Myeloma
Myelomatosis
Peer reviewed by Dr Rosalyn Adleman, MRCGPLast updated by Dr Colin Tidy, MRCGPLast updated 20 Mar 2023
Meets Patient’s editorial guidelines
- DownloadDownload
- Share
- Language
- Discussion
In this series:Hodgkin's lymphomaNon-Hodgkin's lymphomaStem cell transplantBone marrow biopsy and aspiration
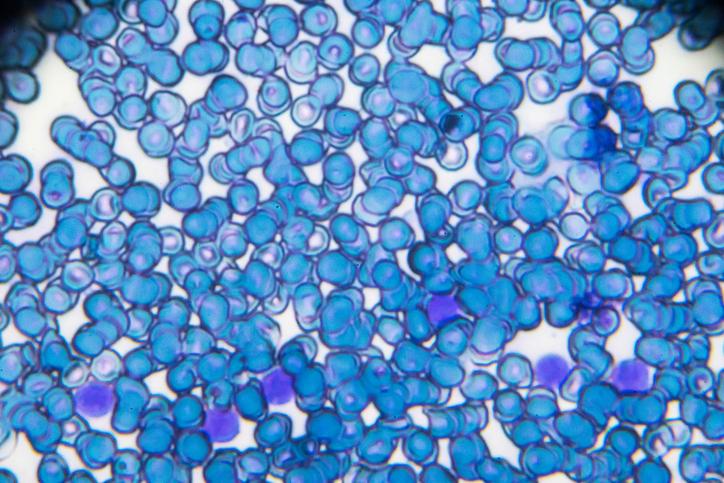
Myeloma is a cancer that affects cells, called plasma cells, in the bone marrow. Bone marrow is the spongy tissue at the centre of some bones that produces the body's blood cells. As the cancerous plasma cells fill the bone marrow, you are not able to make enough normal blood cells. This can lead to anaemia, bleeding problems and infections.
Other symptoms include bone pain, breaks (fractures) due to bone damage, and kidney damage. In many cases, treatment with chemotherapy and other treatments can control the disease, ease symptoms and prolong survival for a number of years.
In this article:
Continue reading below
What is myeloma?
Myeloma is a type of blood cancer. The cancer involves certain white blood cells called plasma cells. The cancerous plasma cells build up in the bone marrow. They also make a lot of one type of antibody. As a result, various symptoms develop. Myeloma is sometimes called multiple myeloma or myelomatosis. See the separate leaflet called Cancer for more general information about cancer.
What happens in myeloma?
Back to contentsAs with other cancers, what seems to happen is that the cancer starts with one abnormal cell. In the case of myeloma, one plasma cell at first becomes cancerous. This abnormal cell then multiplies to produce many identical abnormal plasma cells (a clone of cells). The cancerous plasma cells mainly collect in the bone marrow and continue to multiply without any control.
In the vast majority of cases of myeloma, the abnormal plasma cells make large quantities of one antibody. This single type of antibody is called a paraprotein (or sometimes called a monoclonal antibody, as it is an antibody which comes from a single clone of plasma cells).
There are several different types of antibody. (Antibodies are sometimes called immunoglobulins, or Ig for short.) These are called IgM, IgG, IgA, IgD and IgE. Myelomas are sub-classified by the type of antibody that they make. For example, IgG myeloma is the most common type.
Continue reading below
What causes myeloma?
Back to contentsPlasma cells develop from small white cells called B lymphocytes. It is thought that as B lymphocytes develop into plasma cells, mistakes occur in the process which copies genetic material, leading to the cell becoming cancerous.
The cancerous cell multiplies, leading to the development of myeloma, as described above. The reason why the genetic mistakes occur is not yet known but they do not appear to be handed down from one generation to the next. The condition is therefore not hereditary.
How common is myeloma and who is affected by it?
Back to contentsAbout 6,000 people are diagnosed with myeloma in the UK each year. Myeloma is more common in men than in women. It is more common in older people and very rare in people younger than 40.
