Jaundice
Peer reviewed by Dr Toni Hazell, MRCGPLast updated by Dr Philippa Vincent, MRCGPLast updated 24 May 2023
Meets Patient’s editorial guidelines
- DownloadDownload
- Share
- Language
- Discussion
In this series:Liver function testsGilbert's syndromeCirrhosisLiver failurePrimary biliary cholangitisWilson's disease
Jaundice means that the skin and other body parts turn a yellow colour. It is vital to diagnose the cause of jaundice and therefore important to always seek medical help. Jaundice treatment and outlook (prognosis) depends on the cause.
In this article:
Video picks for Other signs and symptoms
Continue reading below
What is jaundice?
Liver function
Jaundice is due to a build-up of a chemical called bilirubin in the tissues of the body. Bilirubin is a normal body chemical but can build up to abnormally high levels in various diseases.
Jaundice: yellowish pigmentation of the sclera

© Sheila J Toro, CC BY 4.0, via Wikimedia Commons
By Sheila J Toro, CC BY 4.0, via Wikimedia Commons
Causes of Jaundice
Back to contentsIt is useful to divide the causes of jaundice into four general areas:
Conditions affecting the red blood cells.
Conditions affecting the liver cells.
Conditions affecting the tiny bile ducts within the liver.
Conditions affecting the common bile duct outside the liver.
Conditions affecting the red blood cells
Various conditions cause an increased rate of breakdown of red blood cells. As a result, there is more bilirubin made than usual (most bilirubin is made from the breakdown of haemoglobin within red blood cells) which then circulates in the blood. The liver cells are unable to keep pace in processing the extra bilirubin. Therefore, a backlog of bilirubin builds up in the blood awaiting the liver cells to process it. This increased amount of bilirubin then spills into the tissues of the body to cause jaundice.
Conditions that cause an increased rate of breakdown of red blood cells include:
Some genetic diseases, such as sickle cell anaemia, thalassaemia, spherocytosis, and glucose 6-phosphate dehydrogenase deficiency. Genetic means that the condition is passed on through families through special codes inside cells called genes.
Haemolytic uraemic syndrome.
Conditions affecting the liver cells
There are many conditions that affect the liver cells.
In some conditions the liver cells are unable to take in the bilirubin very well, so bilirubin builds up in the bloodstream.
Sometimes there is a problem with the chemicals (enzymes) within the liver cells that process the bilirubin.
Sometimes there is a problem in the way the liver cells pass out the processed bilirubin into the bile ducts.
Sometimes, the liver cells are just damaged and all processes of the cell do not work well, or there are a reduced number of liver cells that are working.
With these problems, bilirubin may spill into the bloodstream to cause jaundice.
Conditions affecting liver cells that may cause jaundice include:
Hepatitis. This means inflammation of the liver. There are many causes, such as:
Infection with one of the hepatitis viruses.
Some infections with germs (bacterial infections).
Alcoholic hepatitis.
Autoimmune hepatitis.
Inflammation caused by poisons or as a side-effect of some medicines.
Cirrhosis. This is a condition where normal liver tissue is replaced by scar tissue (fibrosis). It tends to progress slowly and often does not cause symptoms in its early stages. However, as the function of the liver gradually becomes worse, serious problems can develop and jaundice may occur.
Inherited (hereditary) defects in the enzymes that process bilirubin in liver cells. These include Gilbert's syndrome, Dubin-Johnson syndrome, Crigler-Najjar syndrome and Rotor's syndrome.
Gilbert's syndrome is very common, affecting about 1 in 20 people. It typically causes only very mild jaundice from time to time (often this cannot be seen and is picked up routinely on blood tests), usually during a viral illness. The other hereditary defects are rare.
Conditions affecting the tiny bile ducts
If the tiny bile ducts within the liver become damaged or narrowed then the flow of bile is restricted. A backlog of bile (which contains bilirubin) then spills into the bloodstream. Various conditions can affect or damage the bile ducts in this way, for example, primary biliary cirrhosis or primary sclerosing cholangitis. It can also occur as a side-effect of some medicines.
