Arthritis
Peer reviewed by Dr Colin Tidy, MRCGPLast updated by Dr Toni Hazell, MRCGPLast updated 22 Jan 2023
Meets Patient’s editorial guidelines
- DownloadDownload
- Share
- Language
- Discussion
Arthritis means inflammation in a joint (like your knee, hip, elbow or fingers). It is a common problem and generally affects older people, although there are some rare conditions that cause arthritis in children and teenagers. There are lots of types of arthritis. Some give you short-term aches in the joints and then resolve completely, others can cause long-term problems and permanently affect how your joints move.
This leaflet will explain a bit about how joints work and then go through the main causes of arthritis in easy-to-read language.
In this article:
Continue reading below
What is arthritis?
Arthritis means inflammation of joints. Arthritis is very common. There are many causes of arthritis. Children and adults of all ages can be affected by arthritis, although the most common type is osteoarthritis and that affects older people. It is also more common in women than it is in men. See the separate leaflet called Osteoarthritis for more details.
Arthritis may affect just one joint, a few joints or many joints. Each cause of arthritis tends to have a typical pattern in terms of which joints are affected and the age of people most likely to be affected.
Understanding joints
Normal joint
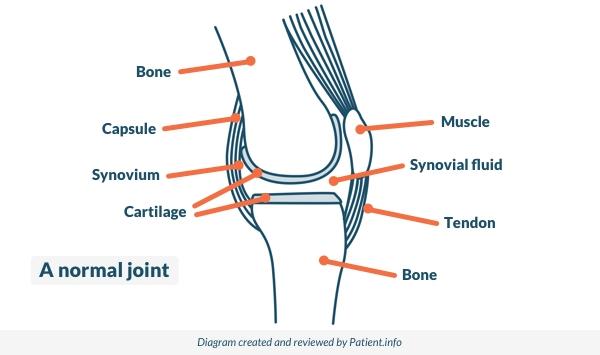
A joint is situated where two bones meet. Joints allow movement and flexibility of various parts of the body. The movement of the bones is caused by muscles which pull on tendons that are attached to bone. Cartilage covers the end of bones. Between the cartilage of two bones that form a joint there is a small amount of thick fluid called synovial fluid. This lubricates the joint, which allows smooth movement between the bones.
The synovium is the connective tissue that surrounds a joint. Synovial fluid is made by cells of the synovium. The outer part of the synovium is called the capsule. This is tough, gives the joint stability, and stops the bones from moving out of joint. Surrounding ligaments and muscles also help to give support and stability to joints.
What causes arthritis?
The two most common types of arthritis are osteoarthritis and rheumatoid arthritis. However, there are many different causes of arthritis.
The following list includes some of the common conditions that mainly affect joints. For further information, each condition has a separate leaflet.
Rheumatoid arthritis
Rheumatoid arthritis (RA) causes inflammation, pain, and swelling of joints. Persistent inflammation over time can damage affected joints. The severity can vary from mild to severe. The earlier treatment is started, the less joint damage is likely to occur.
Osteoarthritis
Osteoarthritis (OA) causes pain and stiffness in joints. Symptoms may be helped by exercises, some physical devices and treatments, and losing weight if you are overweight. It can be caused or worsened by trauma, in which case it may be known as post-traumatic arthritis.
Septic arthritis
Septic arthritis is an infection in a joint. Symptoms of this arthritis include pain and tenderness over a joint, pain on moving the joint, and feeling unwell. It is an uncommon infection but very serious. Emergency treatment in hospital is needed.
Ankylosing spondylitis
Ankylosing spondylitis is a form of arthritis. It mainly affects the lower back. Other joints and other parts of the body are sometimes affected. Treatment includes regular exercise and anti-inflammatory medicines. The severity of ankylosing spondylitis varies from mild to severe. An eye complication called uveitis can be serious but can be treated successfully if treatment is given promptly.
Gout
Gout causes attacks of pain and swelling when uric acid in the body crystalises in one or more joints. An anti-inflammatory painkiller usually eases an attack quickly. Lifestyle factors may reduce the risk of having gout attacks. These include losing weight (if overweight), eating a healthy diet, and not drinking much alcohol or sugar-sweetened soft drinks.
Calcium pyrophosphate deposition
Calcium pyrophosphate is a substance produced in the cartilages of the joints. It can become deposited as crystals on joint tissues. This is called calcium pyrophosphate deposition (CPPD). CPPD can cause a number of problems of which the most well known is pseudogout. This is almost identical to gout, causing attacks of pain and swelling in one or more joints. Some people get damage to the joint, causing a type of long-term arthritis. CPPD may cause no symptoms and is sometimes picked up on an X-ray done for an unrelated condition. Unlike gout, there is no special therapy for pseudogout.
Psoriatic arthritis
Psoriatic arthritis causes inflammation, pain, and swelling of joints in some people who have psoriasis (a skin condition). Other parts of the body may also be affected. For example, inflammation may also affect tendons and ligaments. The severity can vary from mild to severe. In some cases, affected joints become damaged which can cause disability.
Reactive arthritis
Reactive arthritis means that you develop inflammation in joints after you have had an infection in some other part of the body. Other symptoms usually develop in addition to the arthritis. Symptoms commonly last 3-6 months. In some cases the arthritis persists long-term. There is a rare 'triad' syndrome where arthritis, urethritis and conjunctivitis occur at the same time.
Juvenile idiopathic arthritis
Juvenile idiopathic arthritis (JIA) is an unusual condition in which joint inflammation occurs in children under the age of 16 years. It lasts for at least six weeks. Arthritis causes inflammation, pain and swelling of the affected joints. The severity can vary from mild to severe. The earlier the treatment is started, the less joint damage is likely to occur.
Continue reading below
Conditions similar to arthritis
There are some medical problems which don't affect the joints predominantly, but can cause joint problems as they progress. Examples include:
Systemic lupus erythematosus
Systemic lupus erythematosus (SLE) can cause various symptoms, the most common being joint pain and stiffness, skin rashes and tiredness. Problems with kidneys and other organs can occur in severe cases.
Gut (bowel) conditions
Some gut conditions, especially inflammatory bowel diseases such as Crohn's disease and ulcerative colitis, may cause arthritis.
Cervical spondylosis
Cervical spondylosis is a 'wear and tear' of the bones (vertebrae) and discs in the neck. It is a normal part of ageing and does not cause symptoms in many people. However, it is sometimes a cause of neck pain. Symptoms tend to come and go. In severe cases, the degeneration may cause irritation or pressure on the spinal nerve roots or spinal cord. This can cause arm or leg symptoms.
Polymyalgia rheumatica
Polymyalgia rheumatica (PMR) causes pain, stiffness and tenderness in large muscles, typically around the shoulders, upper arms and hips. The cause is not known. Some people with PMR develop a related condition called giant cell arteritis (GCA) which can be more serious and may threaten sight.
Fibromyalgia
Fibromyalgia causes pains and tenderness in many areas of the body, and tiredness. You may also have other symptoms.
Arthritis symptoms
The symptoms of arthritis vary depending on the type of arthritis and severity of the underlying cause. The symptoms include:
Joint pain, tenderness and stiffness.
Restricted movement of the joints.
Warmth and red skin over the affected joint.
Weakness and muscle wasting around the joint.
Continue reading below
How is arthritis diagnosed?
As with all medical conditions, the diagnosis is made by a combination of a history, examination and investigations. Some patients will need to be referred to a specialist. For inflammatory arthritis (eg, rheumatoid and psoriatic), all patients will be seen by a rheumatologist (joint specialist). For a non-inflammatory arthritis such as osteoarthritis, management is usually fully in primary care, by a GP and sometimes other healthcare professionals such as a physiotherapist, with referral being reserved for those who may need surgery.
Arthritis treatment
Although there is no cure for arthritis, there are treatments available for all forms. However, the treatment will depend on the cause of arthritis.
Treatments may include:
Medicines (such as NSAIDs, used by mouth or topically).
Weight loss, and diet changes.
Regular exercise, sometimes in a supervised session.
Heat and cold compresses.
Mobility assistance devices, such as canes or walkers.
Surgery.
Some causes of arthritis only need treatment for a short time. Other causes of arthritis may need lifelong treatment. If it affects the hip or the knee, treatment for osteoarthritis includes surgery to replace the entire joint. See the separate leaflets called Knee Replacement and Hip Replacement.
For elbow arthritis there is a technique known as elbow joint resurfacing, but this is not currently recommended by the National Institute for Health and Care Excellence (NICE) as there is not enough evidence for its safety and effectiveness. Some patients may be offered this procedure as part of a trial.
What is the outlook (prognosis) for arthritis?
Some types of arthritis are short-lived and don't leave you with any problems.
Examples are reactive arthritis, which usually goes away by itself and juvenile arthritis which may sometimes clear up without any long-term problems. Other types come and go, like gout.
Rheumatoid arthritis tends to stay with you for the long term, but can be controlled with medication.
Osteoarthritis can usually be controlled with a combination of painkillers, physiotherapy, and surgery, and by reducing pressure on the joint by avoiding being overweight.4
Although there is no sure way to prevent arthritis, our article on the topic can help you look after your joint health, reduce risk factors, and alleviate symptoms.
Patient picks for Arthritis