Continue reading below
Myeloma symptoms
Back to contentsThere may be no symptoms at first in the early stages of the disease. Some people are diagnosed by chance because they have a blood test done for other reasons which may detect early myeloma. As the disease progresses, symptoms develop.
The symptoms and problems which develop are mainly due to the uncontrolled production of plasma cells in the bone marrow, and the excess amount of antibody (paraprotein) that the plasma cells make.
Bone damage and related problems
The increasing numbers of plasma cells in the bone marrow act like growing tumours (plasmacytomas) inside the bones. They also make a chemical that can damage bone. In time, small parts of bone are destroyed and are called lytic lesions. The term multiple myeloma is sometimes used which means there are lots of (multiple) areas in bones throughout the body which are affected.
The damage to bone can cause:
Bone pain. This is often the first symptom and can become severe. Any bone can be affected but the most common sites where pain first develops are the lower back, the pelvis and the ribs. The pain tends to be persistent and made worse by movement.
Fractures. Affected bones may easily break (fracture) following a mild injury or even no injury.
Compression of nerves coming out of the spinal cord. The compression usually happens because of fractures of the bones surrounding the spinal cord (the vertebrae). This can cause a variety of symptoms such as weakness in muscles of the legs, numbness of areas of the body or legs, bladder or bowel problems, and pain. If you have any of these symptoms you need to seek urgent medical attention.
Hypercalcaemia. This means a high level of calcium in the blood (due to the bone breaking down). This can:
Make you very thirsty.
Cause you to feel and be sick (have nausea and vomiting).
Develop a lack of fluid in the body (dehydration).
Have constipation.
Have kidney damage.
Bone marrow failure
Much of the bone marrow fills with abnormal plasma cells. Because of this, it is difficult for normal cells in the bone marrow to survive and to develop into normal mature blood cells. Therefore, problems which can develop include:
Anaemia. This occurs as the number of red blood cells goes down. This can cause tiredness, breathlessness and other symptoms. You may also look pale.
Blood clotting problems. This is due to low levels of platelets. This can cause easy bruising, bleeding from the gums, and other bleeding-related problems.
Serious infections. The abnormal plasma cells only make one type of antibody. This does not protect against infection. There is a reduced number of normal plasma cells and other types of white blood cells which usually combat infection. Therefore, serious infections are more likely to develop.
Kidney damage
The kidneys may be damaged by an increased calcium level in the bloodstream, and/or by the high level of the abnormal antibody (paraprotein).
Hyperviscosity
This means that the blood may become too thick due to a very high level of paraprotein. Symptoms of hyperviscosity occur in less than one in ten cases of myeloma and include problems such as bruising, nosebleeds, hazy vision, headaches, sleepiness and various other symptoms. If you develop these symptoms then you need to seek medical advice without delay.
Amyloidosis
This is an uncommon complication of myeloma. This is a condition where abnormal protein (amyloid) accumulates in various parts of the body. It can cause various symptoms.
Myeloma diagnosis
Back to contentsTests commonly done to confirm the diagnosis of myeloma include:
A blood or urine test to detect the paraprotein. Other blood tests are also usually done - for example, to see if you are anaemic, to test for the function of your kidneys and to check your calcium level.
A bone marrow sample. A needle is inserted into the pelvic bone, or occasionally the breastbone (sternum), then a small amount of marrow is removed. The sample is placed under the microscope to look for abnormal cells. The diagnosis is confirmed when large numbers of plasma cells are seen in the bone marrow sample. See the separate leaflet called Bone Marrow Biopsy and Aspiration.
X-rays of bones. The areas of damaged bones often show up as typical patterns on X-ray pictures. A magnetic resonance imaging (MRI) scan, computerised tomography (CT) scan or ultrasound scan may be done if X-ray tests do not give enough detailed information. Sometimes more specialised scans - for example, a positron emission tomography (PET) scan - are performed.
