How to prevent varicose veins
Peer reviewed by Dr Doug McKechnie, MRCGPLast updated by Victoria RawLast updated 24 Sept 2024
Meets Patient’s editorial guidelines
- DownloadDownload
- Share
- Language
- Discussion
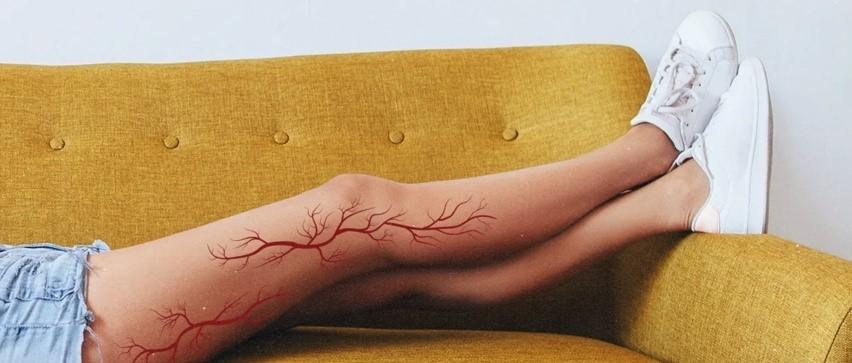
Varicose veins will affect nearly one third of us at some point in our lives. For those who do develop these visible and protruding leg veins, another third will experience symptoms of depression. Unfortunately, we can't prevent varicose veins from developing, but by following five healthy lifestyle habits we can slow down their progression and minimise discomfort.
In this article:
Continue reading below
What causes varicose veins?
You may have heard of varicose veins - a fairly common condition that around one in three of the UK population will develop during their lifetime1. What you may not know is that varicose veins aren't always obvious. This can mean that many of us neglect to follow the lifestyle habits that support our vein health.
Professor Mark Whiteley, leading consultant venous surgeon and founder of The Whiteley Clinic says: "In their simplest form, varicose veins can be identified as bulging veins which protrude from the legs. However, up to half of all people who have them will show no overt symptoms of varicose veins, as the problematic veins remain hidden under the skin. We call these 'hidden varicose veins'.
"Most people have a combination of causes for their varicose veins or 'hidden varicose veins', and so it is essential that all the causes are found and treated. This is why the National Institute for Health and Care Excellence (NICE) guidelines say that patients with varicose veins need to be seen by doctors working in teams2."
The first cause - a number of small communicating leg veins (perforators) that take blood in from your skin to the deep veins in your muscles. When their valves fail, blood is released into the surface veins.
The second cause (pelvic congestion syndrome, or PCS) - a medical condition caused by internal varicose veins in the lower abdomen and pelvis, which cannot be seen on the surface.
Symptoms of varicose veins
Not everyone will experience the same symptoms, but Whiteley shares a helpful mnemonic device listing some of the key indicators to keep an eye out for:
V - Veins which are visible on the surface of the skin, or just underneath it.
E - Enlarged veins that are blue or dark purple in colour.
I - Itchy, sore or dry skin just above the ankle or over the bulging veins.
N - Nodular, hard, and tender veins.
S - Swollen, achy or heavy legs and ankles.
Are varicose veins dangerous?
Sadly, even though they happen to a lot of us, visible varicose veins often affect people's self-esteem. One study of 100 people even found a strong link between varicose veins and undiagnosed depression3.
The appearance of them is often a driving force for people becoming interested in how to prevent varicose veins. Yet, Whiteley also stresses that it is a common misconception that this condition is solely a cosmetic issue. If treatment for varicose veins is ignored, they can go on to cause a lot of problems.
"This is why the NICE guidelines2 say that varicose veins with any symptoms or signs should be scanned and treated in specialist units," he adds.
Possible health problems
Although varicose veins rarely lead to serious health issues, Whitley outlines some possible complications:
Blood clots - superficial vein thrombosis (SVT) and deep vein thrombosis (DVT) are blood clots that develop within a vein.
SVT (also called phlebitis) - the clot is in the superficial veins and appears as a hard, red, painful lump. If the SVT gets within 5-7 cm of the deep vein, it can throw a clot off to the lungs - a pulmonary embolism (PE). Anyone with SVT, or 'phlebitis' should be referred for a duplex scan to see if they need anticoagulation.
DVT - a clot in the deep veins that usually does not move, but if left untreated can cause scar tissue in the wall. This can result in swollen, discoloured and painful legs, and sometimes leg ulcers, a condition called post thrombotic syndrome (PTS). In more serious cases, DVT can lead to PE.
Leg ulcers - research suggests that one in 20 people with 'simple' varicose veins will go on to experience leg ulceration if left untreated. Leg ulcers occur when the skin has broken down to reveal open sores which are unable to heal naturally and can often become infected if not treated correctly. However, they can now be treated - and even prevented - by local anaesthetic varicose vein surgery.
