Overactive thyroid gland
Hyperthyroidism
Peer reviewed by Dr Doug McKechnie, MRCGPLast updated by Dr Colin Tidy, MRCGPLast updated 15 Oct 2024
Meets Patient’s editorial guidelines
- DownloadDownload
- Share
- Language
- Discussion
- Audio Version
In this series:GoitreThyroid eye diseaseThyroid function testsThyroid scans and uptake testsAntithyroid medicines
Hyperthyroidism is an uncommon condition where your thyroid gland (which is in your neck) goes into 'overdrive'. It produces too much of a chemical called thyroxine. We all have a certain amount of thyroxine in our bodies to keep us working at just the right 'energy level'. If too much thyroxine is made, you can become very ill with tiredness, a fast heartbeat and weight loss.
Initially the symptoms can mimic lots of other conditions. However, the diagnosis is usually made with a simple blood test. A number of treatments are available which makes hyperthyroidism fairly easy to treat: tablets are the mainstay of treatment, followed by radiotherapy. Occasionally surgery is needed.
In this article:
Video picks for Thyroid problems
Continue reading below
What is hyperthyroidism?
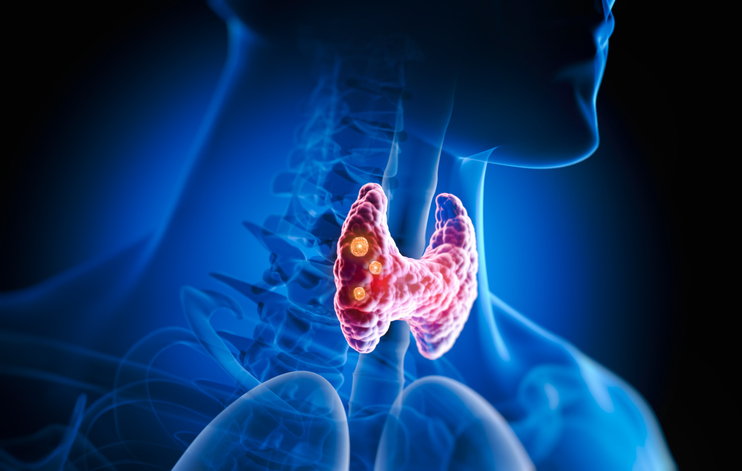
Neck cross-section showing the thyroid gland
Hyperthyroidism means an overactive thyroid gland. When your thyroid gland is overactive it makes too much thyroxine.
The extra thyroxine causes many of your body's functions to speed up. In contrast, if you have hypothyroidism, you make too little thyroxine; this causes many of the body's functions to slow down. See the separate leaflet called Underactive thyroid gland (Hypothyroidism) for more information.
Thyroxine is a body chemical (hormone) made by your thyroid gland. It is carried around your body in your bloodstream. It helps to keep your body's functions (your metabolism) working at the correct pace. Many cells and tissues in your body need thyroxine to keep them going correctly.
Thyrotoxicosis is a term that may be used by doctors instead of hyperthyroidism. The two terms mean much the same.
Symptoms of hyperthyroidism
Back to contentsThe following are symptoms of having an overactive thyroid gland (hyperthyroidism):
Being restless, nervous, emotional, irritable, sleeping poorly and 'always on the go'.
Tremor of your hands.
Losing weight despite an increased appetite.
The sensation of having a 'thumping heart' (palpitations).
Sweating, a dislike of heat and an increased thirst.
Runny stools (diarrhoea) or needing to go to the toilet to pass stools more often than normal.
Skin problems such as hair thinning and itch.
Menstrual changes - your periods may become very light or infrequent.
Tiredness and muscle weakness may be a feature.
A swelling of your thyroid gland (a goitre) in the neck may occur.
Eye problems if you have Graves' disease - see below under 'What are the causes of hyperthyroidism?'.
Most people with hyperthyroidism do not have all the symptoms but a combination of two or more is common. Symptoms usually develop slowly over several weeks. All the symptoms can be caused by other problems and so the diagnosis may not be obvious at first. Symptoms may be mild to start with but become worse as the level of thyroxine in your blood gradually rises.
