Multiple sclerosis
MS
Peer reviewed by Dr Colin Tidy, MRCGPLast updated by Dr Hayley Willacy, FRCGP Last updated 24 Jul 2025
Meets Patient’s editorial guidelines
- DownloadDownload
- Share
- Language
- Discussion
Multiple sclerosis is a disorder of the brain and spinal cord. It can cause various symptoms. In most cases, episodes of symptoms come and go for several years. In time, some symptoms can become permanent and can cause disability. Although there is no cure for multiple sclerosis, various medicines and therapies may reduce the number of flare-ups and can help to ease symptoms and disability.
In this article:
Continue reading below
What is multiple sclerosis?
Multiple sclerosis (MS) is a disease where patches of inflammation occur in parts of your brain and/or spinal cord. This can cause damage to parts of your brain and lead to various symptoms (described below).
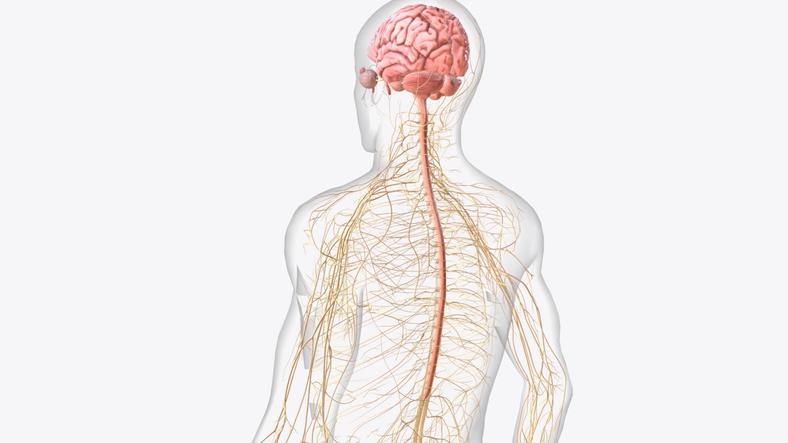
Understanding the brain, spinal cord, and nerves
Many thousands of nerve fibres transmit tiny electrical messages (impulses) between different parts of your brain and spinal cord. Each nerve fibre in the brain and spinal cord is surrounded by a protective sheath made from a substance called myelin. The myelin sheath acts like the insulation around an electrical wire. It is needed for the electrical impulses to travel correctly along your nerve fibres.
Nerves are made up from many nerve fibres. Nerves come out of your brain and spinal cord and take messages to and from your muscles, skin, body organs and tissues.
Continue reading below
What causes multiple sclerosis?
The exact cause of multiple sclerosis (MS) is unknown. Inflammation that is enabled by the immune system is triggered by an abnormal response to environmental factors. This only occurs in those who are susceptible because of their inherited genes.
When the multiple sclerosis is active, parts of the immune system, mainly T cells, attack the myelin sheath which surrounds the nerve fibres in the brain and spinal cord. This is why these types of conditions are called demyelinating diseases.
The inflammation around the myelin sheath prevents the affected nerve fibres from working properly and symptoms develop. When the inflammation clears, the myelin sheath may heal and repair and nerve fibres start to work again. However, the inflammation, or repeated bouts of inflammation, can leave a small scar (sclerosis) which can permanently damage nerve fibres. In a typical person with multiple sclerosis (MS), many (multiple) small areas of scarring develop in the brain and spinal cord. These scars may also be called plaques.
What is multiple sclerosis like?
MS tends to follow one of the following four patterns.
Relapsing-remitting MS
Nearly 9 in 10 people with multiple sclerosis (MS) have the relapsing-remitting form of the disease. In a relapse, an attack (episode) of symptoms occurs. During a relapse, symptoms develop (described below) and may last for days but usually last for 2-6 weeks. They sometimes last for several months. Symptoms of MS then improve or go away which is remission. Further relapses then occur from time to time.
The type and number of symptoms that occur during a relapse of multiple sclerosis vary from person to person. The frequency of relapses also varies. Having one or two relapses every two years is fairly typical. However, relapses can occur more or less often than this. When a relapse occurs, previous symptoms may return, or new ones may appear.
