Eye floaters, flashes and haloes
Peer reviewed by Dr Colin Tidy, MRCGPLast updated by Dr Philippa Vincent, MRCGPLast updated 2 Jul 2024
Meets Patient’s editorial guidelines
- DownloadDownload
- Share
- Language
- Discussion
In this series:Visual problemsMacular degenerationRetinal vein occlusionVitreous haemorrhageGiant Cell ArteritisSquint in children
Eye floaters and flashes are common and are usually nothing to worry about. They usually occur because of normal changes that happen in the jelly-like substance inside the eye (vitreous humour) as you age.
Haloes are bright circles around a source of light. They are also referred to as glare. They are a common symptom, particularly in older people. They can sometimes be a sign of underlying eye conditions such as glaucoma.
In this article:
Video picks for Eye conditions
Key points
Eye flashes are brief bursts of light, eye floaters are small moving specks or lines in your vision, and haloes are bright circles around lights. They are all common visual disturbances that many people experience.
These usually happen due to the gel inside your eye (the vitreous) shrinking or pulling away from the retina. It is a natural part of ageing and usually nothing to worry about.
Seek medical help right away if you suddenly see lots more floaters, flashes, or a curtain-like shadow in your vision, as it could be a sign of a more serious condition like retinal detachment.
Continue reading below
What are eye floaters?
Floaters are shapes (opacities) floating in the field of vision and usually have the following qualities:
They may look like spots, threads, spiders or cobwebs.
They move as you move your eye and can seem to dart away when you try to look at them.
They drift about inside the eye rather than staying still.
They tend to be more obvious when bright objects, such as a blue sky, are being viewed.
What causes eye floaters?
Most floaters are also caused by changes in the vitreous humour. Most commonly this is due to normal ageing of the eye, when opacities form in the clear jelly and drift around. These kinds of floater are not associated with eye flashes or reduction in your vision and they tend to come on gradually.
They also tend to 'settle' at the bottom of the eye, below the line of sight. After a while they become less noticeable. They are more common in those who are short-sighted, those who have had eye surgery and those who have diabetic eye disease.
Floaters can also occur after posterior vitreous detachment. In this case there will be a sudden obvious increase in the number of floaters. Eye flashes may also occur. Again, there should be no loss of vision and most cases settle without causing any problems.
Bleeding into the vitreous humour (vitreous haemorrhage) will also lead to the formation of floaters. However, in this case the floaters represent blood in the jelly. If the bleeding is major then vision may be affected. For more information on this condition see the separate leaflet called Vitreous haemorrhage.
Floaters can also result from any internal damage to the back of the eye. Retinal tears and retinal detachments also cause floaters, and these will vary with severity, depending on the severity of the damage.
Less common causes of floaters include inflammation of the eye (posterior uveitis) and, more rarely still, tumours affecting the eye.
Are eye floaters dangerous?
Back to contentsFloaters are usually not serious. However, you should see an optician, or visit the A&E department, if any of the following apply:
They come on suddenly.
There are large quantities of them.
They are particularly disturbing.
They are associated with other eye symptoms such as pain, severe headaches, changes in vision, grey shadows in the vision or with new onset of eye flashes.
You have previously experienced retinal detachment, have had recent eye injury or eye surgery, have other eye conditions affecting the retina, or you have very high short-sightedness (myopia).
You already have vision in only one eye because of a prior condition, and you experience any new symptoms in your vision.
Continue reading below
What are eye flashes?
Back to contentsEye flashes are unexplained brief flashing lights in the eyes; they can be seen in one or both eyes. They often occur on the edges of vision and they are fairly common. Each flash, which can vary from a sparkle to a bright light, lasts a varying length of time. Periods of flashing can go on for several months. The symptoms are often most noticeable when going from a light to a dark room.
What causes eye flashes?
