Spina bifida
Peer reviewed by Dr Helen Huins, MRCGPLast updated by Dr Colin Tidy, MRCGPLast updated 15 Jul 2017
Meets Patient’s editorial guidelines
- DownloadDownload
- Share
- Language
- Discussion
- Audio Version
This page has been archived.
It has not been reviewed recently and is not up to date. External links and references may no longer work.
Spina bifida is caused by an abnormal development of the spine and spinal cord which leaves a gap in the spine. Spina bifida can vary from causing no problems to causing severe physical disability.
Spina bifida is usually diagnosed at the time of the routine pregnancy ultrasound scan. Treatment of spina bifida may not be needed or may include operations, physiotherapy and walking aids.
The best way to prevent a baby from having spina bifida is to take folic acid supplements before pregnancy and during the first 12 weeks of pregnancy.
In this article:
Video picks for Pregnancy complications
Continue reading below
What is spina bifida?
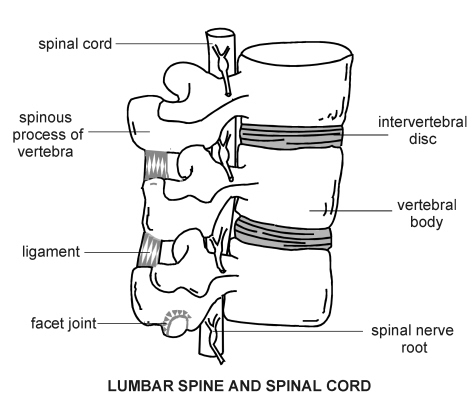
Spina bifida is an abnormal development of the spine and spinal cord which leaves a gap in the spine. The spinal cord connects all parts of the body to the brain.
Lumbar spine and spinal cord
What causes spina bifida?
Back to contentsDuring the first month of pregnancy, a developing baby (embryo) forms special tissue called the neural plate. Early in development, the edges of the neural plate begin to curl up towards each other. This forms the neural tube, which closes to form the brain and spinal cord of the developing baby.
In cases of spina bifida, the bone that surrounds and protects the nerves (the spinal column) does not fully close. The exact cause for this happening is not known.
Continue reading below
Who is at increased risk of having a baby with spina bifida?
Back to contentsThe most important known risk of a baby having spina bifida is the mother having a lack of folic acid before and at the very start of pregnancy. Folic acid is a vitamin that occurs naturally in some foods, such as broccoli, peas and brown rice. It is also added to foods, such as some breakfast cereals. Taking a folic acid supplement before you become pregnant and while you are pregnant can prevent up to 7 out of 10 cases of spina bifida. It is not known how folic acid helps prevent spina bifida.
Having a family member with spina bifida, increases your chances of having a baby with spina bifida. Your risk of having a baby with spina bifida is also increased if you already have a child with spina bifida.
Some types of medicine have been linked to an increased risk of spina bifida or other birth defects. These medicines include sodium valproate, carbamazepine and lamotrigine. These medicines are used to treat epilepsy and some other disorders, such as bipolar disorder.
If you are taking a medicine that increases the risk of spina bifida and you are planning a pregnancy, speak to your GP. Other medicines may be available. Taking extra folic acid supplements may also help reduce the risk. Never stop taking a prescribed medicine without talking to your GP first.
If you have diabetes the risk of giving birth to a child with spina bifida is increased. Women who are overweight are also at increased risk of giving birth to a child with spina bifida. The more overweight you are, the higher the risk.
What are the different types of spina bifida?
Back to contentsThere are two main types of spina bifida:
Spina bifida occulta - there is a bone defect in the spinal cord but there is no nerve (spinal cord) abnormality.
Spina bifida cystica - there is a defect of the spinal cord and the lining of the spinal cord is pushed out through the defect. Spinal cord tissue may also be pushed out through the defect.
Spina bifida occulta
Spina bifida occulta occurs in about 1 in every 10 people and rarely causes any symptoms or problems. Spina bifida occulta is the least serious type of spina bifida. The opening in the spine is very small, with one or more of the bones of the spine (vertebrae) not properly formed. The opening in the spine is covered with skin, so the gap is not visible from the outside.
Spina bifida occulta does not usually cause any symptoms and most people are unaware they have the condition. In such cases, no treatment is needed. In other cases, there may be some symptoms, such as bladder and bowel problems, or an abnormal curve of the spine (scoliosis).
Spina bifida cystica
Spina bifida cystica occurs when the lining (membranes) of the spinal cord and sometimes the spinal cord push out through the defect in the spine. The two main types of spina bifida cystica are called meningocele and myelomeningocele:
Meningocele
Spina bifida meningocele is the rarest type of spina bifida. The protective membranes (the meninges) surrounding the spinal cord are pushed out between openings in the vertebrae. The meningocele is sometimes covered by a layer of skin. There are no spinal cord nerves in the protruding sac. The membranes can usually be removed by surgery.
