How PCOS affects your mental health
Peer reviewed by Dr Sarah Jarvis MBE, FRCGPAuthored by Lydia SmithOriginally published 17 Dec 2017
Meets Patient’s editorial guidelines
- DownloadDownload
- Share
- Language
- Discussion
Polycystic ovary syndrome (PCOS) is one of the most common hormone disorders in the UK, affecting at least one in ten women. Yet despite this, we still don't know exactly what causes the condition, and its potentially debilitating symptoms.
Women can experience distressing symptoms, including reduced fertility, excessive facial or body hair, weight gain, hair loss and acne. And now, research into PCOS has brought to light another devastating effect: women with the condition may be more likely to suffer from mental health problems.
In this article:
Continue reading below
What is PCOS?
What is PCOS?
PCOS affects the way the ovaries work and is characterised by irregular periods, excess androgens - a high level of 'male hormones' in the body - and polycystic ovaries, where the ovaries become enlarged and contain lots of fluid-filled sacs which surround the eggs.
When researchers at the University of Cardiff assessed the mental health history of more than 17,000 women diagnosed with the condition, the results showed those with PCOS were more likely to be diagnosed with depression, anxiety and bipolar disorder.
We don't know what causes the condition, which can run in families and is related to abnormal hormone levels - including high levels of insulin - but can affect any woman. And we don't know exactly why PCOS and mental health problems are linked - whether it is down to hormonal imbalances or other factors.
It's even more complicated because symptoms such as difficulty getting pregnant - not just the condition itself - can severely impact mental well-being too. Other issues associated with PCOS, such as excess hair growth and acne, can also lead to low self-esteem.
It is also possible for mental health problems to stem from a combination of both PCOS itself and the symptoms associated with it.
"I was told it would be almost impossible for me to conceive"
Sarah*, who is in her late 20s and did not want to be identified, was diagnosed with PCOS in her final year of university.
"I'd had really irregular periods ever since I'd started menstruating and it had got to the point where I was either having three periods a month, or none for five months," she says. "One of the things that has stayed with me since the diagnosis is how I was told it would be almost impossible for me to conceive naturally."
This wasn't something Sarah thought about until three years later, when she experienced a miscarriage. "All of a sudden, it dawned on me that that may have been my one chance of being a mother and the impact of my PCOS on that hit home."
Two years afterwards, one of Sarah's family members had a baby. "I was delighted at the news when the little one arrived, and immediately went out buying all sorts of toys and gifts to send home. But that evening it hit me. In what became the beginnings of a severe mental breakdown, I was suddenly overcome by the fact that I would probably never experience that for myself."
"I do believe my PCOS diagnosis really played a role in triggering how I reacted to my relatives' baby," she says. "The prospect of never having a child myself was never ever addressed by my GP when I was diagnosed. I got an: 'Oh, yeah, and you might find it hard to have children.' But that was all."
"There was certainly no groundwork put in at all as to how the condition might have affected me in the future."
Continue reading below
More research needed
According to Aled Rees, one of authors of the Cardiff University study, there are a number of reasons why women with PCOS might be prone to mental illness - but further work is necessary to understand the exact mechanisms involved.
"The effect of PCOS on mental health is under-appreciated. Our work shows that screening for mental health disorders should be considered during clinical assessments," he says, adding more work is needed to find out whether all women with PCOS are exposed to mental health risks.
A 2014 study carried out by the Columbia University School of Nursing found irregular menstrual cycles to be the symptom of PCOS most strongly associated with psychiatric problems. The trial was small - involving the evaluation of 126 women with the condition - but it also found body hair and menstrual problems were linked to anxiety.
Not all women with PCOS experience mental health problems, of course, but dealing with aspects of the condition, such as weight gain and acne, can be extremely distressing - particularly when society has a one-dimensional illustration of beauty as being slim and hairless.
Where to seek support
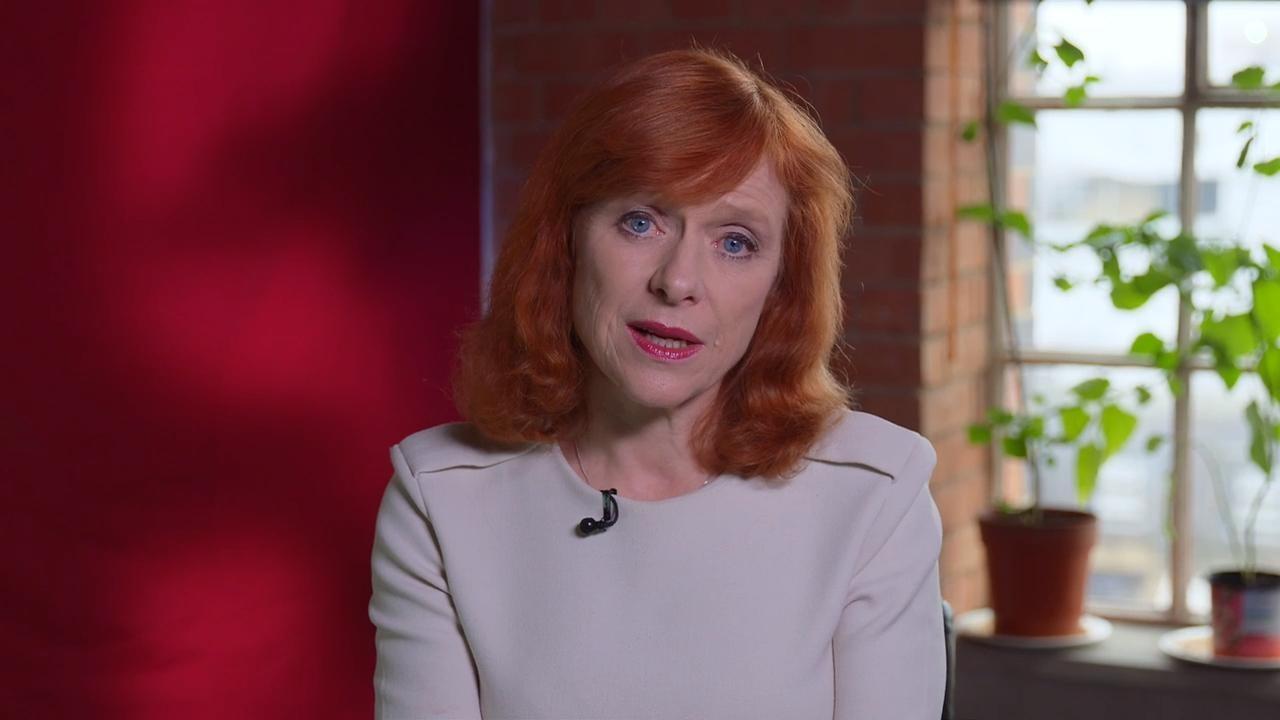
Professor Adam Balen, spokesperson for the Royal College of Obstetricians and Gynaecologists and chair of the British Fertility Society, says PCOS is a multifaceted condition which impacts many aspects of health and well-being.
"PCOS may have significant impacts on quality of life and may be associated with a higher risk of mood disorders," he says.
"It is important that healthcare professionals are aware of the full range of signs of symptoms of PCOS and ensure that appropriate attention is given both to their management and their impact on an individual's mental health."
Although there is no cure, symptoms can be managed through medical treatment and lifestyle changes such as losing weight, exercising regularly and eating a balanced diet.
Most women with PCOS are able to get pregnant, Balen says, adding it is key to seek advice from a GP to refer you to a fertility specialist.
Patient picks for PCOS