Continue reading below
How common is hyperthyroidism?
Back to contentsAbout 1-2 in 100 women and 2 in 1,000 men in the UK develop an overactive thyroid gland (hyperthyroidism) at some stage of their lives. It can occur at any age but it is more common as you become older.
What are the causes of hyperthyroidism?
Back to contentsThere are various causes of having an overactive thyroid gland (hyperthyroidism). They include the following:
Graves' disease
This is the most common cause. It can occur at any age but is most common in women aged 20-50 years. It can affect anyone but there is often a family history of the condition. There may also be family members with other autoimmune diseases (for example, diabetes, rheumatoid arthritis and myasthenia gravis).
Graves' disease is also an autoimmune disease. The immune system normally makes tiny proteins (antibodies) which travel in your bloodstream to attack bacteria, viruses and other germs.
In autoimmune diseases, the immune system makes antibodies against tissues of your body. If you have Graves' disease, you make antibodies that attach to your thyroid gland. These stimulate your thyroid gland to make lots of thyroxine. It is thought that something triggers your immune system to make these antibodies. The trigger is not known.
In Graves' disease the thyroid gland usually enlarges, which causes a swelling (goitre) in the neck. See the separate leaflet called Goitre (Thyroid swelling). The eyes are also affected in about half of cases. If they are affected, your eyes are pushed forwards and look more prominent (proptosis). This can cause discomfort and watering of your eyes.
Problems with eye muscles may also occur and lead to double vision. It is not clear why eye symptoms occur in some people who have Graves' disease. They may be due to the antibodies affecting the tissues around the eye. See the separate leaflet called Thyroid eye disease for more details.
Thyroid nodules
This is a less common cause of hyperthyroidism. Thyroid nodules are lumps which can develop in your thyroid gland. It is not clear why they develop. They are usually non-cancerous (benign) but contain abnormal thyroid tissue.
Some thyroid nodules are non-functional (don't produce any thyroid hormone) but some do, and those are the ones that can rarely cause hyperthyroidism. The abnormal thyroid tissue in some thyroid nodules does not respond to the normal controlling system which normally ensures that you make just the right amount of thyroxine. Therefore, if you have a thyroid nodule, you may make too much thyroxine.
Sometimes only one nodule forms. This is called a toxic solitary adenoma. This most commonly occurs in people aged between 30 and 50 years.
The thyroid may become generally lumpy or nodular. This most commonly occurs in older people and is called a toxic multinodular goitre.
Note: the word toxic above, relating to adenomas or multinodular goitres, does not mean poisonous. It is just one of those medical words which refers to the hyperthyroidism.
Other causes
There are several other rare causes of hyperthyroidism. For example, some people who take the medicines amiodarone and lithium develop hyperthyroidism. There are various other rare conditions which result in excess thyroxine being made.
Continue reading below
How is hyperthyroidism diagnosed?
Back to contentsA blood test can diagnose having an overactive thyroid gland (hyperthyroidism). A normal blood test will also rule it out if symptoms suggest that it may be a possible diagnosis. One or both of the following may be measured in a blood sample:
Thyroid-stimulating hormone (TSH). This chemical (hormone) is made in the pituitary gland in the brain. It is released into the bloodstream. It stimulates the thyroid gland to make thyroxine. If the level of thyroxine in the blood is high then the pituitary gland releases less TSH. Therefore, a low level of TSH means that your thyroid gland is overactive and is making too much thyroxine.
Thyroxine (T4). A high level of T4 confirms hyperthyroidism.
Sometimes the results of the tests are borderline. For example, a normal T4 but with a low TSH. Other tests are sometimes done to clarify the situation and the cause. For example, another blood test that measures T3 is sometimes helpful and an ultrasound scan of the thyroid gland or a thyroid scan may be done if you have a nodular goitre.
Also, if tests are borderline, one option is to repeat the tests a few weeks later, as sometimes borderline tests are due to another illness. Other tests may be done if a rare cause of hyperthyroidism is suspected.