The relapsing-remitting MS pattern tends to last for several years. At first, full recovery from symptoms, or nearly full recovery, is typical following each relapse. In time, in addition to myelin damage, there may also be damage to the nerve fibres themselves.
Eventually, often after 5-15 years, some symptoms may become permanent. The permanent symptoms are due to accumulation of scar tissue in the brain and to the gradual nerve damage that occurs. The condition typically then slowly becomes worse over time and can affect life expectancy. This is called secondary progressive MS. Typically, about two thirds of people with relapsing-remitting multiple sclerosis will have developed secondary progressive MS after 15 years.
Benign MS
10-15% of patients have benign relapsing-remitting MS or 'benign MS'. Benign MS is a variation of relapsing-remitting MS where relapses are very mild, there are very long periods between relapses and/or only a few relapses ever occur.
Secondary progressive form of MS
In this form of multiple sclerosis there is a steady worsening of your symptoms (with or without relapses). Many people with the relapsing-remitting form later develop this type of MS.
Primary progressive form of MS
Primary progressive MS occurs in about 1 in 10 people with multiple sclerosis. There is no initial relapsing-remitting course and the symptoms become gradually worse from the outset and do not recover.
Continue reading below
How common is multiple sclerosis?
Multiple sclerosis (MS) is the most common disabling illness of young adults in the UK. About 1 in 500 people in the UK develop multiple sclerosis. It can affect anyone at any age, although it is rare in young children. It often first develops in people aged between 30 and 50. It is more than twice as common in women as in men.
Is multiple sclerosis hereditary?
Multiple sclerosis is not strictly an hereditary disease. However, you have an increased chance of MS developing if you have a close relative with MS. For example, if your mother, father, brother or sister has MS, then you have about a 2 in 100 chance of developing MS (compared with about a 1 in 500 chance in the general population).
What are the symptoms of multiple sclerosis?
Multiple sclerosis causes a wide variety of symptoms. Many people experience only a few symptoms and it is very unlikely that you would develop all the symptoms described here. Symptoms of MS are usually unpredictable.
MS symptoms may worsen gradually with time. More commonly, symptoms come and go at different times.
Multiple sclerosis relapses can occur at any time and your symptoms may differ within each relapse. Although relapses usually occur for no apparent reason, various triggers can include infection, exercise and hot weather. The symptoms that occur during a relapse depend on which part, or parts, of your brain or spinal cord are affected. You may have just one symptom in one part of your body, or several symptoms in different parts of your body. The symptoms occur because the affected nerve fibres stop working properly.
The more common symptoms of multiple sclerosis include:
Visual problems
The first symptom of multiple sclerosis for around one in four people with MS is a disturbance of vision. Inflammation (swelling) of the optic nerve can occur. This is called optic neuritis. This can cause pain behind your eye and also some loss of your vision. This usually only affects one eye. Other eye symptoms may include blurring of your vision or having double vision.
Muscle spasms and spasticity
Tremors or spasms of some of your muscles may occur in MS. This is usually due to damage to the nerves that supply these muscles. Some muscles may shorten (contract) tightly and can then become stiff and harder to use. This is called spasticity.
Pain
There are two main types of pain that may occur in people with multiple sclerosis:
Neuropathic pain - this occurs due to damage to the nerve fibres. This can cause stabbing pains or a burning sensation over parts of your skin. Areas of skin may also become very sensitive.
Musculoskeletal pain - this type of pain can occur in any of your muscles that are affected by spasms or spasticity.
Fatigue
Extreme tiredness (fatigue) is one of the most common symptoms of MS. This tiredness with multiple sclerosis is more than the tiredness expected after exercising or exertion. This fatigue can even affect balance and concentration. There are different treatments for fatigue which are often a combination of self-management strategies, physiotherapy and exercise.
Emotional problems and depression
People with multiple sclerosis might laugh or cry more easily, even for no reason. Also, many people with MS have symptoms of depression or anxiety at some stage. Acknowledging this and asking for support is important. Your GP can discuss the treatment options available.
Other symptoms of multiple sclerosis which may occur include:
Numbness or tingling in parts of your skin. This is the most common symptom of a first relapse.
