Venous leg ulcers
Peer reviewed by Dr Colin Tidy, MRCGPLast updated by Dr Hayley Willacy, FRCGP Last updated 26 Sept 2023
Meets Patient’s editorial guidelines
- DownloadDownload
- Share
- Language
- Discussion
- Audio Version
In this series:Varicose veinsVaricose eczemaSuperficial thrombophlebitis
Venous leg ulcers are common in older people. The most important part of treatment is for compression bandages to be applied correctly by a nurse. Keep as active as possible but elevate your leg when you are resting. Other treatments may be advised in some cases, such as a skin graft or vein surgery. After an ulcer has healed you should wear a support stocking each day, which helps to prevent it recurring.
In this article:
Video picks for Veins
Continue reading below
What is a venous leg ulcer?
A skin ulcer develops when an area of skin breaks down to reveal the underlying flesh. Venous leg ulcers are the most common type of skin ulcer. They mainly occur just above the ankle. They usually affect older people and are more common in women.
Varicose ulcer
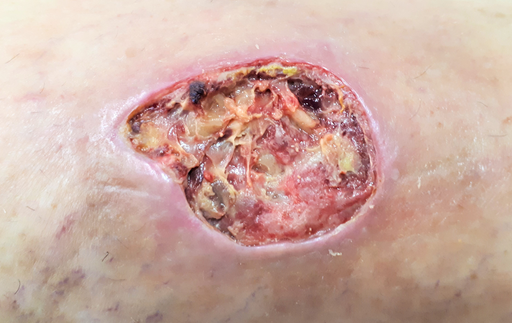
© Raimundo Pastor, CC BY-SA 4.0, via Wikimedia Commons
Raimundo Pastor, CC BY-SA 4.0, via Wikimedia Commons
Chronic venous insufficiency & Venous ulcer

