Abdominal aortic aneurysm
Peer reviewed by Dr Colin Tidy, MRCGPLast updated by Dr Doug McKechnie, MRCGPLast updated 19 Sept 2023
Meets Patient’s editorial guidelines
- DownloadDownload
- Share
- Language
- Discussion
In this series:Aortic dissectionMarfan syndrome
The aorta is the main blood vessel in the abdomen, running down from your heart. It is normally about the diameter of a garden hose. In older people, particularly those who smoke, part of it can enlarge and balloon up.
This is called an abdominal aortic aneurysm (often abbreviated to AAA, pronounced 'triple-A').
This doesn't cause any symptoms and the person is usually unaware they have it, until it leaks or bursts. The medical term for this is rupture. If the aneurysm ruptures, it can be fatal.
In the UK there is a screening programme for men over the age of 65, to see if they have a triple-A. An operation to repair the aneurysm may be advised if it is larger than 5.5 cm, as above this size the risk of rupture increases significantly.
In this article:
Continue reading below
What is an abdominal aortic aneurysm?
An aneurysm is a swelling in a blood vessel. Aneurysms can occur in any artery, including the aorta. The aorta is the large blood vessel that carries blood away from the heart to the body. Most aortic aneurysms occur in the section of the aorta that passes through the lower abdomen. These are known as abdominal aortic aneurysms (AAAs - pronounced by doctors as 'triple-As').
The normal diameter of the aorta in the abdomen is about 2 cm, a bit like a garden hose. An abdominal aortic aneurysm is said to be present if a section of the aorta within the abdomen is 3 cm or more in diameter.
Abdominal aortic aneurysms vary in size. As a rule, once you develop one, it tends gradually to become larger over the years. The speed at which it becomes larger varies from person to person. However, on average, a triple-A tends to become larger by about 10% per year.
These pictures show the typical location of a triple-A: low down in the tummy below the level of the kidneys.
Abdominal aortic aneurysm
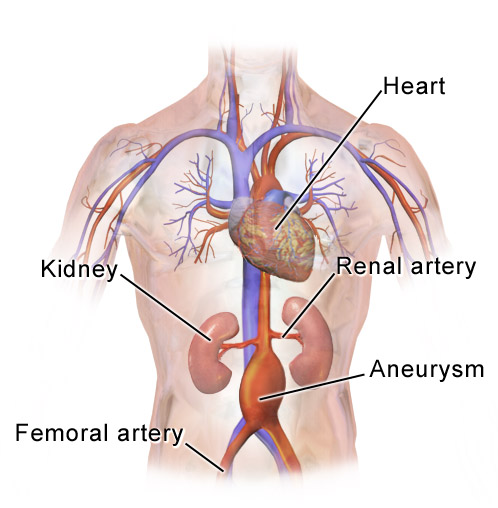
By BruceBlaus [CC VY-SA 4.0 (https://creativecommons.org/licenses/by-sa/4.0)], via Wikimedia Commons
Abdominal aortic aneurysm causes
Common causes
A triple-A occurs because of a weakening in the wall of the aorta. We don't know exactly what causes this weakening to happen. Things that increase the risk of a triple-A developing include:
Age. Triple-As are rare in people under the age of 60. It's likely that ageing is involved in the development of triple-As.
Smoking. Smoking greatly increases the risk of developing a triple-A. It's thought that chemicals in cigarette smoke cause proteins in the aortic wall to break down, making it weaker.
Stopping smoking reduces the risk of developing a triple A, and also slows down the rate at which they grow.
Gender. Triple-As are six times more common in men than in women.
Genetics. People who have a close family member (parent, sibling, or child) with a triple-A have a much higher risk of developing one themselves.
Having diabetes.
A process called atherosclerosis is thought to be important in triple-As. Atherosclerosis is when deposits of cholesterol, fat, calcium, and other chemicals build up in the wall of an artery, forming something called a plaque or atheroma. Sometimes, when this happens in the aorta, it seems to cause other processes to happen that eventually lead to weakening and swelling (aneurysm) of the aorta.
Atherosclerosis can affect arteries all throughout the body. When it affects the arteries supplying the heart, it can cause angina and heart attacks; if it affects the arteries supplying the brain, it can cause strokes; and if it affects the arteries supplying the leg muscles, it can cause peripheral vascular disease.
So, many of the risk factors for triple-As are risk factors for atherosclerosis, and for heart disease, strokes, and peripheral vascular disease. This also means that people with triple-As are likely to have atherosclerosis affecting other arteries, and are at a higher risk of developing heart disease and strokes (see below).
Rarer causes
Rare causes of triple-As include:
Genetic connective tissue disorders that affect the structure of blood vessels, such as Marfan's syndrome and classical Ehlers-Danlos syndrome.
These tend to cause aneurysms in other parts of the aorta, such as in the chest, but can cause triple-As as well.
People with these conditions might develop a triple-A at an unusually young age.
Infections, such as:
Continue reading below
How common are abdominal aortic aneurysms?
