Infective conjunctivitis
Peer reviewed by Dr Colin Tidy, MRCGPLast updated by Dr Philippa Vincent, MRCGPLast updated 26 May 2025
Meets Patient’s editorial guidelines
- DownloadDownload
- Share
- Language
- Discussion
In this series:Eye problemsAllergic conjunctivitisDry eyesEpiscleritis and scleritisUveitisSubconjunctival haemorrhage
Infective conjunctivitis is an infection of the thin skin (the conjunctiva) on the front of the eye. It is very common and often starts in one eye and then spreads to the other. It is generally known as conjunctivitis.
In this article:
Video picks for Eye symptoms
Key points
Conjunctivitis is an eye infection that affects the thin, clear layer that covers the white part of your eye. It often starts in one eye before spreading to the other.
When caused by a virus and bacteria it is known as infective conjunctivitis.
Common symptoms include red or 'pink eye', watery or gritty eyes, a sticky discharge, and mild soreness. It usually doesn't affect your vision.
Most cases clear up on their own within a few days. Eye drops, cool compresses, and keeping your eyes clean can help and stop it spreading.
See a doctor if symptoms get worse, don’t improve, or if you notice pain, light sensitivity, or vision changes.
What is conjunctivitis?
Conjunctivitis is a simple and common condition. The conjunctiva is the thin covering (like a very thin skin) that covers the white part of the eyes and the underside of the eyelids. '-itis' is the medical term that means inflammation.
Conjunctivitis is a very common condition in which one or both eyes become red or pink and may be sticky or watery. Almost everyone will have experienced it several times and will be familiar with the symptoms of sensation of grittiness and discomfort in the eyes, with redness and discharge. Sometimes the discharge can be thick and green; other times it is more watery.
What are the symptoms of conjunctivitis?
Back to contentsThe symptoms of conjunctivitis are generally very mild. Because the conjunctiva does not cover the iris and pupil, conjunctivitis should not affect light getting into the eye and should not affect vision.
Vision can appear blurred or misted because of discharge smeared over the surface of the eye, but this will usually clear on blinking or wiping the eyes.
Because the conjunctiva (unlike the cornea, which covers the iris and pupil) is not very sensitive, conjunctivitis is usually uncomfortable rather than painful.
The main symptom of infective conjunctivitis is 'pink eye'. The eye looks pink or red.
Infective conjunctivitis often begins most obviously in one eye but quickly spreads to both eyes. The whites of the eyes look inflamed.
The eyes may feel gritty and may water more than usual.
Some mild soreness may develop, particularly if you rub the eyes.
The eyelids may become swollen. They may be stuck together with gluey material (discharge) after a sleep. This is particularly common in bacterial conjunctivitis.
Vision is not normally affected. You may develop some blurring of vision, due to discharge at the front of the eye. However, this clears with blinking.
Conjunctivitis does not normally require a healthcare professional to diagnose it. You will realise that you (or your child) have conjunctivitis if you have the signs and symptoms above. However, if you have a pink or red eye with any of the symptoms below, you should seek medical advice as they suggest a different problem.
You should always seek medical advice if you suspect conjunctivitis in a newborn baby.
Note: whilst a sticky eye due to a blocked tear duct is a very common condition in babies, this condition does not cause reddening of the conjunctiva. You do not need to see a doctor about this unless it still persists when your baby is a year old.
What symptoms should I be concerned about when suspecting conjunctivitis?
You should always seek medical advice if your suspected conjunctivitis is particularly painful, or the discharge is particularly profuse. You may still be correct that you have conjunctivitis, but you may have one of the rare but more serious causes, or you may have another condition in addition to conjunctivitis.
Conjunctivitis should NOT be accompanied by any of the following symptoms:
Changes in your vision other than smearing.
Severe pain in the eye.
Inability to open the eye due to pain.
Extreme sensitivity to light in the eye.
Loss of the ability to focus.
Distorted images.
Flashing lights.
Headache.
Being sick (vomiting).