© Ashashyou, CC BY-SA 4.0, via Wikimedia Commons
Ashashyou, CC BY-SA 4.0, via Wikimedia Commons
How common are leg ulcers?
Back to contentsVenous leg ulcers are the most common type of leg ulcer, causing about 3 in 4 of all leg ulcers. They affect about 1 in 100 people in the UK at some stage in their lives. Venous leg ulcers become more common as you get older. Most are painless but some are painful. Without treatment, an ulcer may become larger and cause problems in the leg. Skin inflammation (dermatitis) sometimes develops around a venous ulcer.
Non-venous skin ulcers are less common. For example, a skin ulcer may be caused by poor circulation due to artery disease in the leg, problems with nerves that supply the skin, or other problems. The treatment for non-venous ulcers is different to that of venous ulcers.
The rest of this leaflet deals only with venous leg ulcers.
Continue reading below
What causes venous leg ulcers?
Back to contentsThe root of the problem is increased pressure of blood in the veins of the lower leg. This causes fluid to ooze out of the veins beneath the skin. This causes swelling, thickening and damage to the skin. The damaged skin may eventually break down to form an ulcer.
The increased pressure of blood in the leg veins is due to blood collecting in the smaller veins next to the skin. The blood tends to collect and pool because the valves in the larger veins become damaged by a previous blood clot (thrombosis) in the vein, or varicose veins. Gravity causes blood to flow back through the damaged valves and pool in the lower veins.
How is a venous leg ulcer diagnosed?
Back to contentsThe appearance of a venous leg ulcer is usually fairly typical. It often looks different to ulcers caused by other problems such as poor circulation or nerve problems.
To rule out poor circulation as a cause, it is usual for a doctor or nurse to check the blood pressure in the ankle and in the arm. The ankle blood pressure reading is divided by the arm blood pressure reading to give a blood pressure ratio called the Ankle Brachial Pressure Index (ABPI).
If the ratio is low (less than 0.8) it indicates that the cause of the ulcer is likely to be poor circulation (peripheral arterial disease) rather than venous problems. This is very important to know as the treatments are very different. An ABPI may be checked every six months or so to make sure the circulation to the legs remains good.
Certain blood and urine tests may also be done to rule out conditions such as anaemia, diabetes, kidney problems and rheumatoid arthritis, which may cause or aggravate certain types of skin ulcer.
In complicated cases you may need to have an ultrasound scan, CT scan or MRI scan to produce a detailed map of the blood circulation in your leg.
Continue reading below
Venous leg ulcer treatment
Back to contentsThe ulcer is dressed in a similar way to any other wound. Typically, a nurse will do this every week or so. The wound is cleaned when the dressing is changed - normally with ordinary tap water. However, an ulcer is unlikely to heal with just dressings. In addition to a dressing, the following treatments help the ulcer to heal.
Compression bandaging
Wearing a compression bandage is the most important part of treatment. The aim is to counteract the raised pressure in the leg veins. This gives the best chance for the ulcer to heal. The common method is for a nurse to put on 2-4 layers of bandages over the dressing. When the bandages are put on, the pressure is put highest at the ankle and gradually less towards the knee and thigh. A support (compression) stocking over the dressing is sometimes used as an alternative but not thought to be as good as bandaging.
The bandages are reapplied every week or so. It is best to put the bandages on after you have raised (elevated) the leg for several hours or overnight (see below). So, make extra effort to keep your leg elevated just before the nurse is due to see you.
A note of caution: when you have a compression bandage on you should still be able to move your ankle around. Occasionally, the compression is too tight, or it may affect the circulation in the legs. Therefore, take off the bandages if your foot changes colour or temperature, or if you have increasing pain. Then see your doctor or nurse for advice.
Elevation and activity
When you are resting, if possible, try to keep your leg raised higher than your hip. This is particularly important if your leg is swollen. The aim is to let gravity help to pull fluid and blood in the right direction - towards the heart. This reduces swelling in the leg and reduces the pressure of blood in the leg veins.
Try to set 3 or 4 periods per day of about 30 minutes to lie down with your leg raised. For example, lie on a bed or sofa with your foot on a couple of pillows. However, do not spend all your time in bed or resting. For the rest of the time, keep as active as you can and do normal activities. If possible, regular walks are good but do not stand still for long periods.
When you sleep overnight, if possible, try to keep your leg raised. You can do this by putting some pillows under the bottom of the mattress. (It may not be possible to sleep like this if you have certain other medical problems or disabilities.)
Other treatments
In some people, other conditions such as anaemia, poor nutrition, swelling of the legs and other medical problems may mean that the skin has less chance of healing well. Other treatments may be needed to help heal a venous leg ulcer - for example:
Try to stop smoking if you are a smoker. The chemicals in cigarettes may interfere with the skin healing.
Antibiotic medicines are sometimes advised for short periods if the skin and tissues around the ulcer become infected.
Painkillers can be taken if the ulcer is painful.
Skin care. The skin around an ulcer is often inflamed or scaly. Your doctor or nurse may advise on a cream to reduce inflammation if necessary.
Dietary advice if your diet is not very good. Also, if you are overweight then losing weight may help. Obesity is a risk factor for developing venous leg ulcers.
Iron tablets or other treatments if you are anaemic.
Pentoxifylline improves blood circulation and you may be offered this medicine to promote healing of the ulcer.
Hyperbaric oxygen (oxygen delivered at high pressure) is sometimes used when facilities are available.
A skin graft may be advised for a large ulcer, or for one that does not heal well.
Surgery for varicose veins or other vein problems is advised in some cases. This may correct back pressure of blood pooling in the veins and allow an ulcer to heal.
The topical haemoglobin spray (Granulox®) is a medical device to be used in the treatment of chronic wounds, such as venous leg ulcers. It works by increasing the oxygen supply to the wound, to speed up the healing process. Granulox® is now available to specialist wound care teams in hospitals and in the community.
What is the outlook (prognosis)?
Back to contentsUp to 7 in 10 venous ulcers heal within 12 weeks if treated with compression bandaging which is reapplied every week or so. If compression is not used and an ordinary dressing or support (compression) stockings alone are used, the chance of healing is less.
Preventing a recurrence of venous skin ulcers
Back to contentsVenous leg ulcers commonly come back (recur) after they have healed. To prevent this, you should wear a support (compression) stocking during the daytime for at least five years after the ulcer has healed. This counteracts the raised pressure in the veins that causes venous leg ulcers.
You should get a new stocking about every six months as the elastic tends to go after a while. Special stockings (compression stockings) can be prescribed or bought at pharmacies. They come in different sizes - your pharmacist will advise. Compression stockings for the prevention of venous leg ulcers are usually below knee in length rather than thigh length.
There are different strengths (classes) of compression stockings - class 1, 2 and 3. The higher the class (class 3) the greater the compression. Ideally, wear class 3 stockings. However, some people find class 3 stockings too tight and uncomfortable but class 2 may be fine. It is still better to wear some sort of compression stocking than none at all.
Note: proper compression stockings used for medical purposes are different to the support stockings or tights sold in ordinary clothing shops.
A leg ulcer is much less likely to recur if you wear compression stockings regularly.
Sometimes surgery for varicose veins or other vein problems is advised after an ulcer has healed, in order to help prevent a recurrence.
Patient picks for Veins

