Plantar fasciitis
Peer reviewed by Dr Laurence KnottLast updated by Dr Colin Tidy, MRCGPLast updated 18 Jan 2022
Meets Patient’s editorial guidelines
- DownloadDownload
- Share
- Language
- Discussion
- Audio Version
Medical Professionals
Professional Reference articles are designed for health professionals to use. They are written by UK doctors and based on research evidence, UK and European Guidelines. You may find the Plantar fasciitis article more useful, or one of our other health articles.
In this article:
Continue reading below
What is plantar fasciitis?
Plantar fasciitis continues to be widely used for the clinical syndrome of undersurface heel pain. However, the use of 'itis' denotes an inflammatory disorder. This is a misnomer as the pathology is not the result of excessive inflammation. Pathological changes are degenerative (but partially reversible) in nature, probably due to repetitive trauma1 .
The plantar fascia is a thick, fibrous band of connective tissue. Its origin is the medial plantar tubercle of the calcaneum. It runs along the sole of the foot like a fan, being attached at its other end to the base of each of the toes. It is a tough, resilient structure that has a number of critical functions during running and walking:
It stabilises the metatarsal joints during impact with the ground.
It acts as a shock absorber for the entire leg.
It forms the longitudinal arch of the foot and helps to lift the arch to prepare it for the 'take-off' phase of the gait cycle.
Plantar fasciitis pathophysiology
Back to contentsPlantar fascia and Achilles tendon
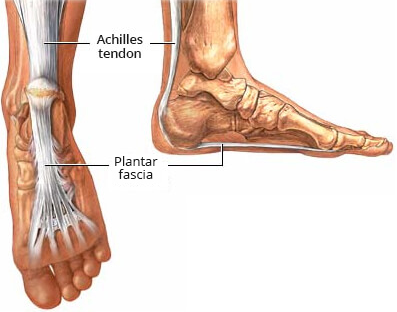
© By Ryxi10, via Wikimedia Commons
By Ryxi10, via Wikimedia Commons
The plantar fascia is a sturdy structure but the degree of stress that it takes makes it susceptible to injury. A force equal to almost three times the body's weight passes through the foot with each step. On running, this typically happens about 90 times a minute.
Plantar fasciitis is thought to be a traction and overuse injury. Damage to the plantar fascia is usually in the form of micro-tears. Plantar fasciitis is a degenerative rather than an inflammatory process2 .
Damage tends to occur near the heel, where stress on the fibres is greatest and where the fascia is the thinnest. The fascia broadens as it extends toward the toes.
Plantar fasciitis is often associated with calcaneal spurs. These are depositions of calcium where the fascia suffers most damage. Spurs are most commonly on the medial side at the origin of the fascia from the calcaneum. Spurs are the result of the process of plantar fasciitis and not the cause of the pain.
Plantar fasciitis can present bilaterally.
Continue reading below
Epidemiology
Back to contentsPlantar fasciitis is common in runners but can also affect sedentary people3 .
Plantar fasciitis risk factors4
Intrinsic:
Pes planus.
Pes cavus.
Over-pronation.
Leg-length discrepancy.
Excessive lateral tibial torsion.
Excessive femoral anteversion.
Being overweight.
Gastrocnemius and soleus muscles tightness.
Achilles tendon tightness.
Gastrocnemius, soleus and intrinsic foot muscles weakness.
Ageing of the heel fat pad.
Atrophy of the heel fat pad.
Plantar fascia stiffness.
Extrinsic:
Overuse.
Mechanical stresses and micro-tearing.
Incorrect training: a too-fast increase in the distance, intensity, duration or frequency of activities that involve repetitive impact loading of the feet.
Inadequate or inappropriate footwear.
History
Back to contentsThe principal complaint is heel/plantar pain. Most often this is 1 or 2 cm distal to the medial calcaneal tuberosity.
Ask about the onset of the symptoms and any precipitating, aggravating or relieving factors. What brings it on? What makes it worse?