These or any other severe symptoms suggest another cause for your eye symptoms, and you should seek medical advice urgently.
Continue reading below
How common is conjunctivitis?
Back to contentsAnyone can get conjunctivitis. However, simple bacterial conjunctivitis is particularly common in children, whilst viral conjunctivitis is more common in adults.
Viral conjunctivitis is the most common overall cause of infectious conjunctivitis. Bacterial conjunctivitis is the second most common cause of infectious conjunctivitis.
What causes conjunctivitis?
Back to contentsInfective conjunctivitis may be caused by germs. Bacterial conjunctivitis is more common in children, whilst viral conjunctivitis is more common in adults.
Infection is the most common cause of conjunctivitis. This leaflet only concerns infective conjunctivitis. However, conjunctivitis may also be due to:
Allergy: many people with hay fever (pollen allergy) have a red and inflamed conjunctiva - the thin, clear covering over the white part of the eyes and inside of the eyelids. See the separate leaflet called Allergic conjunctivitis for more details. This can be treated with eye drops or other medications bought over the counter.
Irritation: irritant conjunctivitis sometimes occurs. For example, your conjunctiva may become inflamed after getting some shampoo in your eyes. Chlorine in swimming pools is a common cause of mild irritant conjunctivitis. Crowd control substances like tear gas cause a severe form of irritant conjunctivitis.
Continue reading below
What types of conjunctivitis are there?
Back to contentsMost cases of conjunctivitis are caused by the same viruses that cause coughs and the common cold, and conjunctivitis commonly develops when you have a cold or cough.
In the vast majority of cases, conjunctivitis is not serious.
Most bacterial conjunctivitis is mild. It usually clears within a week or so without antibiotics.
Most viral conjunctivitis is caused by a virus called adenovirus. This tends to cause a very red and more prolonged conjunctivitis. It is very contagious and may last 2-3 weeks. It tends to get worse over the first 4-5 days and then improve over the next 2 weeks.
Molluscum contagiosum virus can cause a mild conjunctivitis which, like adenovirus, can persist for several weeks. This is more common in children, and typically the little mole-like bumps of molluscum are visible on the eyelids or fingers.
More serious types of conjunctivitis
Rarely, infective conjunctivitis can more serious, with some rarer germs being capable of spreading into, and damaging, the cornea and the main part of the eye:
Some bacteria can cause more serious infective conjunctivitis.
Conjunctivitis in newborn babies can be caused by germs called chlamydia or gonorrhoea. These are sexually transmitted infections (STIs) in adults; babies can acquire them from the birth canal during childbirth. They cause a severe, very sticky conjunctivitis which can spread rapidly to the cornea and permanently damage the eye. They need urgent treatment. Note: this is different to the very common sticky eye of newborn babies, caused by a blocked tear duct. A blocked tear duct with sticky eye does not cause redness and inflammation of the conjunctiva. See the separate leaflet called Tear duct blockage in babies for more details.
Some adults can develop conjunctivitis due to chlamydia or gonorrhoea. These STIs cause a severe conjunctivitis, with extremely profuse discharge. They need urgent treatment as they can spread quickly to the cornea and can affect vision.
Some viruses can cause more serious viral conjunctivitis. These tend to cause marked pain, particularly if the cornea is also affected. They include:
Cold sore virus (herpes simplex virus), which in addition to causing a conjunctivitis, can cause keratitis and painful ulcers on the surface of the eye.
Shingles (varicella-zoster virus), which can cause inflammation of the inside of the eye and can affect vision.
Trachoma is conjunctivitis caused by a different form of chlamydia to the one that causes STIs in the UK. Repeated infection particularly affects the underside of the eyelids and gradually leads to scarring and loss of vision. It is widespread in many of developing countries but is rarely seen in the UK.
Conjunctivitis can sometimes be one part of a more serious infection of the cornea or of deeper structures of the eye. This is suggested by symptoms of eye pain, reduced vision, or swelling around the eye.
