Temporomandibular Joint Disorder (TMD)
Peer reviewed by Dr Toni Hazell, MRCGPLast updated by Dr Rosalyn Adleman, MRCGPLast updated 18 Nov 2024
Meets Patient’s editorial guidelines
- DownloadDownload
- Share
- Language
- Discussion
Temporomandibular disorders are problems affecting the jaw joint and the muscles and other tissues around the jaw joint. These disorders usually cause pain or reduced movement of the jaw, and sometimes sounds such as clicking or grating of the jaw joint. There are various causes but generally temporomandibular disorders are not serious and often improve with simple treatments.
In this article:
Continue reading below
What are temporomandibular disorders?
Temporomandibular disorders (TMDs) are problems which affect the jaw joint.
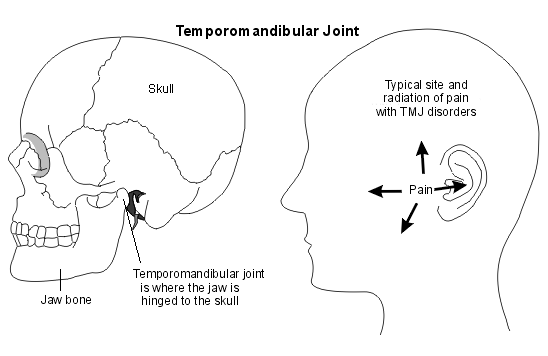
The jaw joint is located just in front of the ear, and it joins the jaw bone (mandible) to the skull near to the temple. The jaw joint is also called the 'temporomandibular joint'. Problems affecting this joint itself are usually known as TMJ disorders. However, there are various other causes of jaw pain and so the various conditions affecting the joint are now called 'temporomandibular disorders (TMDs)'.
TMJ dysfunction
Understanding the jaw joint
A joint is the place where two bones meet. Joints allow movement and flexibility between two bones. The jaw joint allows movement between the jawbone (mandible) and the skull. Muscles attached to the skull and jawbone cause the jawbone to move as the mouth is opened and closed.
Inside the jaw joint, there is a smooth material called cartilage, covering part of the bones. There is also a cartilage disc within the joint. The joint is lubricated by fluid called synovial fluid.
The muscles used for chewing (mastication) are mainly responsible for movement of the jaw.
Continue reading below
Symptoms of TMD
Pain in the joint area or nearby. The pain is usually located just in front of the ear and it may spread to the cheek, the ear itself and the temple.
Jaw movements may be reduced. This may be a general tight feeling or a sensation of the jaw getting stuck. Very rarely, the jaw may become 'locked', causing difficulty in opening or closing the mouth.
Clicks or noises can sometimes be heard coming from the jaw joint when you chew or move your mouth. These noises can be normal, so they are only relevant if you have other symptoms in the joint, such as pain or reduced movement.
Because the ear is very close to the jaw joint, some people develop ear symptoms such as:
Noise in the ear.
Sensitivity to sound.
Dizziness (vertigo).
TMD treatment
Most problems in the jaw joint can be helped with simple treatments such as painkillers and advice on how to rest the joint. If you think you have TMD see your dentist for advice. There are various treatments which are often used in combination:
Resting the jaw joint
At rest, try to keep your teeth slightly apart and your tongue resting in the bottom of your mouth.
You can rest the joint by eating soft food and not using chewing gum.
Also, avoid opening the mouth very wide - so don't do too much singing and try not to yawn too widely.
Massaging the muscles and applying warmth can help.
Improving posture can help - for instance, when sitting in front of a computer for a long time.
Other treatments are relaxation and stress-reducing therapies - presumably because people tend to clench their jaw when they are stressed, or because stress makes pain worse.
Splints or bite guards are sometimes suggested. These cover the teeth at night to reduce clenching of the jaw and can be made by dentists. There is no definite evidence from research trials that they work but some people find them helpful.
Medication
Painkillers such as paracetamol, ibuprofen or codeine can help. If these are not enough, muscle relaxants or a small dose of a medicine called a tricyclic antidepressant or a medicine called gabapentin can give added pain relief.
Physiotherapy
Physiotherapy treatments, such as ultrasound and gentle jaw exercises, can be helpful.
Exercises for jaw pain:
Before you start, warm the jaw area up with a hot water bottle or wheatbag. This will help the muscles to move more easily.
Place your fingers on the front of your chin and try to move the lower jaw forward against the resistance of your fingers. Hold this position for a few seconds, then relax. Repeat three times.
Place your fingers under your chin and try to open your jaw against resistance. Hold this position for a few seconds, then relax. Repeat three times.
Place your fingers on one side of your lower jaw and try to move your lower jaw sideways against the resistance of your fingers. Hold this position for a few seconds, then relax. Repeat three times. Then do the same on the other side.
Place your fingers over the jaw joint and gently open your mouth as far as you can. Take care that your jaw opens straight and not to one side.
You can repeat these exercises several times a day until the symptoms ease.
Treatment of other conditions
If there is an underlying condition - for example, a type of arthritis which is contributing to the TMD - this may need treating in its own right.
Injections or surgery
An injection of a medicine called a steroid into the joint may help, when symptoms are due to inflammation in the joint.
If the jaw muscles are overactive to a severe degree (such as with a movement disorder), an injection of botulinum toxin (Botox®) can reduce symptoms. There is debate about how effective this treatment is.
Inserting a fibre-optic device (arthroscopy) can be used for some types of treatment or surgery to the joint.
For a very few patients, surgical repair of the joint may be suggested. Various operations can be done, depending on the individual situation.
Other treatments
Some other treatments have been tried and may be available in some areas. These treatments include kinesio taping and acupuncture.
Continue reading below
How common are temporomandibular disorders?
TMDs are fairly common. About 1 in 4 people have symptoms in the jaw joint at some time in their lives. Of these people, only about 1 in 20 consult a doctor for this problem.
What causes temporomandibular disorders?
In general, TMDs are thought to have a 'multifactorial' cause, meaning that there are usually a number of factors contributing to the cause. These factors can be grouped into two types:
Problems linked to the muscles working the joint.
Problems inside the joint itself.
The muscle problems are the most common type, particularly for younger people.
Problems with the muscles may be caused by:
Tension of the jaw muscles. This can occur if you clench your jaw a lot during sleep, which is quite common. Some people also clench their jaw during the day if they are feeling tense or anxious.
Overuse of the jaw muscles, such as habitually chewing gum, or biting nails.
Rarely, other conditions make the jaw muscles overactive. For example, there are some rare kinds of movement disorders (called orofacial dystonias) which cause excessive jaw clenching.
Increased sensitivity to pain. We don't know why this happens but it may be linked to stress, or to some other process which affects pain sensitivity. Some doctors call this type of problem a pain syndrome because the exact cause of the pain is not known.
Problems in the joint may be caused by:
Wear and tear to the inside of the joint - for example, wear and tear to the cartilage. Sometimes this is due to a type of arthritis called osteoarthritis. This problem tends to affect older rather than younger people.
Certain other types of arthritis. Arthritis means inflammation in a joint. There are different kinds of arthritis. For example, rheumatoid arthritis and gout are both types of arthritis which may affect various joints in the body and they can sometimes affect the jaw joint.
Injury to the TMJ or to its cartilage disc can cause TMJ pain.
How are temporomandibular disorders diagnosed?
Often, the diagnosis is made on the basis of your symptoms and a dentist or doctor's examination. In many cases, no tests are necessary if you are healthy and have symptoms that are typical of a TMD. if your symptoms don't settle with simple advice and treatment then you may be referred to specialist for tests and further treatment. Possible tests are:
Blood tests which may be helpful to look for signs of inflammation, or to rule out other causes of pain in that area.
X-rays may be used to assess your teeth and to look for any fractures, joint dislocations, or severe wear and tear (degeneration) of the jaw joint.
An MRI scan or CT scan can be used to give a detailed picture of the joint.
Use of a fibre-optic device (arthroscopy) to look inside the joint. This may be used if other tests do not show the cause of the pain.
What is the outlook (prognosis)?
Generally the outlook is good. Most TMDs improve over time and do not become worse. It is very rare to have any complications with this condition. Some people do have symptoms that last longer or come back (recur). However, even these can usually be improved with the treatments described above. Most people do not need injections or surgery and will get better with simple treatments and time.
Patient picks for Joint problems