Plantar fasciitis is often at its most severe during the first few steps after prolonged inactivity, such as sleeping or sitting.
Sitting with the foot elevated usually relieves the pain.
For those who are on their feet all day, pain is worst at the end of the day.
Walking barefoot, on toes, or up stairs can precipitate pain.
Ask about running or jogging and other sports.
Ask about footwear and when it was last replaced.
Ask about previous trauma to the foot.
Continue reading below
Examination
Back to contentsLook at the foot. Note any obvious deformities, skin changes, or congenital conditions. Look for pes planus or pes cavus.
There is often tightness of the Achilles tendon and ankle dorsiflexion may be limited.
Palpate the plantar surface over the medial calcaneal tuberosity and along the course of the plantar fascia, pressing quite hard. The reproduction of the pain is the most important physical sign to confirm the diagnosis.
Pain may be reproduced by asking the patient to stand on their toes or by passive dorsiflexion of the toes.
Palpate the back of the heel and ankle to exclude Achilles tendonitis.
Subcalcaneal bursitis produces a tender swelling underneath the calcaneum. It is not aggravated by dorsiflexing the toes. There is usually little or no swelling in plantar fasciitis.
Referred pain from an S1/S2 lesion should be excluded. Perform the straight leg raising test as for examination of the back. Check the ankle tendon reflex (S1) and calf strength. This is easily performed by asking the patient to walk on toes or stand on one leg and raise the heel off the floor. These tests should be normal.
Exclude tarsal tunnel syndrome: the posterior tibial nerve passes under the flexor retinaculum which runs between the medial malleolus and the calcaneum. Percuss over the nerve below and posterior to the medial malleolus. This can reproduce pain, numbness and burning on the medial side of the foot, ankle or calf if there is tarsal tunnel syndrome.
Press together the heads of the 2nd and 3rd metatarsals and then the 3rd and 4th. Reproduction of the pain suggests Morton's neuroma, with entrapment of the common digital nerve between the metatarsal heads.
A stress fracture of the calcaneum will cause tenderness over the calcaneum rather than anterior to it.
Differential diagnosis
Back to contentsSee also the separate Painful Foot and Foot Fractures and Dislocations articles.
Subcalcaneal bursitis.
S1 radiculopathy or referred pain.
Morton's neuroma.
Sever's disease (children and adolescents).
Stress fracture of calcaneum.
Very rarely:
Fibrosarcoma.
Metastases.
Foreign body.
Gout.
Investigations
Back to contentsThe diagnosis is essentially clinical. However, imaging may be required to exclude other possible underlying conditions5 .
Blood tests are not helpful.
Weighing and measuring the patient may reinforce that the BMI needs attention if obesity is a contributory factor.
X-ray: should not be performed as a matter of routine but may be indicated if you suspect another diagnosis. A lateral view may show soft tissue calcifications or a calcified spur on the anterior aspect of the calcaneus. X-ray may also help to exclude stress fracture, although stress fractures may not always be evident.
Ultrasound: this may show a thicker heel aponeurosis in plantar fasciitis6 .
Bone scans and MRI: these have also been used in diagnosis.
Plantar fasciitis treatment and management
Back to contentsThere is no one treatment with very strong evidence of efficacy; however, there are several treatment options with moderate levels of evidence, including stretching, orthotics, shock-wave therapy and injections. Plantar fasciitis treatments should be offered in sequence, depending on the individual patient's circumstances and likelihood of response1 .
General advice
Resting of the foot as much as possible.
Loss of weight if obese.
Correction of pes planus if present.
Advice to run on a softer surface.
A laced sports shoe gives good support. Update shoes regularly.
If the patient is an athlete, discuss training schedules. Cardiovascular fitness may be built by a shift, even temporarily, to swimming, cycling, a step machine in a gym or other low-impact exercise.
Non-steroidal anti-inflammatory drugs and ice may be useful.