There are several serious eye conditions which are not caused by infection, but which make the eye red. These conditions include acute glaucoma and uveitis. These conditions generally markedly affect vision, and most also cause severe pain.
How to treat conjunctivitis
Back to contentsMost episodes of infective conjunctivitis settle down in less than a week with simple self-management. That means that in many cases, you don't need medical help at all. Antibiotics are only occasionally needed.
Not treating - this is a common option for mild or moderate infections. Your tears contain chemicals that fight off the bacteria.
Bathing the eyes - using cool boiled water; this may be soothing.
Lubricating eye drops - these may reduce eye discomfort. They are available over the counter.
Antibiotic preparations
Antibiotics for conjunctivitis are available over the counter from a pharmacist. These might be:
Eye drops such as chloramphenicol.
Eye ointment such as chloramphenicol or fusidic acid (actually an oily drop, halfway between an ointment and a drop).
Note: treatment using antibiotic preparations tends to be for more severe cases, as they make very little difference in mild cases, which get better anyway. It is also used for those cases not clearing on their own. (Tell your doctor if you are pregnant, as some eye drops may not be suitable.)
Other general advice
Do not wear contact lenses until symptoms have completely gone and for 24 hours after the last dose of any eye drops or ointment.
You can clean secretions from eyelids and lashes with cotton wool soaked in water.
Infective conjunctivitis is contagious, which means it can be passed on by touching. The likelihood of passing on the infection is not high unless you are in close contact with others. Washing your hands regularly, particularly after touching your eyes, and not sharing towels or pillows, will help avoid it.
What is the treatment for viral conjunctivitis?
Viral conjunctivitis infection usually settles by itself within 2-4 weeks. You can help make it more comfortable with cold compresses and lubricants, such as chilled artificial tears (available from pharmacies). Occasionally a pharmacist or other healthcare professional may suggest antibiotic drops to prevent additional bacterial infection.
Preventing transmission of viral conjunctivitis is important. Wash your hands thoroughly and often, keep hands away from your eyes and avoid sharing towels and cosmetics. Those who wear contact lenses should stop using them until the condition has settled down.
What should I look out for?
Back to contentsSee a doctor if symptoms change, or do not start to settle within a few days, or if you are concerned that you have anything other than a common conjunctivitis. In particular, see a doctor urgently if:
You develop marked eye pain.
Light starts to hurt your eyes (photophobia).
Spots or blisters develop on the skin next to the eye.
Your vision becomes affected.
Your newborn or very young baby develops conjunctivitis.
Most conjunctival infections are not serious, do not harm the eye, and clear in a few days. However, some infections such as herpes or chlamydia persist for longer than usual, are more serious and need special treatment.
Most serious eye infections feel different to simple conjunctivitis because they cause significant pain. Many also affect vision. Some other conditions, including allergic conjunctivitis, can appear similar to infective conjunctivitis initially. This makes it particularly important that you go back to your doctor if things become worse or if they do not settle as expected.
What else do I need to know?
Back to contentsThe image below shows how the conjunctiva runs over the surface of the white part of the eye and over the underside of the eyelids.
Side View of the Eye
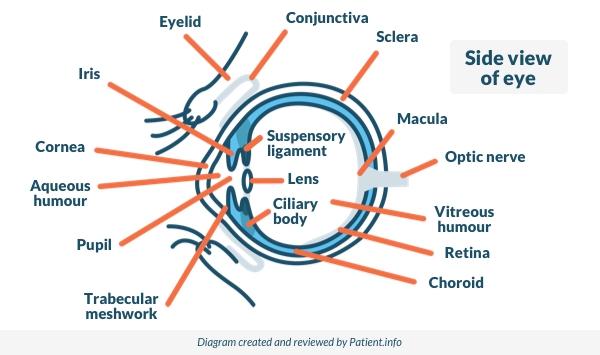
You will see that the conjunctiva does not cover the coloured part of the eye (the iris) and the dark, circular part of the eye (the pupil). This part of the eye is the cornea. The cornea is much more sensitive than the conjunctiva. Infection or inflammation of the cornea is called keratitis and it is a more serious condition.