The symptoms can be very variable. Sometimes there are few or no symptoms or problems. Others may have severe weakness of the legs and also bladder and bowel problems.
Myelomeningocele
This is the most serious type of spina bifida. About one pregnancy in every 1,000 pregnancies is affected in the UK. The spinal column remains open along the bones making up the spine. The membranes and spinal cord push out to make a sac on the baby's back. This sometimes leaves the nervous system at risk of infections that may be life-threatening.
In most cases of myelomeningocele, surgery can be carried out to close the defect. However, damage to the nervous system will usually already have taken place. The nerve damage can cause a range of symptoms, including weakness (paralysis) of the legs and loss of feeling in the skin of the legs. There may also be problems with passing wee (urine) and poo (faeces, stools or motions).
Continue reading below
What are the signs of spina bifida?
Back to contentsSpina bifida occulta does not cause any defect of the skin over the spine and may go unnoticed. Spina bifida occulta may be associated with changes in the overlying skin. For example, there may be a change in colour of the skin, a hairy patch, a birthmark or a dimple in the skin.
Spina bifida cystica causes a swelling over the defect in the spine and this may contain nerve (spinal cord) tissue. Meningocele and myelomeningocele usually involve a fluid-filled sac, which can be seen on the back. In meningocele, the sac may be covered by a thin layer of skin. In most cases of myelomeningocele, there is no layer of skin covering the sac and an area of abnormal spinal cord tissue can be seen.
How is spina bifida diagnosed?
Back to contentsIn most cases, spina bifida is diagnosed before birth. Some mild cases may go unnoticed until after birth. Very mild forms (spinal bifida occulta), in which there are no symptoms, may never be detected.
Before birth
The most common screening methods used to look for spina bifida during pregnancy are the blood test for alpha-fetoprotein and an ultrasound scan, which are routinely performed at 16-18 weeks of pregnancy. See the separate leaflet called Pregnancy - Screening Tests for more details.
After birth
Mild cases of spina bifida (occulta) may be detected after birth by plain film X-ray examination. Babies with the more severe forms of spina bifida often have muscle weakness in their feet, hips and legs that result in deformities that may be present at birth. Further X-rays of hips, legs and feet may be required.
Magnetic resonance imaging (MRI) or a computerised tomography (CT) scan may be used to get a clearer view of the spinal cord and vertebrae. If hydrocephalus (see below) is suspected, the doctor may request a CT scan of your baby's head to look for signs of extra fluid inside the brain.
Further tests may also be needed. These tests will depend on any associated problems but may include an ultrasound scan of the kidneys and bladder.
What are the complications of spina bifida?
Back to contentsComplications of spina bifida can vary from no problems to severe physical disabilities. Most people with spina bifida are of normal intelligence. The problems caused by spina bifida depend on the size and position of the defect in the spine, whether it is covered, and which spinal nerves are involved. All nerves located below the defect will be affected to some extent. Therefore, the higher the defect occurs on the back, the greater the amount of nerve damage and loss of muscle power and sensation.
Hydrocephalus
Most babies with myelomeningocele will also develop an excess of the fluid surrounding the brain - this fluid is called cerebrospinal fluid (CSF). This causes an increased pressure in the brain (hydrocephalus). Hydrocephalus needs to be treated urgently, as the pressure on the brain can cause brain damage. Hydrocephalus is often treated by an operation to insert a hollow tube (shunt) from the brain to the tummy (abdomen) to drain the excess fluid.
Chiari II malformation
Myelomeningocele can also be associated with a serious condition called a Chiari malformation. This condition involves part of the brain being pushed down and out of the skull and into the spinal canal in the neck.
This can lead to squashing (compression) of the spinal cord. This may cause a variety of symptoms including difficulties with feeding, swallowing, breathing problems and arm weakness. A Chiari malformation may also cause blockage of the CSF (hydrocephalus).
Meningitis
Some newborn babies with myelomeningocele may develop meningitis, an infection in the lining of the brain and spinal cord (meninges). Meningitis may cause brain injury and can be life-threatening.
Other complications
Spina bifida may be associated with abnormal curvature (scoliosis) of the spine. A child with spina bifida may also have leg and foot abnormalities - for example, abnormal hips, unequal leg length or club foot.
There may be associated bladder problems - for example, problems passing urine or loss of control passing urine (urinary incontinence). Bowel problems may also occur - for example, passing hard poo (constipation), frequent watery loose poo (diarrhoea), or loss of control of passing poo (incontinence).
Children with both myelomeningocele and hydrocephalus may have learning disabilities, including difficulty paying attention, problems with language and reading, and trouble learning maths. However, most people with spina bifida have normal intelligence.
Some children with myelomeningocele develop a condition called progressive tethering (tethered cord syndrome). The spinal cord becomes stuck to the overlying membranes and bones (vertebrae). This causes the spinal cord to become stretched as your child grows. This can cause loss of muscle power in the legs. It can also cause bowel and bladder problems. Early surgery on a tethered spinal cord may prevent further damage to the spinal cord.