Conditions affecting the common bile duct
The bile from all the tiny bile ducts in the liver drains into the common bile duct. If the common bile duct becomes narrowed or blocked (obstructed) then bile (which contains bilirubin) can seep out into the bloodstream and cause jaundice. This is sometimes called obstructive jaundice or posthepatic jaundice (hepatic is another word for liver). Conditions that can cause obstructive jaundice include:
Gallstones. These occur when bile, which is normally fluid, forms stones. Most gallstones form in the gallbladder and do not cause any problem. Jaundice is an uncommon complication of gallstones. It occurs if a gallstone comes out of the gallbladder but gets stuck in the common bile duct. Bile then cannot pass into the gut and so seeps into the bloodstream. See the separate leaflet called Gallstones and Bile for more details.
Pancreatic cancer in the head of the pancreas, which can block the flow of bile. See the separate leaflet called Pancreatic Cancer for more details.
Inflammation of the pancreas (pancreatitis). This can cause swelling of the pancreas, which may block the flow of bile. See the separate leaflets called Acute Pancreatitis and Chronic Pancreatitis for more details.
Biliary atresia. In this condition, part or all of the bile ducts become inflamed. This then leads to scarring (fibrosis) and narrowing and blockage of the bile ducts. The cause is not clear.
Cancer of the gallbladder. This may grow to block the common bile duct.
Continue reading below
The cause of jaundice - understanding bilirubin
Back to contentsThere are millions of red blood cells in the bloodstream. Each blood cell lasts for about 120 days and is then broken down by cells in the body into various waste chemicals. (New red blood cells are being made all the time to replace the ones being broken down.) Bilirubin is one of the chemicals that comes from the broken-down red cells.
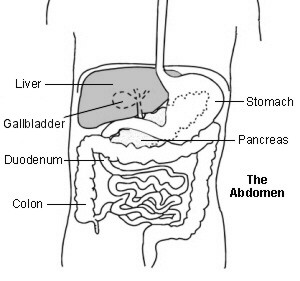
Upper abdomen showing bile ducts
Bilirubin is carried around the bloodstream in blood vessels. As the blood flows through the liver, the liver cells take up the bilirubin. Chemicals in the liver cells slightly alter the structure of the bilirubin to make it water-soluble. This water-soluble bilirubin is called conjugated bilirubin. (The bilirubin in the blood before being taken up by liver cells is called unconjugated bilirubin.)
The liver cells pass out the conjugated bilirubin into tiny tubes called bile ducts. The bilirubin is therefore now part of bile. Bile is a mix of various waste chemicals passed out by the liver cells. (One function of liver cells is to get rid of a range of waste chemicals into bile.)
There is a network of bile ducts in the liver. They join together (like branches of a tree) to form the larger common bile duct. Bile constantly drips down the tiny bile ducts, into the common bile duct and into the first part of the gut (small intestine), known as the duodenum.
The gallbladder lies under the liver. It is like a pouch off the common bile duct, which stores bile. The gallbladder squeezes (contracts) when we eat. This empties the stored bile back into the common bile duct and out into the duodenum. The bilirubin in the bile gives the stools (faeces) their typical brown colour.
Getting rid of bilirubin is a normal process. It is when abnormal amounts of bilirubin build up in the blood that you jaundice occurs.
Jaundice symptoms
Back to contentsThe whites of the eyes are often the first tissues that can be noticed turning yellow when jaundice develops. If the bilirubin level is only mildly high then this might be the only part of the body where a yellow colour is detected. With higher levels of bilirubin, the skin also becomes yellow.
Other symptoms associated with jaundice will depend on the cause but may include one or more of the following:
Tummy (abdominal) pain.
Weight loss.
Being sick (vomiting).
Pale stools (faeces).
Dark urine.
Continue reading below
Testing for jaundice
Back to contentsIf you become jaundiced you should see your doctor. As discussed above, there are various causes. Some are more common than others and some are more serious than others.
It is vital to obtain the correct diagnosis as the treatment and outlook (prognosis) can vary greatly, depending on the cause of jaundice. Sometimes, finding the cause can be a bit of a detective process and is not always easy or straightforward.
Your doctor is likely to ask various questions if you become jaundiced. He or she will also examine you. On the basis of this assessment, the possible causes may become clear, as certain symptoms and signs are associated with some causes of jaundice and not with others.