Editor’s note
Dr Krishna Vakharia, 10th April 2025
The National Institute for Health and Care Excellence (NICE) has updated its guidance on assessment for myeloma in all ages including those under 60 years of age if they have persistent bone pain, especially back pain, or an unexplained fracture. In these individuals, NICE recommends a series of blood tests that a doctor should carry out.
These include a full blood count, calcium, erythrocyte sedimentation rate (ESR), serum paraproteins and serum free light chains. If serum free light chains are not possible, the doctor can look for Bence-Jones test to check for free light chains in urine a urine sample.
If any of these test results suggest myeloma, people should be referred using the suspected cancer pathway referral.
These tests may be repeated from time to time to monitor the progress of the disease and also to monitor the response to treatment.
Editor’s note
Dr Krishna Vakharia, 16th October 2023
The National Institute for Health and Care Excellence (NICE) has recommended that a person should receive a diagnosis or ruling out of cancer within 28 days of being referred urgently by their GP for suspected cancer.
Assessing the severity of myeloma
Tests which are commonly done to assess the severity of the disease and to monitor the response to treatment include:
Blood tests to check on your kidney function.
Blood tests to check the level of calcium in your blood.
Blood tests to check the level of paraprotein in your blood.
Chromosome and gene testing of the myeloma cells. This can help to identify the exact type of myeloma so that doctors can decide which treatment is best.
Blood tests to measure proteins in the blood, called beta-2 microglobulin and albumin. The levels of these proteins are affected by myeloma and give an indication as to the severity of the disease.
Other disorders related to myeloma
Back to contentsThe following are other plasma cell abnormalities. If you are diagnosed with any of these conditions, myeloma may develop sometime later, but not always.
Isolated (solitary) plasmacytoma of bone. In this condition only one plasma cell tumour is found in a bone. There is no other evidence of myeloma anywhere else in the body.
Extramedullary plasmacytoma. In this condition, one or more plasma cell tumours occur outside the bone marrow. These most commonly occur in the tonsils or the tissues around the nose.
Monoclonal gammopathy of unknown significance (MGUS). In this condition a paraprotein is found in the blood, without other symptoms or signs of myeloma. (Monoclonal gammopathy is another way of saying a high level of a monoclonal, or single type of, antibody.) This condition does not require treatment but needs monitoring. Around 1 in 100 people with MGUS develop myeloma in the future.
Aims of myeloma treatment
Back to contentsTreatments may be used to treat and to control the myeloma itself; also, to ease symptoms and complications of the myeloma. Treatment options are briefly discussed below.
Treatment is usually given to those people with myeloma who have some organ or tissue damage due to the myeloma. For example, if you are anaemic or have some impairment in the function of your kidneys.
Treatment is not usually started in those people who have no symptoms from their myeloma. However, these people are normally monitored closely by a specialist as there is a chance that treatment may be needed in the future.
However, different treatments suit different people. You should have a full discussion with a specialist who knows your case. They will be able to give the pros and cons, likely success rate, possible side-effects, and other details about the treatment options for myeloma.
In many cases, treatment can control the myeloma and put the disease into remission. Remission is not necessarily a cure. Full remission means that tests cannot detect the abnormal plasma cells in the blood or bone marrow, and the bone marrow is producing normal blood cells again.
Some remissions are partial which means there is some improvement, often a great improvement, but some myeloma cells remain. In many cases where there is remission or partial remission, at some point in the future the disease returns (relapses). Further treatment may be considered if the disease relapses. However, in time, the relapses become more difficult to treat.
Myeloma treatment
Back to contentsTreatment for myeloma may include one or more of the following:
Chemotherapy.
Steroids.
Radiotherapy.
Stem cell transplant.
Chemotherapy
Chemotherapy is a treatment which uses anticancer medicines to kill cancer (myeloma) cells, or to stop them from multiplying. Various medicines are used and myeloma may be treated with chemotherapy medicines given as tablets or injections. The exact combination of medicines used, and the length of the course of chemotherapy, depend on various factors. For example, the severity of the myeloma, the exact type of myeloma, if you have kidney damage, your age and general health.