About 1 in 170 men over the age of 65 have an abdominal aortic aneurysm. The prevalence in women is much lower - about 1 in 600 - but the chance of rupture is significantly higher. It becomes more common with increasing age. However, most people with an abdominal aortic aneurysm are not aware that they have one (see below in the section on symptoms). A triple-A is rare in people under the age of 50.
Abdominal aortic aneurysm symptoms
Usually there are no symptoms and the person is entirely unaware they have an abdominal aortic aneurysm. At the time of diagnosis, 7 in 10 people with an abdominal aortic aneurysm will not have had any symptoms due to the aneurysm. The ballooning of the aneurysm does not cause any symptoms unless it becomes large enough to put pressure on nearby structures.
If symptoms do occur, they are likely to be:
Mild tummy (abdominal) or back pains.
There are many causes of mild abdominal and back pain. So, it may be difficult to diagnose at this stage, unless the aneurysm is large enough to be felt by a doctor when they examine the abdomen.
Sometimes, small blood clots form on the inside lining of an abdominal aortic aneurysm. These may break off and be carried down the aorta and block a smaller blood vessel further on. These blood clots are called emboli and can be dangerous. The symptoms vary depending on where the blood clot is, but might include:
Sudden, severe pain in one leg or foot.
Pale colour of the leg or foot.
Inability to move the leg or foot.
If the blood supply is completely blocked and not treated in time, affected parts of the leg or foot may die (gangrene).
The main complication from an abdominal aortic aneurysm is rupture (bursting). Symptoms of a burst aortic aneurysm include:
Sudden severe abdominal (tummy) and/or back pain.
Other symptoms caused by internal bleeding and dropping blood pressure, such as a collapse, loss of consciousness, or otherwise becoming extremely unwell.
A burst aortic aneurysm is a life-threatening emergency. Call 999 for emergency medical help if you, or someone you know, has symptoms of a burst aortic aneurysm.
Continue reading below
How is an abdominal aortic aneurysm diagnosed?
Abdominal aortic aneurysms can sometimes be felt when examining the abdomen (tummy). However, this isn't very reliable, as many of them are too small to feel.
Triple-As are usually diagnosed with:
Ultrasound scans. These use high-frequency sound waves (ultrasound) to measure the size of the aorta, and can quickly detect a triple-A. Ultrasound scans are the basis of the triple-A screening programme in the UK (see below).
A CT scan. This gives more information about the exact location and size of a triple-A, and also shows if other arteries coming off the aorta are affected. This is very important information for surgeons if they are planning an operation.
Because many people with triple-As have no symptoms, they are often diagnosed when someone has an ultrasound or CT scan for another reason.
Abdominal aortic aneurysm treatments
The only definitive treatment for the aneurysm itself is surgery.
Should everyone with an abdominal aortic aneurysm have surgery?
No. For many people with a triple-A, the risk of surgery outweighs the risk of the aneurysm bursting. Surgical repair of an abdominal aortic aneurysm is a major operation and carries risks. A small number of people will die during, or shortly after, the operation.
For small abdominal aortic aneurysms, the risk of death caused by surgery is higher than the risk of bursting. Therefore, surgery is usually not advised if you have a triple-A less than 5.5 cm wide. However, regular ultrasound scans are usually offered to monitor its size over time; if it becomes large enough, surgery may be offered.
Surgery is often recommended for people with an abdominal aortic aneurysm larger than 5.5 cm, or a smaller abdominal aortic aneurysm that is growing rapidly. For these larger aneurysms the risk of rupture is usually higher than the risk of surgery. However, if your general state of health is poor, or if you have certain other medical conditions, this may increase the risk if you have surgery. So, in some cases the decision to operate may be a difficult one.
Any decision about whether to have surgery should be made between you and the surgeon, who should provide information about the risks and benefits of an operation, and how it compares to the alternative of not having surgery.
If an abdominal aortic aneurysm ruptures, it is always fatal without emergency surgery. Emergency surgery can be life-saving. However, a ruptured aortic aneurysm is still very difficult to treat; many people do not survive long enough to reach the operating theatre, and, of those that do, about half of them die despite surgery.
What operations are performed?
There are two types of surgical operation to repair an abdominal aortic aneurysm:
Open repair, or 'traditional repair' The traditional operation is to cut out the bad piece of aorta and replace it with an artificial piece of artery (a graft). It's called an 'open' repair because it involves making an incision (cut) in the abdomen (tummy) to access the aorta and other organs. This is a major operation and, as mentioned, carries some risk. Some people die during this operation. It usually requires a month or two to recover. However, it is successful in most cases and the aneurysm is totally fixed. If the operation is successful, the long-term outlook is good. The graft usually works well for the rest of your life.
Endovascular repair (EVAR)
Endovascular repair (EVAR) is an alternative to open surgery. Instead of making a cut in the abdomen, a tube-shaped graft is passed up from inside one of the leg arteries into the area of the aneurysm. This graft is then passed across the widened aneurysm and fixed to the good aorta wall, using metal clips. EVAR is now more-commonly performed than open repair.
The advantage to this type of repair is that there is no tummy (abdominal) surgery. Recovery time is usually much shorter than with open surgery. There is also a lower chance of serious complications at the time of the operation. EVAR has been particularly useful for people with other medical conditions that mean an open repair would be too risky.