Infection of the conjunctiva causes mild symptoms only. As the conjunctiva does not cover the part of the eye that lets light in for vision, conjunctivitis should not affect your vision. The only exception to this is if you have a lot of discharge in your eye and it smears over the surface - but in this case it should clear on blinking or wiping.
Severe pain, or change in your vision that is not caused by smearing, would suggest a condition affecting the cornea rather than the conjunctiva, and this should always be seen by a healthcare professional.
Does a child with conjunctivitis need to stay off school?
Back to contentsGuidance from UK Health Security Agency (formerly known as Public Health England ) states that children do not need to be excluded from school or from childcare if they have infective conjunctivitis, unless there is an outbreak of several cases. This is because conjunctivitis is a mild condition which represents no danger to others, whilst breaks in school attendance affect your child's learning.
Some nursery and daycare facilities take the view that conjunctivitis is a nuisance for other parents, and is more easily passed amongst small children who tend to have close physical contact with one another. They may ask you to keep your child at home until the eye is no longer red or sticky, in order to prevent other parents being affected or annoyed.
If an outbreak occurs, with many cases, the school or childcare centre may seek advice from UK Health Security Agency or other health professional.
Frequently asked questions
Back to contentsHow do you know if conjunctivitis is infectious?
Conjunctivitis is usually infectious if it causes redness, discharge, and affects both eyes or spreads quickly to others. Bacterial and viral forms are contagious, whereas allergic or irritant conjunctivitis is not.
How to treat conjunctivitis when pregnant?
If you have conjunctivitis while pregnant, treatment depends on the cause. Viral or allergic conjunctivitis often clears on its own, while bacterial cases may need antibiotic eye drops that are safe to use in pregnancy - always check with your doctor or pharmacist first.
Is infective conjunctivitis serious?
Infective conjunctivitis is usually not serious and often clears on its own within one to two weeks. However, it can be uncomfortable and highly contagious, so good hygiene and avoiding touching your eyes are important.
Dr Mary Lowth is an author or the original author of this leaflet.
Patient picks for Eye symptoms

Eye health
Allergic conjunctivitis
Allergic conjunctivitis causes red, watery, itchy or gritty eyes. The condition is not usually painful and does not make eyes sensitive to light. It does not affect vision. The most common cause is an allergy to pollen in the hay fever season. Other causes are allergies to house dust mite, cosmetics, and problems with contact lenses, although these are less common. Eye drops usually ease symptoms.
by Dr Philippa Vincent, MRCGP
%2Fog.png&w=1600&q=75)
Eye health
Eye infection (herpes simplex)
A herpes simplex eye infection, or eye herpes, is a viral infection caused by the herpes simplex virus (HSV). It can damage the eye and affect vision, so see a doctor if your eye becomes red, sore, or painful, especially after having a cold sore.
by Dr Hayley Willacy, FRCGP
Further reading and references
- Sheikh A, Hurwitz B, van Schayck CP, et al; Antibiotics versus placebo for acute bacterial conjunctivitis. Cochrane Database Syst Rev. 2012 Sep 12;(9):CD001211. doi: 10.1002/14651858.CD001211.pub3.
- Guidance on infection control in schools and other childcare settings; UK Health Security Agency (September 2017 - last updated February 2023)
- Conjunctivitis - infective; NICE CKS, October 2022 (UK access only)
- Conditions for which over-the-counter items should not be routinely prescribed
Continue reading below
Article history
The information on this page is written and peer reviewed by qualified clinicians.
Next review due: 25 May 2028
26 May 2025 | Latest version

Ask, share, connect.
Browse discussions, ask questions, and share experiences across hundreds of health topics.

Feeling unwell?
Assess your symptoms online for free
Sign up to the Patient newsletter
Your weekly dose of clear, trustworthy health advice - written to help you feel informed, confident and in control.
By subscribing you accept our Privacy Policy. You can unsubscribe at any time. We never sell your data.