In people with Graves' disease a blood test may detect specific autoantibodies which are commonly raised. However, these can also be raised in some people without Graves' disease so this is not a specific test for Graves' disease.
See the separate leaflet called Thyroid function tests for more information.
Hyperthyroidism treatment
Back to contentsThe main aim of treatment of an overactive thyroid gland (hyperthyroidism) is to reduce your level of thyroxine to normal. Other problems, such as a large thyroid swelling (goitre) or associated eye problems, may also need treatment.
Factors such as the underlying cause of the problem, your age and the size of any goitre are taken into account to decide on the best treatment plan.
Treatment options include the following:
Antithyroid medicines
Antithyroid medicines can reduce the amount of thyroxine made by the overactive thyroid gland. The most common medicine used in the UK is carbimazole.
Carbimazole does not affect the thyroxine which is already made and stored but reduces further production. Therefore, it may take 4-8 weeks of treatment for your thyroxine level to come down to normal. The dose of carbimazole needed to keep the thyroxine level normal varies from person to person. A high dose is usually given initially which is then reduced as your thyroxine levels come down.
Carbimazole is usually taken for 12-18 months at first. After this, in about half of cases, the condition will have settled down and the carbimazole can be stopped. If the condition flares up again some time in the future, a further course may be needed. However, in these cases an alternative treatment (for example, radioactive iodine) is often recommended.
In about half of cases, carbimazole needs to be continued long-term to control symptoms. A different treatment may then be a better option if you do not want to take carbimazole long-term.
Warning: carbimazole can, rarely, affect your white blood cells which fight infection. Whilst taking carbimazole, you should see a doctor urgently for a blood test if you develop any of the following:
A high temperature (a fever).
A sore throat.
Mouth ulcers.
You should also stop taking carbimazole until you receive further instruction from your doctor.
Taking carbimazole in early pregnancy slightly increases the risk of certain birth defects in the baby. An alternative medicine, propylthiouracil, is safer, and usually used instead for women who are planning a pregnancy, or become pregnant. Carbimazole is safe to take if you are breastfeeding. If you are planning a pregnancy, speak to your endocrinologist about the options for medication.
Radio-iodine
This involves taking a drink, or swallowing a capsule, which contains radioactive iodine. The main use of iodine in your body is to make thyroxine. Therefore, the radioactive iodine builds up in your thyroid gland.
As the radioactivity is concentrated in your thyroid gland, it destroys some thyroid tissue which reduces the amount of thyroxine that you make. The dose of radioactivity to the rest of your body is very low and is not dangerous. However, it is not suitable if you are pregnant or breastfeeding. In addition, after treatment, women should not become pregnant for at least six months and men are advised not to father children for at least four months.
Following radio-iodine treatment, you should avoid prolonged contact with others for a specified time. This may be for 2-4 weeks, depending on the amount of radio-iodine you receive. The aim is to limit the exposure of radioactivity to others. For the specified period you will be advised to take precautions such as:
Limit close contact with babies, children or pregnant women. Close contact means being within one metre; so, for example, don't cuddle children or allow them to sit on your lap.
You may wish to apply similar precautions as above for contact with your pets.
If you have children, or have a job where you have contact with children, you should discuss this with the specialist before treatment.
Stay more than an arm's length away from other people.
Sleep alone.
Avoid going to places like cinemas, theatres, pubs and restaurants where you may be in close contact with other people.
Take some time off work if your work involves close contact with other people.
Your specialist will give more detailed advice regarding these precautions.
Surgery
This involves removing part of your thyroid gland. It may be a good option if you have a large goitre which is causing problems in your neck. If too much thyroid tissue is removed then you will be given thyroxine tablets to keep your thyroxine level normal.
It is usually a safe operation. However, as with all operations, there is a very small risk of complications.
Thyroid replacement therapy
It can be difficult for a doctor to judge just the right dose of carbimazole, or just the right amount of radio-iodine, to give in each case. Too much treatment may make your thyroxine level go too low. Not enough treatment means your level remains higher than normal. Regular blood tests are needed to check on the thyroxine level.
