Spinal disc problems
Peer reviewed by Dr Colin Tidy, MRCGPLast updated by Dr Hayley Willacy, FRCGP Last updated 17 Nov 2024
Meets Patient’s editorial guidelines
- DownloadDownload
- Share
- Language
- Discussion
- Audio Version
Spinal discs are also called intervertebral discs. There is a spinal disc between each bone (vertebra) in your spine. This keeps the vertebrae separated and acts as a shock absorber. As we get older the spinal discs gradually become damaged and this can cause problems such as back pain. Other problems affecting the spinal discs include a slipped disc or, much more rarely, infection (discitis).
In this article:
Video picks for Back and spine
Continue reading below
What are spinal discs?
Lumbar spine and spinal cord
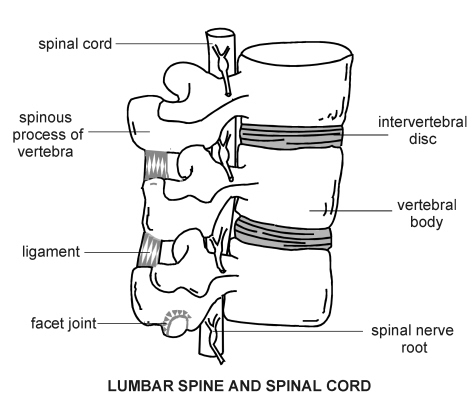
The spinal discs lie between the vertebrae in your spine. Spinal discs are also called intervertebral discs. A spinal disc acts as shock absorber between each of the vertebrae in the spinal column. Each disc keeps the vertebrae separated. The spinal discs also protect the nerves that run down the middle of the spine and the nerves that pass out of each level of the spinal column.
The spinal cord is shorter than the spinal canal. The cord ends between the first and second lumbar vertebrae in adults and between the second and third lumbar vertebrae in children. Below the end of the spinal cord, the nerve roots form what is called the cauda equina (because it looks like a horse's tail). Any problem with the spine below the first lumbar vertebra can cause weakness in the legs and also bladder or bowel upset. This is called cauda equina syndrome.
What are the causes of spinal disc problems?
Back to contentsThe main causes of spinal disc problems include:
Slipped disc (prolapsed disc).
Degenerative disc disease. As we get older the spinal discs become damaged and weaker (degenerate).
Infection of the spinal disc (discitis). The infection is usually caused by a germ (bacterium) but is sometimes caused by a viral infection. See the end of this leaflet for more information about discitis.
A prolapsed disc
A 'slipped' (prolapsed) disc often causes severe lower back pain. The disc often presses on a nerve root which can cause pain and other symptoms in a leg. For more information see the separate leaflet called Slipped disc (Prolapsed disc).
Degenerative disc disease
As we get older our spinal discs begin to shrink. The disc dries out and doesn't absorb shocks as well. Over a period of time this degeneration can be aggravated by sports and our daily activities. Injuries to our back can also cause the discs to degenerate more quickly. There is very little blood supply to the disc. So, once a disc is injured it cannot repair itself and the disc can start to deteriorate.
Nearly everyone has some signs of wear and tear of the spinal discs as they get older. Almost everyone older than 60 years has some degeneration of the discs, but not all people with disc degeneration will have back pain. In some cases, the discs may collapse completely and cause the facet joints in the vertebrae to rub against one another. This causes arthritis of the facet joints.
Continue reading below
What are the symptoms of spinal disc problems?
Back to contentsSpinal disc problems can lead to symptoms of back pain, most often low back pain. The pain may also go into one or both of your legs (sciatica). Back pain with or without sciatica is very common. Most causes are not serious but it is very important for any serious cause to be found early so that it can be treated.
Nerve pain occurs if the affected disc is pressing on a nerve. The most common nerve pain caused by disc problems is sciatica - where the affected disc presses on your sciatic nerve, causing pain radiating into your leg. This nerve travels from your spine to your hip and buttock and down your leg.
The pain can be sudden and sharp, and move down the nerve to your leg and sometimes down to your foot. The pressure of the disc on the nerve may also cause numbness and tingling.
Sciatica is caused by a problem with a disc in your lower back (lumbar spine). A similar problem with a disc in your neck (cervical spine) may cause pain, numbness and tingling in your arm.
What are red flags?
Back to contents'Red flags' are symptoms which may suggest that there is a serious underlying condition that is causing your symptoms.
Red flags that suggest cauda equina syndrome
Severe or worsening weakness of both legs.
Being unable to empty your bladder.
Loss of the feeling when you empty your bladder.
Losing control of your bladder (urinary incontinence).
Losing control of your bowels (faecal incontinence). This is caused by a loss of feeling of your rectum being full and weakness (laxity) of your back passage (anus).
Red flags that suggest spinal fracture
Sudden severe pain in your spine which is relieved by lying down.
History of major or minor injury - or even just strenuous lifting if you have 'thinning' of the bones (osteoporosis).
Localised tenderness over one of your vertebrae.
Red flags that suggest cancer or infection
(Infection includes conditions such as discitis, vertebral osteomyelitis, or spinal epidural abscess.)
Onset of symptoms in people aged older than 50 years, or younger than 20 years.
Pain that remains when you are lying down, night pain that disturbs your sleep, or pain in your spine in your upper or middle back (thoracic spine).
Past history of cancer.
High temperature (fever) or unexplained weight loss.
Recent infection (for example, urinary tract infection).
Drug abuse when the drug is injected into a vein.
Weak body defence against infection (immune deficiency).
Red flags that suggest arthritis affecting the spine
Early morning stiffness lasting longer than 45 minutes.
Pain during the night.
Pain that improves when you are moving and is worse after resting.
Red flags that suggest a high risk of permanent nerve damage
Muscle weakness or wasting.
Continue reading below
Do you need any tests for spinal disc problems?
Back to contentsSometimes no tests are needed but this will depend on your symptoms.
Initial tests may include blood tests. X-rays of your spine aren't usually recommended but you may need a magnetic resonance imaging (MRI) scan which will help to confirm the diagnosis and decide on the best treatment
What are the treatment options?
Back to contentsIf there are red flag symptoms and signs that may suggest a serious underlying cause, you will need to be admitted urgently to hospital, or referred urgently to a neurosurgery or back specialist (an orthopaedic spinal specialist).
Otherwise, the initial treatment is usually painkillers, simple back exercises and advice for you to keep as normally active and mobile as you can,
If the pain or any restrictions caused by the problem with your back last for more than 1-2 weeks the treatment options include:
Physiotherapy.
Referral to a specialist for an epidural corticosteroid injection.
Further treatment may be needed from an orthopaedic spinal specialist or a pain specialist.
What are the possible complications?
Back to contentsPermanent nerve damage may be caused by prolonged and severe disc problems.
The pain and restrictions may lead to psychological and social problems - for example, depression and being unable to continue with socialising and hobbies.
The pain and restrictions may also prevent you from working.
What is the outlook?
Back to contentsThe outlook (prognosis) is good for most people. However, some people will continue to have pain for longer than one year and sometimes much longer. The outlook tends to be worse for people who initially have more severe pain and have a greater restriction of daily activities.
Can spinal disc problems be prevented?
Back to contentsWe should all take good care of our back. The ways we can do this include:
Regular exercise.
Weight loss if you are overweight.
Safe lifting techniques (such as bending your knees when lifting objects).
Correct sitting position and posture.
Discitis
Back to contentsInflammation of a spinal disc (discitis) is rare. It is often caused by infection with a germ (a bacterial infection). Sometimes, however, the infection may be caused by a virus. Occasionally discitis is not caused by infection but results from a chemical reaction when you have a spinal injection.
Infection of the disc may occur after back surgery or a needle placed in the back for a lumbar puncture or spinal injection. Infection can also spread from other sites in your body via the bloodstream - for example, a urinary tract infection or throat infection.
Discitis is more common in people with diabetes, in any condition reducing the body's defence against infection (immune deficiency) and in people with peripheral arterial disease. Drug misuse and alcohol misuse are also risk factors.
Severe, almost unbearable back pain is usually the main symptom of discitis. The pain is usually just in the area of the affected spinal disc and doesn't travel down your leg or to any other parts of your body. Other symptoms can include changes in your posture, stiffness in your back, difficulty performing your daily tasks, tummy (abdominal) pain or discomfort, and high temperature (fever).
Infection of the disc can be very difficult to treat. It usually takes a long course of antibiotics, usually given by injection into a vein (intravenously). Usually a period of six to eight weeks of antibiotic treatment is needed. Strong painkillers are often needed and other treatments may include surgery.
Patient picks for Back and spine