If a course of chemotherapy achieves a remission, you may then be advised to take medicines as a regular maintenance treatment. These may include interferon, steroids, thalidomide, lenalidomide or bortezomib. This is, in effect, low-level chemotherapy which aims to keep you in remission for as long as possible.
Recent developments in medicines to combat myeloma have improved the outlook (prognosis). For example, tailoring treatment to the genetic make-up of the patient seems to be a promising way forward.
Your doctor will be able to discuss with you the most suitable type of chemotherapy for you in more detail.
Daratumumab monotherapy for treating relapsed and refractory multiple myeloma
NICE has published guidance on using daratumumab monotherapy for treating relapsed and refractory multiple myeloma.
Daratumumab is a monoclonal antibody. These medications target the cancer cells causing them to die without affecting the healthy ones. Monotherapy means that the medication is working on its own and not together with other medications.
NICE has recommended this treatment as an option if:
People with relapsed and refractory multiple myeloma have already had three treatments. These should include a proteasome inhibitor and an immunomodulator.
Their disease has become worse during their last treatment.
It has been shown that this medication can increase how long people live (though we don't know by how much) and that there is an increase in quality of life. This is because it is not as toxic as other medications used as chemotherapy.
Ixazomib with lenalidomide and dexamethasone for treating relapsed or refractory multiple myeloma
NICE has recommended that ixazomib, with lenalidomide and dexamethasone, is an option for treating multiple myeloma in adults, only if two or three different therapies have already been used.
See Further Reading and References below.
Editor’s note
Dr Krishna Vakharia, 27th June 2023
Daratumumab with bortezomib and dexamethasone for previously treated multiple myeloma
NICE has recommended the above treatment regime for those people who have had one treatment already with lenalidomide or if the lenalidomide cannot be used again as a second line treatment. Studies have shown that this combination of treatments reduces the risk of dying, or the chance of the myeloma becoming worse or returning.
Stem cell transplant
A stem cell transplant may be an option. It is an intensive treatment that is not suitable in all cases. However, this treatment generally gives the best chance of a complete remission.
Stem cells are the immature cells that develop into mature blood cells in the bone marrow. Briefly, a stem cell transplant involves high-dose treatment with chemotherapy (and sometimes radiotherapy) to kill all the abnormal plasma cells. However, this also kills the stem cells that make normal blood cells. So, after the high-dose treatment, some stem cells are given to you via a drip into a vein (like having a blood transfusion).
The stem cells are usually obtained from the blood of the patient with the myeloma before the high-dose treatment is started. The stem cells from the transfusion make their way to the bone marrow where they then multiply and make normal blood cells, including plasma cells. See the separate leaflet called Stem Cell Transplant for more details.
Induction treatment before stem cell transplant
If you are offered a stem cell transplant, your doctor will usually advise that before this you have a combination of treatments, including chemotherapy. This increases the chance that the transplant will be effective.
The standard 'induction therapy' is a combination of bortezomib plus thalidomide and dexamethasone. NICE has reviewed the evidence for adding an extra treatment, daratumumab, to this combination. They have found that adding this extra drug improves your chance of long-term survival and reduces the chance of the condition getting worse.
They have therefore recommended that doctors consider this new combination for people who haven't yet been treated for myeloma and who are suitable for stem cell transplant. See Further Reading below for the NICE reference details.
Radiotherapy
Radiotherapy is a treatment which uses high-energy beams of radiation which are focused on cancerous tissue. This kills cancer cells, or stops cancer cells from multiplying. For myeloma, radiotherapy is mainly used to treat severe localised problems and plasmacytomas. For example, to treat severe pain and/or pressure on nerves due to a damaged spinal bone because of a build-up of myeloma cells in the bone. See the separate leaflet called Radiotherapy for more details.
Treatments to ease symptoms
Depending on the effects of the myeloma, one or more of the following may be advised:
Painkillers - to ease any pain.