Hormones
What's the link between PCOS and diabetes?
Polycystic ovary syndrome (PCOS) is an incurable endocrine condition affecting up to one in ten women in the UK. It's most commonly associated with hormonal symptoms, such as acne, excess hair growth, weight gain, irregular periods, and reduced fertility. However, it is also associated with seemingly unrelated long-term health risks, like type 2 diabetes and cardiovascular disease. In fact, women with PCOS are as much as 40% more likely to develop type 2 diabetes than women without the condition - so what exactly is the link between PCOS and diabetes?
by Sarah Graham
Hormones
Video: How much does PCOS affect fertility?
With PCOS leading to so many subsequent problems, it's no wonder that many women have a lot of questions about the condition. Our experts have the answers to some of them.
by Amberley Davis
Continue reading below
Article history
The information on this page is peer reviewed by qualified clinicians.
17 Dec 2017 | Originally published
Authored by:
Lydia SmithPeer reviewed by
Dr Sarah Jarvis MBE, FRCGP

Ask, share, connect.
Browse discussions, ask questions, and share experiences across hundreds of health topics.

Feeling unwell?
Assess your symptoms online for free
Sign up to the Patient newsletter
Your weekly dose of clear, trustworthy health advice - written to help you feel informed, confident and in control.
By subscribing you accept our Privacy Policy. You can unsubscribe at any time. We never sell your data.