually last long. It will usually ease within 10 minutes when you rest.
If you take some glyceryl trinitrate (GTN) it should go within 1-2 minutes (see 'Glyceryl trinitrate' section, below).
Angina pain may also be triggered by other causes of a faster heart rate - for example, when you have a vivid dream or an argument. The pains also tend to develop more easily after meals.
See also the separate leaflet called Chest Pain.
Less typical symptoms that sometimes occur
Some people have non-typical pains - for example, pains that develop when bending or eating.
If the symptoms are not typical then it is sometimes difficult to tell the difference between angina and other causes of chest pain, such as a pulled muscle in the chest or heartburn.
Some people with angina also become breathless when they exert themselves. Occasionally, this is the only symptom and there is no pain.
What tests will I have for angina?
If you have suspected angina, tests are usually advised:
Blood tests to check for anaemia, thyroid problems, kidney problems, a high blood sugar (glucose) level and a high cholesterol level, as these may be linked with angina.
A heart tracing (electrocardiogram, or ECG). This can be useful. However, a routine ECG may be normal if you have angina. In fact, more than half of people with angina have a normal resting ECG.
Continue reading below
How do doctors know that I have angina?
In many cases doctors can make the diagnosis based on the typical symptoms. No further tests may then be necessary. Tests are advised in some cases when the diagnosis is not clear, or sometimes to assess the severity of the condition. The tests that you have will depend on what is available locally and whether the test is suitable for you. One or more of these may be advised:
An ultrasound scan of the heart (echocardiogram, or 'echo').
A magnetic resonance imaging (MRI) scan can also show how your heart works under stress.
Exercise tolerance testing has been used for many years to diagnose and assess the severity of angina. However, this test is done less often these days due to more the more modern tests (listed above) becoming available. Current UK guidelines do not recommend using exercise testing to make the initial diagnosis of angina.
What can I do to help with angina?
Certain risk factors increase the risk of more fatty patches or plaques (atheroma) forming, which can make angina worse. See the separate leaflet called Cardiovascular Disease (Atheroma) for more details.
Briefly, risk factors that can be modified and may help to prevent angina from becoming worse include:
Smoking. If you smoke, you should make every effort to stop.
High blood pressure. Your blood pressure should be checked regularly, at least once a year, if you have angina. If it is high, it can be treated.
If you are overweight, losing some weight is advised. Losing weight will reduce the amount of workload on your heart and also help to lower your blood pressure.
High cholesterol. This should be treated if it is high.
Inactivity. You should aim to do some moderate physical activity on most days of the week for at least 30 minutes. For example, brisk walking, swimming, cycling, dancing, gardening, etc. (Occasionally, angina is due to a heart valve problem where physical activity may not be so good. Ask your doctor to confirm that you can undertake regular physical activity.)
Diet. You should aim to eat a healthy diet. A healthy diet means:
At least five portions (and ideally 7-9 portions) of a variety of fruit and vegetables per day.
You should not eat much fatty food such as fatty meats, cheeses, full-cream milk, fried food, butter, etc. Ideally you should use low-fat, mono-unsaturated or polyunsaturated spreads.
Try to include 2-3 portions of fish per week, at least one of which should be oily (such as herring, mackerel, sardines, kippers, salmon, or fresh tuna).
If you eat red meat, it is best to eat lean red meat, or eat poultry such as chicken.
If you do fry, choose a vegetable oil such as sunflower, rapeseed or olive.
Try not to add salt to food. Limit foods which are salty.
Alcohol definitely has a harmful effect on heart health when consumed above the recommended guideline amounts - ie 14 units per week maximum with at least two completely alcohol-free days in the week. However when alcohol is consumed at a lower level than that, the effect on risks is less clear.
Angina treatment
The main aims of treatment are:
To prevent angina pains as much as possible and to ease pain quickly if it occurs.
To limit further deposits of fatty patches or plaques (atheroma) as much as possible. This prevents or delays the condition from worsening.
To reduce the risk of having a heart attack (myocardial infarction).
Treatments that are advised in most cases
In addition to the lifestyle factors listed above, the treatments for angina include:
Glyceryl trinitrate (GTN) to relieve an angina episode.
Aspirin or another antiplatelet medicineto reduce the risk of blood clots.
A beta-blocker medicine to prevent the heart beating too fast.
Other treatments that may be advised
Other medicines to prevent angina pains
A beta-blocker may be sufficient to prevent angina pains but other medicines are available if required. They fall into three main groups:
Calcium-channel blockers (for example, amlodipine).
Nitrate medicines (for example, isosorbide mononitrate).
Potassium-channel activators (for example, nicorandil).
Non-medicine treatments
Coronary angioplasty or coronary artery bypass graft (CABG) surgery may be offered if:
You have pains not controlled by medicines; or
The site and severity of the atheroma deposits are particularly suited to one of these treatments. In some cases this may even be if you have few or no pains, as the overall outlook may be improved in certain circumstances.
Common worries about angina
Straining the heart by exertion
This is a common worry. On the contrary, more physical activity is usually advised. You will normally be encouraged to exercise regularly. Physical activity helps to make the heart fitter and improves the blood supply to the heart muscle.
Sex
Some people with angina worry that the physical effort of having sex will damage the heart. This is wrong and you do not need to stop having sex. If sex does bring on an angina pain, it may be helpful to take some GTN beforehand.
Driving and flying
There is usually no restriction for driving your own car unless pains occur at rest, with emotion or while driving. But, you must inform your insurance company if you have angina. People with PCV or LGV licences, who have angina, must stop driving and, in the UK, contact the DVLA.
As regards flying, in general, if you can climb 12 stairs and walk 100 metres on the level without pain or becoming very breathless, you are fit to fly as a passenger. People with frequent angina pains or unstable angina should avoid flying. Please note that your GP is not able to sign a form stating that you are fit to fly. This must be assessed by a doctor who has been specifically trained for this task.
Other points about angina
Stable angina and unstable angina
In most cases, angina pains come on with a certain amount of exertion and you can predict the level of exertion that triggers a pain. This situation is called stable angina. More than a million people in the UK have stable angina. It is common to have stable angina for many years and, with treatment, most pains can be prevented. Over months or years the pains may come on with a lesser amount of exertion if the condition gradually becomes worse.
If the pattern of your pain changes fairly suddenly and the pains develop after minimal exertion, or while you are resting, this is called unstable angina. This is an emergency and needs immediate medical care.
Prolonged pain
If you have a pain that lasts longer than 10 minutes, does not respond to your GTN or is different or more severe than usual, call an ambulance immediately. It may be unstable angina or a heart attack and immediate medical care is needed.
Immunisation
People with angina should have the pneumococcal immunisation and the annual flu immunisation.
Patient picks for Heart disease