Bones, joints and muscles
Reactive arthritis
Reactive arthritis is a type of arthritis in which you develop inflammation in joints after you have had an infection in some other part of the body. For example, after a bad bout of diarrhoea you might develop a sore knee a couple of weeks later. Symptoms commonly last between a few weeks and a few months. Anti-inflammatory medicines usually ease the pain. Other treatments are sometimes needed. This is an unusual condition that would usually be managed by a specialist.
by Dr Rosalyn Adleman, MRCGP

Bones, joints and muscles
Osteoarthritis
Osteoarthritis is a degenerative joint disease that causes pain and stiffness in joints. Symptoms may be helped by exercises, some physical devices and treatments and by losing weight if you are overweight. Anti-inflammatory painkillers and other medicines are sometimes advised. Joint replacement surgery is an option for severe cases.
by Dr Doug McKechnie, MRCGP
Further reading and references
- Rheumatoid arthritis in adults: management; NICE Guideline (July 2018 - last updated October 2020)
- Versus Arthritis
- Lateral elbow resurfacing for arthritis; NICE Interventional procedures guidance, September 2021
- Osteoarthritis in over 16s: diagnosis and management; NICE guideline (October 2022)
- Gout; NICE CKS, June 2023 (UK access only)
Continue reading below
Article history
The information on this page is written and peer reviewed by qualified clinicians.
Next review due: 21 Jan 2028
22 Jan 2023 | Latest version
11 Mar 2015 | Originally published
Authored by:
Dr Colin Tidy, MRCGP

Ask, share, connect.
Browse discussions, ask questions, and share experiences across hundreds of health topics.

Feeling unwell?
Assess your symptoms online for free
Sign up to the Patient newsletter
Your weekly dose of clear, trustworthy health advice - written to help you feel informed, confident and in control.
By subscribing you accept our Privacy Policy. You can unsubscribe at any time. We never sell your data.