Weakness or paralysis of muscles. Mobility may be affected.
Problems with your balance and co-ordination.
Problems with your concentration and attention.
Tremors or spasms of some of your muscles.
Dizziness.
Problems with passing urine.
Difficulty with speaking.
Secondary MS symptoms
These are symptoms that may develop later in the course of the disease when some of the above symptoms become permanent. Symptoms including contractures, urine infections, bone fragility (osteoporosis), muscle wasting and reduced mobility may be experienced.
How is multiple sclerosis diagnosed?
Almost all the symptoms that can occur with MS can also occur with other diseases. It is often difficult to be sure if a first episode of symptoms (a first relapse) is due to MS. For example, an episode of numbness in a leg, or blurring of vision for a few weeks, may have been the first relapse of MS or just a one-off illness that was not MS.
A firm diagnosis of MS is often not made until two or more relapses have occurred. So, there may be months, or years, of uncertainty when there is an episode of symptoms and the diagnosis is not yet clear. This can be a very difficult time for many people.
Can you test for multiple sclerosis?
In most cases, no test can definitely prove that you have multiple sclerosis after a first episode of symptoms or in the very early stages of the disease. However, some tests are helpful and may indicate that MS is a possible, or probable, cause of the symptoms.
A magnetic resonance imaging (MRI) scan of the brain is a useful test. This type of scan can detect small areas of inflammation and scarring in your brain which occur in multiple sclerosis. Although very useful in helping to make a diagnosis of MS, MRI scans are not always conclusive, especially in the early stages of the disease. A scan result should always be viewed together with your symptoms and physical examination.
Since MRI scans became available, other tests for multiple sclerosis are now done less often. However, they are sometimes done and include:
Lumbar puncture. In this test a needle is inserted, under local anaesthetic, into the lower part of your back. It takes a sample of some of the fluid that surrounds your brain and spinal cord. This is called cerebrospinal fluid (CSF). Certain protein levels are measured. Some proteins are altered in multiple sclerosis, although they can be altered in other conditions too.
Visual evoked potentials test. In this test, electrodes measure if there is slowing or any abnormal pattern in the electrical impulses in the optic nerves.
Can multiple sclerosis be treated?
At present there is no cure for multiple sclerosis. However many symptoms of MS can be eased to improve quality of life and make living with MS more manageable. Treatments generally fall into four categories:
Medicines that aim to modify the disease process.
Steroid medication to treat relapses.
Other medicines to help ease symptoms.
Other therapies and general support to minimise disability.
Medicines that aim to modify the disease process
These medicines are known as immunomodulatory agents. They do not cure MS and they are not suitable for everyone with MS.
Fingolimod, Ponesimod, Teriflunomide, Diroximel fumarate and Dimethyl fumarate are the only tablet forms of disease-modifying treatment. All the others are given by injection.
Natalizumab, Alemtuzumab, Ofatumumab, Ublituximab and Ocrelizumab are given by injection and are used for patients with more advanced or active disease.
Newer medicines and combinations of medicines are also being developed and studied.
Studies have shown that these medicines reduce the number of relapses for some people. They may also have a small effect on slowing the progression of the disease. The exact way in which they work is not always clear but they all interfere with the immune system in some way.
As there is still some uncertainty as to the role of these medicines and how effective they are, guidelines have been drawn up as to when they may be prescribed on the NHS. A consultant neurologist will advise on which of the treatments are recommended. Each of the different disease-modifying medicines has pros and cons. The Multiple Sclerosis Trust (see under 'Further Reading', below) provides an MS Decisions page which is designed to help you decide which is the best medicine for you.
If any of these treatments are prescribed, further monitoring and review also happens. With the help of this monitoring, over time, it should become clear how effective the treatments are.
Steroids for multiple sclerosis (sometimes called corticosteroids)
A steroid is often prescribed if there is a relapse which causes disability. A high dose is usually given for a few days. Sometimes steroid tablets are used or the steroid may be given through veins. The steroids work by reducing inflammation. A course of steroids will usually shorten the duration of a relapse. This means that symptoms usually improve more quickly than they would otherwise have done.
However, steroids do not affect the ongoing progression of the disease.