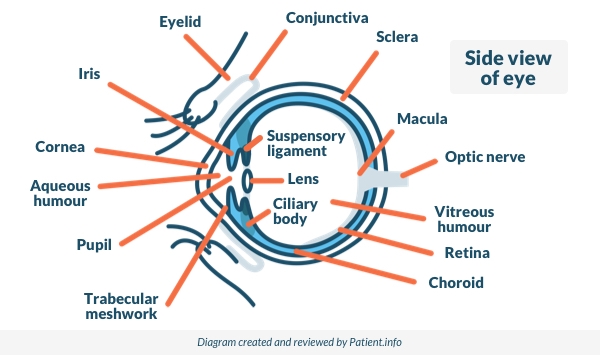
Back to contentsEye flashes are most commonly due to age-related changes in the vitreous humour. The vitreous humour is the jelly-like substance which fills the inside of the eye, between the lens and the retina. The vitreous humour is contained in a fine membrane and this is attached to the retina at the back and the lens at the front.
Side View of the Eye
Age
As we age, the vitreous humour (or vitreous gel) shrinks and as it does so it can pull on the retina. This can cause eye flashes because the pulling triggers nerves in the retina and they send signals to the seeing nerve (optic nerve).
Eventually the vitreous membrane tends to pull right off the retina, a condition called posterior vitreous detachment. This condition is harmless in itself, and in fact it happens to almost everyone eventually. The vitreous is detached from the retina in 75% of people aged over 65 and this is usually harmless.
Vitreous detachment
The flashes of vitreous detachment may occur in one or both eyes. If they occur in both eyes this is because the same thing is happening in each eye separately (but since the eyes are usually very similar this can occur at the same time).
Sometimes, as the vitreous pulls on the retina, it can tear it, causing a retinal tear or a retinal detachment. However, most vitreous detachment does not harm the retina.
Eye conditions
Conditions which affect the retina may also cause eye flashes. These include diabetic eye disease and sickle cell disease. Again, these can affect one or both eyes.
Migraines
Eye flashes can also relate to migraines. Some people with migraine experience flashing lights. Usually, in migraine, these occur in both eyes simultaneously. They can last up to an hour and tend to increase to a maximum before fading away and being replaced by a headache, which is typically one-sided and which may or may not be severe.
Charles Bonnet syndrome
Charles Bonnet syndrome is a condition experienced by people, usually elderly people, whose vision is deteriorating. The brain, deprived of real visual information, can "make things up" instead, particularly in conditions of low light. Patients may sometimes see flashes, although more frequently they see complex visual images like children or animals, which can look very real.
Continue reading below
Are flashes in the eyes serious?
Back to contentsMost eye flashes are caused by changes in the vitreous humour which are related to age and which are harmless. Occasionally flashes can be a sign that the retina is at risk of being torn or detached.
Increasing, persistent or constant flashes all suggest strong pulling on the retina and may mean that there is a risk of retinal damage. Flashes accompanied by a shadow coming down over the vision is suggestive of retinal detachment.
For further detail see the separate leaflet called Retinal detachment. Retinal detachment can lead to permanent vision loss.
Some people are at greater risk of retinal detachment than others, including:
Those who have already had a retinal detachment in the other eye.
Those with inflammatory eye disorders such as uveitis, or degenerative conditions of the retina.
Those who have had significant eye trauma or surgery.
Those with a family history of retinal detachment.
People who are extremely short-sighted (correction more than -6.00 ) are at higher risk, as the globe of their eye tends to be longer so that the vitreous is more likely to pull away.
What are eye haloes?
Back to contentsHaloes are rainbow-like coloured rings around lights or bright objects. They usually occur because there is extra water in the layers of the eye. The most common and important cause of this is acute glaucoma.
Glaucoma is a condition where there is increased pressure in the eye. Acute glaucoma is a very painful condition which can threaten sight if not treated promptly. However, another cause - chronic glaucoma - comes on more gradually and is not painful.
Many other conditions can lead to the experience of haloes. These include watering or tearful eyes, overuse of contact lenses, cataracts and opacities in the vitreous humour. Some prescribed medicines may also cause people to see haloes, including digoxin and chloroquine.
Are eye haloes serious?
Back to contentsBecause haloes can be a sign of increased pressure in the eye (glaucoma) then it is important to see an optician if persistent haloes develop. It is also important not to drive in conditions where haloes may affect the vision - for example, when driving at night.
If you have any doubts about your fitness to drive it is your responsibility to speak to the DVLA, who will advise you.
Who develops eye floaters, flashes and haloes?