Bones, joints and muscles
Joint pain
There are many causes of joint pain. The different causes result in differing symptoms, treatments and outcomes. Most causes of joint pain resolve without any long-term problems. However, some require treatment for a long time and cause long-term joint problems as well as problems elsewhere in the body. This leaflet summarises the most common causes of joint pain, and discusses when you should seek help if you have joint pain. There are links to many of the specific conditions which cause joint pain.
by Dr Toni Hazell, MRCGP

Bones, joints and muscles
Hip problems
Hip problems are pretty common. The cause may be obvious, like an injury that comes on suddenly while playing sports. Sometimes the cause is not as clear and you will need to be checked out by a doctor or physiotherapist.
by Dr Rachel Hudson, MRCGP
Further reading and references
- Buescher JJ; Temporomandibular joint disorders. Am Fam Physician. 2007 Nov 15;76(10):1477-82.
- Coskun Benlidayi I, Salimov F, Kurkcu M, et al; Kinesio Taping for temporomandibular disorders: Single-blind, randomized, controlled trial of effectiveness. J Back Musculoskelet Rehabil. 2016 Feb 19.
- Pihut M, Ferendiuk E, Szewczyk M, et al; The efficiency of botulinum toxin type A for the treatment of masseter muscle pain in patients with temporomandibular joint dysfunction and tension-type headache. J Headache Pain. 2016 Dec;17(1):29. doi: 10.1186/s10194-016-0621-1. Epub 2016 Mar 24.
- Temporomandibular disorders (TMDs); NICE CKS, May 2024 (UK access only)
- Ghurye S, McMillan R; Orofacial pain - an update on diagnosis and management. Br Dent J. 2017 Dec;223(9):639-647. doi: 10.1038/sj.bdj.2017.879. Epub 2017 Oct 27.
Continue reading below
Article history
The information on this page is written and peer reviewed by qualified clinicians.
Next review due: 17 Nov 2027
18 Nov 2024 | Latest version

Ask, share, connect.
Browse discussions, ask questions, and share experiences across hundreds of health topics.

Feeling unwell?
Assess your symptoms online for free
Sign up to the Patient newsletter
Your weekly dose of clear, trustworthy health advice - written to help you feel informed, confident and in control.
By subscribing you accept our Privacy Policy. You can unsubscribe at any time. We never sell your data.