Bones, joints and muscles
Axial spondyloarthritis
Axial spondyloarthritis (also known as axSpA or axial SpA) is a painful, chronic arthritis that mainly affects the joints of the spine, and also the joints connecting each side of the base of the spine with the pelvis (sacroiliac joints). It can also affect other joints in the body, as well as tendons and ligaments. It is divided into: 1) Ankylosing spondylitis. 2) Non radiographic axial spondyloarthritis.
by Dr Philippa Vincent, MRCGP
Bones, joints and muscles
Scoliosis and kyphosis
Scoliosis is a back condition that causes the (back) spine to curve to the side - either left or right. Most cases develop in children between the ages of 9 and 14 years during the growth spurt of puberty. Scoliosis is usually mild and needs no treatment. For more severe cases treatments include specific exercises, a back brace or occasionally surgery to straighten the spine. A very pronounced front-to-back curve is called a kyphosis, which does not usually need treatment.
by Dr Colin Tidy, MRCGP
Further reading and references
- Low back pain and sciatica in over 16s: assessment and management; NICE Guidelines (November 2016 - last updated December 2020)
- Molinos M, Almeida CR, Caldeira J, et al; Inflammation in intervertebral disc degeneration and regeneration. J R Soc Interface. 2015 Mar 6;12(104):20141191. doi: 10.1098/rsif.2014.1191.
- Back pain - low (without radiculopathy); NICE CKS, September 2023 (UK access only)
- Sciatica (lumbar radiculopathy); NICE CKS, September 2023 (UK access only)
Continue reading below
Article history
The information on this page is written and peer reviewed by qualified clinicians.
Next review due: 16 Nov 2027
17 Nov 2024 | Latest version

Ask, share, connect.
Browse discussions, ask questions, and share experiences across hundreds of health topics.

Feeling unwell?
Assess your symptoms online for free
Sign up to the Patient newsletter
Your weekly dose of clear, trustworthy health advice - written to help you feel informed, confident and in control.
By subscribing you accept our Privacy Policy. You can unsubscribe at any time. We never sell your data.