A bisphosphonate medicine. Bisphosphonates are a type of medicine that is used to strengthen your bones. It is now recommended that all people with myeloma that is causing any symptoms should take a bisphosphonate.
Erythropoietin. This is a hormone that helps to increase the number of red cells made in the bone marrow. It may be used to help improve anaemia.
Blood transfusions to correct anaemia.
Plasma exchange or exchange blood transfusions if you have a very high level of paraprotein in your blood, which is causing hyperviscosity symptoms.
Antibiotics if you develop infections. If you develop any symptoms to suggest an infection you should go to see a doctor as soon as possible. Some people will need to have intravenous antibiotics in hospital if they develop an infection.
Surgery is sometimes needed to help heal fractured bones or to ease pressure on a trapped nerve due to breaks (fractures) of the spinal bones.
Kidney dialysis if you develop kidney damage and kidney failure.
People with myeloma will also usually be advised to drink plenty of fluids (at least three litres a day). This helps to lower a high calcium level.
Myeloma prognosis
Back to contentsThe outlook (prognosis) is variable and in some cases the disease responds very well to treatment and survival is longer. In particular, a successful stem cell transplant gives a good chance of a complete remission. In some cases the disease does not respond to treatment very well, or life-threatening complications develop such as kidney failure.
Generally for people with myeloma in England:
Almost 85 out of every 100 will survive their myeloma for a year or more after diagnosis.
More than 50 out of every 100 will survive their myeloma for five years or more after diagnosis.
About 30 out of every 100 will survive their myeloma for 10 years or more after they are diagnosed.
The treatment of cancer and myeloma is a developing area of medicine. New treatments continue to be developed and the information on outlook, above, is very general. As mentioned above, there are some newer medicines that have been introduced in the last few years that show promise to improve the outlook. The specialist who knows your case can give more accurate information about the outlook for your particular situation.
Patient picks for Blood cancers
Cancer
Leukaemia
Leukaemia is a cancer of blood-forming cells. There are different types of leukaemia. If you develop leukaemia it is important to know what type it is. This is because the outlook (prognosis) and treatments vary for the different types.
by Dr Hayley Willacy, FRCGP

Cancer
Acute myeloid leukaemia
Acute myeloid leukaemia is where the bone marrow makes large numbers of abnormal immature white blood cells which are derived from a myeloid stem cell.
by Dr Laurence Knott
Further reading and references
- Bone Marrow Transplantation and Peripheral Blood Stem Cell Transplantation; National Cancer Institute (US)
- Myeloma: diagnosis and management; NICE Guidance, (February 2016 - last updated October 2018)
- Haematological cancers: improving outcomes; NICE Guidance (May 2016)
- Daratumumab in combination for untreated multiple myeloma when a stem cell transplant is suitable; NICE Technology appraisal guidance, February 2022
- Daratumumab monotherapy for treating relapsed and refractory multiple myeloma; NICE Technology appraisal guidance, April 2022
- Ixazomib with lenalidomide and dexamethasone for treating relapsed or refractory multiple myeloma; NICE Technology appraisal guidance, February 2023
- Multiple myeloma: diagnosis, treatment and follow-up; ESMO Clinical Practice Guideline (2021).
- Myeloma; Cancer Research UK
- Daratumumab with bortezomib and dexamethasone for previously treated multiple myeloma; NICE Technology appraisal guidance, June 2023
Continue reading below
Article history
The information on this page is written and peer reviewed by qualified clinicians.
Next review due: 18 Mar 2028
20 Mar 2023 | Latest version

Ask, share, connect.
Browse discussions, ask questions, and share experiences across hundreds of health topics.

Feeling unwell?
Assess your symptoms online for free
Sign up to the Patient newsletter
Your weekly dose of clear, trustworthy health advice - written to help you feel informed, confident and in control.
By subscribing you accept our Privacy Policy. You can unsubscribe at any time. We never sell your data.