However, tests are usually needed to confirm an exact diagnosis of jaundice:
Various blood tests are usually done:
These will show whether the raised level of bilirubin is unconjugated or conjugated (as discussed earlier). This can help to narrow down the possible causes of jaundice.
Blood tests, called liver function tests, can also measure various liver enzymes which help to show if the liver is inflamed or working well.
Blood tests can also detect certain viruses or markers of other infections that can affect the liver.
Various other more detailed blood tests may be needed.
Urine tests may help to show if the levels of various chemicals in the blood are raised. This can help to narrow down the possible causes of jaundice.
An ultrasound scan of the liver, common bile duct and pancreas may identify a cause. In particular, it can often identify the cause of any blockage to the common bile duct. For example, a gallstone or cancer of the pancreas.
A magnetic resonance imaging (MRI) scan of the liver may be useful.
Taking a sample of the liver (a liver biopsy). This is taken to look at under the microscope.
Other more complex tests may be needed if the diagnosis is still in doubt.
Sometimes someone with jaundice will be admitted to hospital for tests; on other occasions, it is safe to carry out tests in the community to determine the underlying cause of the jaundice.
Jaundice in newborn babies
Back to contentsJaundice in newborn babies can be divided up into common simple (physiological) jaundice and other causes. It is often not serious but some cases are serious and need further tests and treatment. A midwife should usually be able to advise about jaundice in babies.
Physiological jaundice
It is common for newborn babies to develop mild jaundice when they are 2-3 days old. It is due to a mild increase in the breakdown of red blood cells combined with a liver that is not quite fully functioning. The liver soon matures and the jaundice begins to disappear towards the end of the first week and has gone by day 10. The baby is well and has no other problems.
Other causes of jaundice
The are various other causes of jaundice in newborn babies. Some can be due to serious disease of the blood or liver or to other problems. As a rule, the jaundice is not likely to be physiological jaundice if the baby is unwell and/or the jaundice is present in the first 24 hours after birth or lasts for more than 10 days. Therefore, if a baby is unwell or the jaundice is persisting past 10 days, medical advice should be sought. Kernicterus is a very rare but serious complication of jaundice in babies where brain damage can occur due to high levels of bilirubin in the blood.
See the separate leaflet called Neonatal Jaundice for more information.
Treatment of Jaundice
Back to contentsThere is no specific treatment for jaundice in children and adults. Treatment depends on the cause. See individual leaflets on the various diseases that can cause jaundice, including:
Patient picks for Other signs and symptoms

Signs and symptoms
Chronic pain
Chronic pain (also called long-term pain or persistent pain) is pain that lasts for more than three months. Pain can be caused by (secondary to) an underlying condition (such as osteoarthritis, rheumatoid arthritis, ulcerative colitis, or endometriosis). Chronic pain can also be primary. Chronic primary pain has no obvious underlying condition, or the pain appears to be much worse than any observable injury or disease.
by Dr Hayley Willacy, FRCGP
Signs and symptoms
Itchy bottom
An itchy bottom (pruritus ani) is a persistent itch around the anus. There are many different causes, like haemorrhoids, skin conditions, or infections. Treatments depend on the cause, but include hygiene measures and creams or ointments to treat the itching.
by Dr Doug McKechnie, MRCGP
Further reading and references
- Jaundice in newborn babies under 28 days; NICE Clinical Guideline (May 2010 - last updated October 2023)
- Bassari R, Koea JB; Jaundice associated pruritis: a review of pathophysiology and treatment. World J Gastroenterol. 2015 Feb 7;21(5):1404-13. doi: 10.3748/wjg.v21.i5.1404.
- Fargo MV, Grogan SP, Saguil A; Evaluation of Jaundice in Adults. Am Fam Physician. 2017 Feb 1;95(3):164-168.
- Jaundice in Adults; NICE CKS, November 2020 (UK access only)
Continue reading below
Article history
The information on this page is written and peer reviewed by qualified clinicians.
Next review due: 12 May 2028
24 May 2023 | Latest version

Ask, share, connect.
Browse discussions, ask questions, and share experiences across hundreds of health topics.

Feeling unwell?
Assess your symptoms online for free
Sign up to the Patient newsletter
Your weekly dose of clear, trustworthy health advice - written to help you feel informed, confident and in control.
By subscribing you accept our Privacy Policy. You can unsubscribe at any time. We never sell your data.