One option is to take a high dose of carbimazole each day deliberately, or to receive a one-off high dose of radio-iodine. This stops your thyroid gland making any thyroxine. You will then need to take a daily dose of thyroxine tablets to keep your blood level of thyroxine normal. This over-treatment and then taking replacement thyroxine is called 'block and replace'.
Treatment for eye problems
You may need to see an eye specialist if you develop the eye problems of Graves' disease. Relatively minor symptoms affect the eyes in about half of people with Graves' disease. Measures such as artificial tears, sunglasses and eye protectors whilst you sleep may be sufficient to help.
However, about 1 in 20 people with Graves' disease have severe eye changes. Treatment can then be more difficult and may include surgery, radiation treatment or steroid tablets.
If you smoke then it is important that you try to stop. Smoking can actually make your eye problems worse.
Beta-blocker medicines
Some people are given a beta-blocker medicine (for example, propranolol, atenolol) for a few weeks whilst the level of thyroxine is reduced gradually by one of the above treatments.
Beta-blockers can help to reduce symptoms of tremor, the sensation of having a 'thumping heart' (palpitations), sweating, agitation and anxiety.
Complications of hyperthyroidism
Back to contentsIf you have untreated hyperthyroidism:
You have an increased risk of developing heart problems such as abnormal heart rhythm (atrial fibrillation), a weak heart (cardiomyopathy), angina and heart failure.
If you are pregnant, you have an increased risk of developing some pregnancy complications.
You have an increased risk of developing fragile bones (osteoporosis).
With treatment, the outlook (prognosis) is excellent as most of the symptoms and risks of complications go.
Follow-up
Back to contentsRegular checks are recommended, even after you finish a successful treatment for an overactive thyroid gland (hyperthyroidism).
It is very important to have a regular blood test (at least every year) to check that you have the right level of thyroid hormone (thyroxine) in your blood. Your GP may do this test. This is because some people become hyperthyroid again at some time in the future.
Others who have been treated successfully develop an underactive thyroid gland (hypothyroidism) in the future. If this occurs, it can usually be treated easily with thyroxine tablets.
Patient picks for Thyroid problems
Hormones
Underactive thyroid gland
If you have an underactive thyroid gland, the condition is called hypothyroidism. In hypothyroidism, there is a reduced level of thyroid hormone in the body. This can cause various symptoms, the most common being tiredness, weight gain, constipation, aches, dry skin, lifeless hair and feeling cold. Treatment usually involves taking a daily tablet of thyroid hormone to replace the missing thyroxine. Treatment works very well for most people with hypothyroidism but is required for life.
by Dr Colin Tidy, MRCGP

Hormones
Iodine deficiency
Iodine is essential for the body to make thyroid hormone. Low levels of iodine may cause an underactive thyroid gland and symptoms of hypothyroidism (eg, tiredness, constipation and weight gain). Iodine deficiency in pregnant women may cause problems for the baby, including learning disability. There has been a worldwide campaign to prevent iodine deficiency by using salt containing added iodine. However, iodine deficiency is still a widespread problem in many countries. Mild iodine deficiency may still affect some people in the UK.
by Dr Rosalyn Adleman, MRCGP
Further reading and references
- Thyroid disease: assessment and management; NICE guidance (November 2019 - last updated October 2023)
- CKS Hyperthyroidism; NICE CKS, January 2021 (UK access only)
- Mathew P, Rawla P; Hyperthyroidism. StatPearls, March 2023.
Continue reading below
Article history
The information on this page is written and peer reviewed by qualified clinicians.
Next review due: 14 Oct 2027
15 Oct 2024 | Latest version

Ask, share, connect.
Browse discussions, ask questions, and share experiences across hundreds of health topics.

Feeling unwell?
Assess your symptoms online for free
Sign up to the Patient newsletter
Your weekly dose of clear, trustworthy health advice - written to help you feel informed, confident and in control.
By subscribing you accept our Privacy Policy. You can unsubscribe at any time. We never sell your data.