However, there is a higher chance of needing another operation later on, compared to an open repair; it's roughly twice as likely with EVAR. In addition, some types of abdominal aortic aneurysms are not suitable for treatment with EVAR; for example, aneurysms that affect the arteries going to the kidneys. Some centres offer 'complex EVAR' procedures for these, though, and this area might change in future.
Choosing between open repair and EVAR depends on lots of factors. Your surgeon should discuss the benefits and risks of all the options with you, to help you come to a shared decision.
Other treatments
People with an abdominal aortic aneurysm are likely to have atherosclerosis in other arteries, such as the heart (coronary) arteries and brain arteries. So, people with a triple-A are often at higher risk of heart disease and strokes.
In fact, most people who develop an abdominal aortic aneurysm do not die of the aneurysm but die from other vascular conditions, such as a heart attack or stroke.
Therefore, it's very important to reduce the risk of these happening. Ways to do this include:
Eat a healthy diet which includes keeping a low salt intake.
Exercise as much as you are able.
If you have high blood pressure, diabetes or a high cholesterol level, they should be well controlled on treatment.
You may be prescribed a statin drug to lower your cholesterol level and low-dose aspirin to help to prevent blood clots from forming.
See the separate leaflet called Cardiovascular Disease (Atheroma) for more details.
Screening for abdominal aortic aneurysm
In the UK, there is a national screening programme to detect abdominal aortic aneurysms in men. This is because many people with triple-As have no symptoms, and would otherwise go undiagnosed; research evidence shows that diagnosis and treatment can help to prevent complications from triple-As in future.
In England, Wales, Scotland, and Northern Ireland, men aged 65 are invited for a one-off ultrasound scan to check for an abdominal aortic aneurysm.
If an aneurysm is found, men may be offered surgery or observation, depending on the size of the aneurysm.
Screening for triple-As is currently only offered to men, as they are much more common in men than in women.
What is the chance of an abdominal aortic aneurysm rupturing?
The chance of bursting (rupture) is low if a triple-A is small. As a rule, the risk of rupture increases with increasing size. This is much like a balloon - the larger you blow it up, the greater the pressure and the greater the chance it will burst.
The diameter of a triple-A can be measured by an ultrasound scan. As a rule, for any given size, the risk of rupture is increased in smokers, women, those with high blood pressure and those with a family history of AAA.
Patient picks for Arteries
Heart health and blood vessels
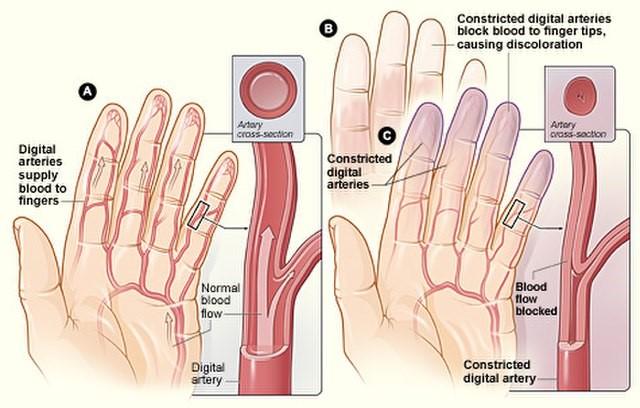
Raynaud's phenomenon
Raynaud's phenomenon (often just called Raynaud's), is a condition where the small blood vessels of the fingers become narrow (constrict). This happens most often when they are in a cool environment. Blood vessels to other extremities such as the toes, ears and nose may also be affected. It is named after Dr Maurice Raynaud, the man who first described it in 1862.
by Dr Hayley Willacy, FRCGP

Heart health and blood vessels
Coronary artery spasm
Coronary artery spasm is a temporary, sudden narrowing of one or more of the coronary arteries.
by Dr Hayley Willacy, FRCGP
Further reading and references
- Cosford PA, Leng GC; Screening for abdominal aortic aneurysm. Cochrane Database Syst Rev. 2007 Apr 18;(2):CD002945.
- Badger S, Bedenis R, Blair PH, et al; Endovascular treatment for ruptured abdominal aortic aneurysm. Cochrane Database Syst Rev. 2014 Jul 21;7:CD005261. doi: 10.1002/14651858.CD005261.pub3.
- Guidelines on the diagnosis and treatment of aortic diseases; European Society of Cardiology (2014)
- Abdominal aortic aneurysm: diagnosis and management; NICE Guidance (March 2020)
Continue reading below
Article history
The information on this page is written and peer reviewed by qualified clinicians.
Next review due: 17 Sept 2028
19 Sept 2023 | Latest version

Ask, share, connect.
Browse discussions, ask questions, and share experiences across hundreds of health topics.

Feeling unwell?
Assess your symptoms online for free
Sign up to the Patient newsletter
Your weekly dose of clear, trustworthy health advice - written to help you feel informed, confident and in control.
By subscribing you accept our Privacy Policy. You can unsubscribe at any time. We never sell your data.