Continue reading below
Can you prevent varicose veins?
Unfortunately, developing varicose veins is sometimes unavoidable - for example, your age, family history of the condition, and being female. Other factors in your life can also increase your likelihood of developing varicose veins. These include obesity, hormone replacement therapy, and pregnancy - varicose veins are almost twice as common in women who have been pregnant, compared to women who have never been pregnant4.
"You cannot prevent varicose veins," says Whiteley. "However, there are some things you can do to minimise any discomfort in your legs, and slow down the progression of the condition, if you do have varicose veins or 'hidden' varicose veins."
Vein Health Awareness Week falls in September each year. Started by Professor Mark Whiteley, this aims to raise awareness of the importance of good vein health, how to spot venous disease, and when to get checked.
Habits that help prevent varicose veins
Let's explore the five healthy lifestyle habits that can aid prevention of varicose veins and help to delay problems with your veins.
1. Elevate your legs
"Raising your legs while you're sitting will help lower the pressure in your legs by allowing blood that has pooled in the veins to drain away - reducing your chance of skin damage and blood clots," advises Whiteley.
"This is a simple daily habit you can adopt while on the sofa. If you work at a desk from home, you could even prop up your legs while working using a footstool or cushions."
2. Get moving
"It is very important you get moving every hour to help keep your blood circulation working," says Whiteley. "Sitting or standing for long periods of time can make it harder for your blood to travel in the leg veins against gravity. This causes an increase in pressure in the veins, resulting in blood beginning to pool around the ankles."
3. Exercise regularly
We know that regular exercise supports our health in all sorts of ways, from keeping our hearts healthy to regulating our weight. Preventing varicose veins may be one of the lesser-known reasons to work out.
"Low-impact exercises such as yoga are particularly good at improving blood circulation," Whiteley adds. "The bending and stretching movements involved in the practice help to compress and decompress the blood vessels."
4. Watch your diet
Being overweight or obese increases the pressure in the veins lower down in your legs and could cause your ankles to swell. Therefore, a poor diet that is high in saturated fats and sugar increases your likelihood of varicose veins.
To maintain a healthy weight, make sure you eat a nutritious diet made up of all the food groups5 - including lots of fruit and vegetables. Be mindful of the recommended daily calorie intake for your sex.
5. Wear supportive socks or stockings
Supportive stockings from your doctor - also called graduated pressure or compression stockings - can help to relieve aching legs. Whiteley advises that even ones that sit below the knee can make your legs feel much better. These are often prescribed after your doctor has checked there are no problems with the arteries in your legs.
Continue reading below
Further reading
Patient picks for Blood vessels

Heart health and blood vessels
Cheese could protect blood vessels from damage caused by high-salt diet
US researchers found cheese can help protect blood vessels against damage done by sodium, according to new findings.
by Ashwin Bhandari

Heart health and blood vessels
What is Chronic Venous Insufficiency?
US President Donald Trump’s has been diagnosed as having chronic venous insufficiency (CVI). We look at how CVI affects your heart health, what causes it, and the signs to look out for.
by Lawrence Higgins
Continue reading below
Article history
The information on this page is peer reviewed by qualified clinicians.
Next review due: 26 Sept 2027
24 Sept 2024 | Latest version
20 Sept 2022 | Originally published
Authored by:
Amberley Davis

Ask, share, connect.
Browse discussions, ask questions, and share experiences across hundreds of health topics.

Feeling unwell?
Assess your symptoms online for free
Sign up to the Patient newsletter
Your weekly dose of clear, trustworthy health advice - written to help you feel informed, confident and in control.
By subscribing you accept our Privacy Policy. You can unsubscribe at any time. We never sell your data.