Heart health and blood vessels
Superficial thrombophlebitis
Superficial thrombophlebitis is inflammation of a vein just under the skin, usually in the leg. A small blood clot also commonly forms in the vein, but is usually not serious. The condition usually settles and goes within 2-6 weeks. Treatments can ease pain or discomfort. Superficial thrombophlebitis is different to, and much less serious than, deep vein thrombosis (DVT). However, in a small number of cases, complications can occur with superficial thrombophlebitis, including extension of the blood clot further up the vein. If the clot extends to where the superficial and deep, larger veins join, a DVT can develop.
by Dr Toni Hazell, MRCGP

Heart health and blood vessels
Varicose veins
Studies suggest that varicose veins occur in 10-20 out of 100 men and 25-33 out of 100 women. Most people with varicose veins do not have an underlying disease. They often occur for no apparent reason, although they are associated with lifestyle factors in some cases. Varicose veins do not cause symptoms or complications in most cases, although some people find them unsightly. If treatment is advised, or wanted for cosmetic reasons, a procedure to seal them off is used. There are several procedures available: heat, lasers or chemicals injected into the veins. These methods have largely replaced the old-fashioned surgical methods such as stripping the veins out.
by Dr Colin Tidy, MRCGP
Further reading and references
- Bonkemeyer Millan S, Gan R, Townsend PE; Venous Ulcers: Diagnosis and Treatment. Am Fam Physician. 2019 Sep 1;100(5):298-305.
- Compression stockings; NICE CKS, May 2022 (UK access only)
- Norman G, Westby MJ, Rithalia AD, et al; Dressings and topical agents for treating venous leg ulcers. Cochrane Database Syst Rev. 2018 Jun 15;6(6):CD012583. doi: 10.1002/14651858.CD012583.pub2.
- Cullum N, Liu Z; Therapeutic ultrasound for venous leg ulcers. Cochrane Database Syst Rev. 2017 May 15;5(5):CD001180. doi: 10.1002/14651858.CD001180.pub4.
- Keohane C, Westby D, Nolan FC, et al; Hyperbaric Oxygen as an Adjunct in the Treatment of Venous Ulcers: A Systematic Review. Vasc Endovascular Surg. 2023 Mar 8:15385744231162924. doi: 10.1177/15385744231162924.
- Leg ulcer - venous; NICE CKS, July 2023 (UK access only)
Continue reading below
Article history
The information on this page is written and peer reviewed by qualified clinicians.
Next review due: 24 Sept 2028
26 Sept 2023 | Latest version

Ask, share, connect.
Browse discussions, ask questions, and share experiences across hundreds of health topics.

Feeling unwell?
Assess your symptoms online for free
Sign up to the Patient newsletter
Your weekly dose of clear, trustworthy health advice - written to help you feel informed, confident and in control.
By subscribing you accept our Privacy Policy. You can unsubscribe at any time. We never sell your data.