Patients should be counselled that with any conservative management plan they should not expect to note a significant improvement in symptoms before 6-8 weeks2 .
Physiotherapy and stretching exercises
Stretching exercises are often advised for the plantar fascia, calf muscles and the Achilles tendon. Again, hard evidence for their use is lacking7 . However, benefit has been shown in some studies8 . The patient may be taught to do these exercises independently.
Deep massage of the sole of the foot also stretches the plantar fascia.
A physiotherapist may also recommend ultrasound, laser treatment, or iontophoresis with dexamethasone to assist pain relief and reduce inflammation. Again, evidence for these treatments is limited.
Orthotics, splinting and casting
A heel and arch support may help. However, a review showed that even though there is some evidence to support the use of foot orthoses in the prevention of lower-limb overuse injuries, there is limited evidence for their use in the treatment9 . Another study showed that they had short-term but not long-term treatment benefits10 . A Cochrane review suggested that there was silver level evidence for their use11 . Various pads and shoe inserts can be bought to cushion and raise the heel and give good arch support. Inserts should be worn in both shoes, even if pain is only in one foot.
Night splints to keep the ankle dorsiflexed and the toes extended can help to stretch the plantar fascia and may induce faster healing.
Corticosteroid injection
The evidence for steroid injection shows that it may provide some short-term benefit for plantar fasciitis but the evidence for its effectiveness in the long term is lacking12 . Counsel the patient accordingly.
The technique
A posterior tibial nerve block before injection has been suggested to reduce pain of the injection.
Ultrasound guidance has been used to facilitate accurate injection13 14 .
Plantar fascia rupture may also be a complication of steroid injection.
Use a maximum of three injections in six months.
Other modalities
Extracorporeal shock-wave therapy: a meta-analysis has shown this to be a safe and effective treatment which may be preferable to steroid injection15 . However, the National Institute for Health and Care Excellence (NICE) states that, although the evidence on extracorporeal shock-wave therapy for refractory plantar fasciitis raises no major safety concerns, current evidence on its efficacy is inconsistent16 .
Botulinum toxin A injections: may produce some benefit in the short term17 .
Autologous blood injection: the idea is that growth factors promote healing of the plantar fascia by stimulating fibroblast activity and vascular growth. There is currently a lack of long-term evidence for this technique18 . In one study it was shown to be effective in lowering pain and tenderness in chronic plantar fasciitis but corticosteroid injections were found to be superior in terms of speed and probably extent of improvement19 .
Radiotherapy has been shown to provide effective pain relief20 .
Surgery: endoscopic fasciotomy may be required in patients who continue to have pain that limits activity and function despite exhausting non-operative treatment options3 .
Plantar fasciitis prognosis
Back to contentsPain may be long-standing and can last for some years. However, plantar fasciitis generally resolves over time and with minimally invasive management1 .
80% show spontaneous response within 12 months.
Plantar fasciitis prevention
Back to contentsRegularly changing footwear used for running and walking.
Wearing shoes with good cushioning in the heels and good arch support.
Losing weight if overweight.
Avoiding exercising on a hard surface.
Regular stretching exercises for the plantar fascia and Achilles tendon.
Further reading and references
- Buchanan BK, Kushner D; Plantar Fasciitis. StatPearls, July 2021.
- Orchard J; Plantar fasciitis. BMJ. 2012 Oct 10;345:e6603. doi: 10.1136/bmj.e6603.
- Schwartz EN, Su J; Plantar fasciitis: a concise review. Perm J. 2014 Winter;18(1):e105-7. doi: 10.7812/TPP/13-113.
- Trojian T, Tucker AK; Plantar Fasciitis. Am Fam Physician. 2019 Jun 15;99(12):744-750.
- Petraglia F, Ramazzina I, Costantino C; Plantar fasciitis in athletes: diagnostic and treatment strategies. A systematic review. Muscles Ligaments Tendons J. 2017 May 10;7(1):107-118. doi: 10.11138/mltj/2017.7.1.107. eCollection 2017 Jan-Mar.