Heart health and blood vessels
Cardiovascular disease
Cardiovascular diseases (CVD) is a general term to describe diseases of the heart or blood vessels. The cause of most cardiovascular disease is a build-up of atheroma - a fatty deposit within the inside lining of arteries. The blood flow to the heart muscle may also be restricted by a blood clot in an artery taking blood to the heart muscle (coronary artery disease). Atheroma or a blood clot may also restrict or prevent blood going to the brain (cerebrovascular disease) or to the legs and feet (peripheral arterial disease). There are lifestyle factors that can be taken to reduce the risk of forming atheroma. These include not smoking; choosing healthy foods; a low salt intake; regular physical activity; keeping your weight and waist size down; drinking alcohol in moderation. Your blood pressure and cholesterol level are also important. All people aged over 40 years should have a cardiovascular health risk assessment - usually available at your GP surgery. If you have a high risk of developing a cardiovascular disease, treatment to reduce high blood pressure (hypertension) and/or cholesterol may be advised.
by Dr Colin Tidy, MRCGP

Heart health and blood vessels
Aortic stenosis
The aortic valve is a heart valve that lies between the left ventricle and the aorta. In aortic stenosis, when the aortic valve opens to let blood pump through, it does not open as widely as it would normally. The opening between the left ventricle and the aorta is therefore narrowed (stenosed). The amount of blood that can pass from the left ventricle to the aorta is therefore reduced. The more narrowed the valve, the smaller the amount of blood that can get through, and the more significant the symptoms. In some cases, aortic stenosis occurs at the same time as aortic regurgitation.
by Dr Philippa Vincent, MRCGP
Further reading and references
- Assessing fitness to drive: guide for medical professionals; Driver and Vehicle Licensing Agency
- Management of stable angina; Scottish Intercollegiate Guidelines Network - SIGN (April 2018)
- Saraste A, Knuuti J; ESC 2019 guidelines for the diagnosis and management of chronic coronary syndromes : Recommendations for cardiovascular imaging. Herz. 2020 Aug;45(5):409-420. doi: 10.1007/s00059-020-04935-x.
- Angina; NICE CKS, October 2022 (UK access only)
- Mahtani AU, Padda IS, Johal GS; Cardiac Syndrome X.
- Hoek AG, van Oort S, Mukamal KJ, et al; Alcohol Consumption and Cardiovascular Disease Risk: Placing New Data in Context. Curr Atheroscler Rep. 2022 Jan;24(1):51-59. doi: 10.1007/s11883-022-00992-1. Epub 2022 Feb 7.
Continue reading below
Article history
The information on this page is written and peer reviewed by qualified clinicians.
Next review due: 29 Jan 2028
30 Jan 2023 | Latest version

Ask, share, connect.
Browse discussions, ask questions, and share experiences across hundreds of health topics.

Feeling unwell?
Assess your symptoms online for free
Sign up to the Patient newsletter
Your weekly dose of clear, trustworthy health advice - written to help you feel informed, confident and in control.
By subscribing you accept our Privacy Policy. You can unsubscribe at any time. We never sell your data.