Other treatments to improve MS symptoms
Depending on which symptoms develop, other treatments may be advised. For example:
Anti-spasm medicines.
Painkillers. There are specific types of painkillers which can improve neuropathic pain.
Medicines which can help with some urinary problems that may develop.
Medicines to help with erectile problems.
Cannabis-based products
NICE provided guidance on the use of cannabis-related medicinal products for muscle spasticity in MS. The guidance recommends that people with moderate-to-severe muscle spasticity (which has not responded to other treatments), may be offered treatment with a cannabis-based mouth spray called Sativex® for four weeks. If the symptoms improve by at least 20% in this time, longer-term treatment may be offered.
This treatment should be started and supervised by an MS specialist doctor. Find out more about this treatment in our separate leaflet called Cannabis-based medicinal products (Medicinal marijuana).
Other treatments, therapies and support
Other therapies that may be offered include:
Speech therapy.
Specialist nurse advice and support.
Psychological therapies.
Counselling.
Driving
If you drive a car or ride a motorcycle, you must tell the DVLA that you have multiple sclerosis. However you can continue to drive or ride a motorcycle as long as you can drive safely at all times.
Multiple sclerosis outlook (prognosis)
Multiple sclerosis affects different people in many different ways. This means that it is very difficult to predict your outlook (prognosis) if you have MS. There are currently no tests to predict how your MS will progress.
Many people with MS will be able to continue to walk and function at their work for many years after their diagnosis.
However, some people with MS do become disabled over time, and a minority become severely disabled.
The treatment of MS is a rapidly developing area of medicine. The research into newer and better disease-modifying treatments brings a great deal of hope that the outlook for people with MS will continue to improve in the future and hopefully slow the progress of symptoms. The specialist who knows your case can give more accurate information about the outlook for your particular situation.
Patient picks for Limb weakness and numbness
Brain and nerves
Motor neurone disease
Motor neurone disease (MND) is a neurological condition causes a progressive weakness and wasting of many of the muscles in the body. There are various types of motor neurone disease. This leaflet is mainly about amyotrophic lateral sclerosis (ALS), which is the most common type of motor neurone disease. Although there is no cure for motor neurone disease, treatments can help to ease symptoms and disability.
by Dr Rachel Hudson, MRCGP

Brain and nerves
Cauda equina syndrome
Cauda equina syndrome is a particularly serious type of nerve root problem. This is a rare disorder where there is pressure on the nerves at the very bottom of the spinal cord. The collection of nerves at the bottom of the spinal cord is called the cauda equina because it is said to look like a horse's tail. Cauda equina means horse's tail in Latin. The condition may cause low back pain and problems with bowel and bladder function (usually not being able to pass urine), numbness in the saddle area, which is around the back passage (anus), and weakness in one or both legs. It needs urgent investigation and treatment to prevent the nerves to the bladder and bowel from becoming permanently damaged. See a healthcare professional immediately if you suspect CES.
by Dr Colin Tidy, MRCGP
Further reading and references
- Multiple sclerosis; NICE CKS, May 2024 (UK access only)
- Multiple sclerosis in adults: management; NICE guideline (June 2022)
- Assessing fitness to drive: guide for medical professionals; Driver and Vehicle Licensing Agency
- Multiple Sclerosis Society
- Lunde HMB, Assmus J, Myhr KM, et al; Survival and cause of death in multiple sclerosis: a 60-year longitudinal population study. J Neurol Neurosurg Psychiatry. 2017 Aug;88(8):621-625. doi: 10.1136/jnnp-2016-315238. Epub 2017 Apr 1.
- Introducing MS Decisions; Multiple Sclerosis Trust
Continue reading below
Article history
The information on this page is written and peer reviewed by qualified clinicians.
Next review due: 23 Jul 2028
24 Jul 2025 | Latest version

Ask, share, connect.
Browse discussions, ask questions, and share experiences across hundreds of health topics.

Feeling unwell?
Assess your symptoms online for free
Sign up to the Patient newsletter
Your weekly dose of clear, trustworthy health advice - written to help you feel informed, confident and in control.
By subscribing you accept our Privacy Policy. You can unsubscribe at any time. We never sell your data.