- Thompson JV, Saini SS, Reb CW, et al; Diagnosis and management of plantar fasciitis. J Am Osteopath Assoc. 2014 Dec;114(12):900-6. doi: 10.7556/jaoa.2014.177.
- Cole C, Seto C, Gazewood J; Plantar fasciitis: evidence-based review of diagnosis and therapy. Am Fam Physician. 2005 Dec 1;72(11):2237-42.
- Radford JA, Landorf KB, Buchbinder R, et al; Effectiveness of calf muscle stretching for the short-term treatment of plantar heel pain: a randomised trial. BMC Musculoskelet Disord. 2007 Apr 19;8:36.
- Digiovanni BF, Nawoczenski DA, Malay DP, et al; Plantar fascia-specific stretching exercise improves outcomes in patients with chronic plantar fasciitis. A prospective clinical trial with two-year follow-up. J Bone Joint Surg Am. 2006 Aug;88(8):1775-81.
- Collins N, Bisset L, McPoil T, et al; Foot orthoses in lower limb overuse conditions: a systematic review and meta-analysis. Foot Ankle Int. 2007 Mar;28(3):396-412.
- Landorf KB, Keenan AM, Herbert RD; Effectiveness of foot orthoses to treat plantar fasciitis: a randomized trial. Arch Intern Med. 2006 Jun 26;166(12):1305-10.
- Hawke F, Burns J, Radford JA, et al; Custom-made foot orthoses for the treatment of foot pain. Cochrane Database Syst Rev. 2008 Jul 16;(3):CD006801.
- Porter MD, Shadbolt B; Intralesional corticosteroid injection versus extracorporeal shock wave therapy for plantar fasciopathy. Clin J Sport Med. 2005 May;15(3):119-24.
- Tsai WC, Wang CL, Tang FT, et al; Treatment of proximal plantar fasciitis with ultrasound-guided steroid injection. Arch Phys Med Rehabil. 2000 Oct;81(10):1416-21.
- Tsai WC, Hsu CC, Chen CP, et al; Plantar fasciitis treated with local steroid injection: comparison between sonographic and palpation guidance. J Clin Ultrasound. 2006 Jan;34(1):12-6.
- Ogden JA, Alvarez RG, Marlow M; Shockwave therapy for chronic proximal plantar fasciitis: a meta-analysis. Foot Ankle Int. 2002 Apr;23(4):301-8.
- Extracorporeal shockwave therapy for refractory plantar fasciitis; NICE Interventional Procedures Guidance, August 2009
- Babcock MS, Foster L, Pasquina P, et al; Treatment of pain attributed to plantar fasciitis with botulinum toxin a: a short-term, randomized, placebo-controlled, double-blind study. Am J Phys Med Rehabil. 2005 Sep;84(9):649-54.
- Autologous blood injection for plantar fasciopathy, NICE Interventional Procedure Guidance, January 2013
- Lee TG, Ahmad TS; Intralesional autologous blood injection compared to corticosteroid injection for treatment of chronic plantar fasciitis. A prospective, randomized, controlled trial. Foot Ankle Int. 2007 Sep;28(9):984-90.
- Niewald M, Seegenschmiedt MH, Micke O, et al; Randomized, multicenter trial on the effect of radiation therapy on plantar fasciitis (painful heel spur) comparing a standard dose with a very low dose: mature results after 12 months' follow-up. Int J Radiat Oncol Biol Phys. 2012 Nov 15;84(4):e455-62. doi: 10.1016/j.ijrobp.2012.06.022. Epub 2012 Jul 25.
Continue reading below
Article history
The information on this page is written and peer reviewed by qualified clinicians.
Next review due: 17 Jan 2027
18 Jan 2022 | Latest version

Ask, share, connect.
Browse discussions, ask questions, and share experiences across hundreds of health topics.

Feeling unwell?
Assess your symptoms online for free