How can spina bifida be treated?
Back to contentsA number of different treatments can be used to treat symptoms or conditions associated with spina bifida.
There is no cure for spina bifida. The nerve tissue that is damaged cannot be repaired. Treatment depends on the type and severity of spina bifida. Generally, children with the mildest form of spina bifida need no treatment, although some may require surgery as they grow.
A baby born with spina bifida cystica will usually have surgery to close the defect and reduce the risk of infection or further injury within the first few days of life. It has been shown that operating on your baby before birth may also be effective.
Some children will need further operations to manage problems with the feet, hips, or spine. Children with increased pressure in the brain (hydrocephalus) will need further operations to replace the shunt used to reduce the brain pressure.
Therapies such as physiotherapy, occupational therapy and speech therapy may be needed. Equipment such as walking aids and a wheelchair may be needed. Computer software may be used to help with schoolwork and writing
Treatment for bladder and bowel problems usually begins soon after birth. The treatments will vary depending on the problems being caused.
What is the outcome?
Back to contentsOutcome (prognosis) will depend on the type of spina bifida and any permanent damage to the spinal cord or brain. Some people with spina bifida will have severe physical disability and learning difficulties.
However, many children with spina bifida can lead active lives and survive well into adulthood. Most children with spina bifida have normal intelligence. Many adults with spina bifida are able to lead independent and fulfilling lives.
How can spina bifida be prevented?
Back to contentsThe best way to prevent your baby having spina bifida is to take folic acid supplements both before and during pregnancy. It is recommended that all women who might get pregnant should take a daily supplement of folic acid.
Folic acid should be taken for the first 12 weeks of pregnancy because this is when your baby's spine is developing. If you have an increased risk of having a child with spina bifida you may need a higher dose of folic acid. For example, you are at increased risk if you have diabetes or you are taking medicines to treat epilepsy.
It is also very important to eat food that is rich in folic acid. These foods include dark green vegetables, egg yolks and some fruits. Many foods have folic acid added - for example, some breakfast cereals, some breads, flours, pastas and brown rice.
Patient picks for Pregnancy complications
Pregnancy
Fetal anticonvulsant syndrome
Fetal anticonvulsant syndrome (FACS) - also known as fetal valproate syndrome and fetal hydantoin syndrome - is a group of malformations that can affect some babies if they are exposed to certain medicines known as antiepileptic drugs (AEDs) while in the womb. Most women with epilepsy will have a healthy child. Women with epilepsy who are pregnant and worried about their medication should not stop taking it without talking to their doctor. Stopping your medication makes you more likely to have seizures which can also be a risk to the baby.
by Dr Hayley Willacy, FRCGP

Pregnancy
Pre-eclampsia
Pre-eclampsia involves high blood pressure and protein in the urine. It can have no symptoms but some women may have headache, blurred vision, tummy pain and swollen ankles. The severity of pre-eclampsia is usually (but not always) related to your blood pressure level. It can be a serious condition but specialist care will help mother and baby stay safe.
by Dr Toni Hazell, MRCGP
Further reading and references
- Copp AJ, Stanier P, Greene ND; Neural tube defects: recent advances, unsolved questions, and controversies. Lancet Neurol. 2013 Aug;12(8):799-810. doi: 10.1016/S1474-4422(13)70110-8. Epub 2013 Jun 19.
- Adzick NS; Fetal surgery for spina bifida: past, present, future. Semin Pediatr Surg. 2013 Feb;22(1):10-7. doi: 10.1053/j.sempedsurg.2012.10.003.
- De-Regil LM, Pena-Rosas JP, Fernandez-Gaxiola AC, et al; Effects and safety of periconceptional oral folate supplementation for preventing birth defects. Cochrane Database Syst Rev. 2015 Dec 14;12:CD007950. doi: 10.1002/14651858.CD007950.pub3.
- Salih MA, Murshid WR, Seidahmed MZ; Classification, clinical features, and genetics of neural tube defects. Saudi Med J. 2014 Dec;35 Suppl 1:S5-S14.
- Salih MA, Murshid WR, Seidahmed MZ; Epidemiology, prenatal management, and prevention of neural tube defects. Saudi Med J. 2014 Dec;35 Suppl 1:S15-28.
- Copp AJ, Adzick NS, Chitty LS, et al; Spina bifida. Nat Rev Dis Primers. 2015 Apr 30;1:15007. doi: 10.1038/nrdp.2015.7.
Continue reading below
Article history
The information on this page is written and peer reviewed by qualified clinicians.
15 Jul 2017 | Latest version

Ask, share, connect.
Browse discussions, ask questions, and share experiences across hundreds of health topics.

Feeling unwell?
Assess your symptoms online for free
Sign up to the Patient newsletter
Your weekly dose of clear, trustworthy health advice - written to help you feel informed, confident and in control.
By subscribing you accept our Privacy Policy. You can unsubscribe at any time. We never sell your data.