Back to contentsMost people will notice occasional floaters, as there are often small opacities and crystals in the vitreous. Because more marked floaters, together with eye flashes and haloes, are mostly caused by conditions occurring naturally in older eyes, most people who experience frequent floaters are over 60 years of age.
Children and young adults may also experience eye flashes, floaters and haloes, particularly if there has been trauma or surgery to the eye or if they have other existing eye disease. These might include inflammatory conditions of the eye like uveitis, and conditions which can affect the retina like sickle cell disease and the form of retinopathy that can affect very premature babies.
When should I worry about eye floaters, flashes or haloes?
Back to contentsUrgent medical advice should be sought if eye floaters and flashes are very marked or sudden in onset. Urgent advice should also be sought if they are associated with pain, changes in the vision, or if both floaters and flashes are occurring together. Optician advice should also be obtained if persistent haloes develop.
People who have previously lost the sight in one eye should seek advice for any new symptoms, even if less severe.
Most opticians are able to check the pressures in the eyes in order to rule out glaucoma. They also have equipment to allow them to perform detailed eye exams to look for damage to the retina. This equipment (called a slit lamp) is also available in A&E departments. Most GPs do not have slit lamps and will redirect to A and E or the optician depending on the urgency required.
Frequently asked questions
Back to contentsWhat is the treatment for eye flashes?
Treatment for eye flashes depends on the cause. If they’re due to age-related changes in the eye, no treatment may be needed, but sudden or severe flashes should be checked urgently to rule out retinal problems that may require surgery or laser treatment.
Will eye flashes go away?
Eye flashes often fade over time as the jelly-like substance inside the eye (the vitreous) settles. However, if they suddenly appear or worsen, it’s important to get your eyes checked.
How to get rid of haloes in eyes?
The treatment of haloes depends on what's causing them but usually involves using prescribed eye drops, updating your glasses, or treating the underlying cause.
Are eye floaters normal?
Yes, eye floaters are normal and usually harmless, especially as you get older. They happen when tiny fibres in the eye cast shadows on the retina.
Can eye floaters happen in both eyes at the same time?
Yes, eye floaters can appear in both eyes at the same time, however, if you notice new or sudden floaters in either eye, it’s best to get your eyes checked to rule out any underlying problems.
Can you prevent eye floaters?
There’s no guaranteed way to prevent eye floaters, as they’re usually a natural part of ageing. However, protecting your eyes from UV light, managing conditions like diabetes, and having regular eye checks can help keep your eyes healthy and reduce your risk of developing them.
Dr Mary Lowth is an author or the original author of this leaflet.
Patient picks for Eye conditions

Eye health
Episcleritis and scleritis
Episcleritis and scleritis are inflammatory conditions which affect the eye. Both cause redness, but scleritis is much more serious (and rarer) than episcleritis.
by Dr Doug McKechnie, MRCGP

Eye health
Astigmatism
Astigmatism is a common eye condition that affects the shape of the cornea or the lens of the eye. The cornea and lens are typically smooth and round in shape, but in people with astigmatism, they are irregularly shaped. The main symptom of astigmatism is blurred vision. It occurs because the cornea at the front of the eye is unevenly curved. Vision problems, such as astigmatism, are also known as refractive errors. Astigmatism is a common condition that can be corrected by glasses or contact lenses, or cured with laser eye surgery.
by Dr Doug McKechnie, MRCGP
Further reading and references
- Posterior vitreous detachment; Royal National Institute of Blind People (RNIB)
- Khan AA, Kelly RJ, Carrim ZI; Flashes, floaters, and a field defect. BMJ. 2013 Nov 4;347:f6496. doi: 10.1136/bmj.f6496.
- Bergstrom R, Czyz CN; Vitreous Floaters.
Continue reading below
Article history
The information on this page is written and peer reviewed by qualified clinicians.
Next review due: 1 Jul 2027
2 Jul 2024 | Latest version

Ask, share, connect.
Browse discussions, ask questions, and share experiences across hundreds of health topics.

Feeling unwell?
Assess your symptoms online for free
Sign up to the Patient newsletter
Your weekly dose of clear, trustworthy health advice - written to help you feel informed, confident and in control.
By subscribing you accept our Privacy Policy. You can unsubscribe at any time. We never sell your data.