Legionnaires' disease
Peer reviewed by Dr Rosalyn Adleman, MRCGPLast updated by Dr Toni Hazell, MRCGPLast updated 6 Aug 2024
Meets Patient’s editorial guidelines
- DownloadDownload
- Share
- Language
- Discussion
- Audio Version
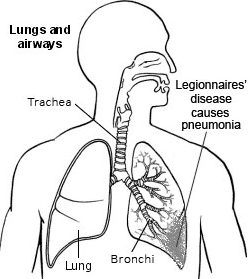
Legionnaires' disease is a serious lung infection (pneumonia) with chills, high temperature (fever) and muscle pains. You get the infection by breathing in droplets of water which contain legionella germs (bacteria) from contaminated water systems.
The earlier the illness is treated with antibiotic medication, the better the likely outcome. The illness is serious and can be fatal. However, it cannot be passed from person to person (it is not contagious). Pontiac fever is a milder illness caused by the same bacterium.
In this article:
Video picks for Chest and lung infections
Continue reading below
What is Legionnaires' disease?
Legionnaires' disease (also called legionellosis) is an uncommon infection caused by a germ (bacterium) called legionella. The name came about from a 1976 outbreak of lung infection (pneumonia) among American ex-servicemen (Legionnaires) who attended a conference. A new germ (bacterium) that had never been identified before was found to be the cause.
There are two types of illness which can develop after being infected with this bacterium:
Legionnaires' disease. This causes a lung infection (pneumonia). It is usually a severe illness which is sometimes fatal.
Pontiac fever. This occurs when the bacteria cause a flu-like illness. It is not usually serious.
What are the symptoms of Legionnaires' disease?
Back to contentsLungs and airways - Legionnaires' disease
The incubation period is the period of time between breathing in the germs (bacteria) and developing symptoms of the illness. This period is normally 2-10 days. However, it can be up to 2 weeks. On average, the incubation period is 3-6 days.
The usual first symptoms are:
Cough.
High temperature (fever).
Sweat.
Shivers.
Losing your appetite.
Feeling generally unwell.
Headaches.
Aches and pains.
Phlegm (sputum) may become yellow/green and is sometimes bloodstained.
Symptoms tend to become worse quite quickly as the infection spreads through the lung tissue. You may become breathless, breathe fast and develop a tight chest.
You may have pain in the side of the chest when breathing, worse when taking a deep breath. (This is called pleuritic chest pain and is probably due to the surface of the lung becoming inflamed.) These are typical symptoms of the lung infection pneumonia. See separate leaflet called Pneumonia for more details.
Other symptoms of Legionnaires' disease include:
Confusion.
A feeling of sickness (nausea).
Being sick (vomiting).
Diarrhoea.
About 3 in 10 people have symptoms that affect the gut (gastrointestinal tract).
Complications can develop and can cause heart, brain, kidney or blood problems.
Continue reading below
How do you get Legionnaires' disease?
Back to contentsInfected water
The source of the germs (bacteria) in an outbreak is usually a man-made water distribution system where the bacteria have multiplied in great numbers.
Warm storage tanks where the water stagnates are ideal for legionella bacteria to multiply. The bacteria thrive in water temperatures between 25°C and 45°C - about 35°C is the optimum temperature - particularly if the water is still and contains debris of any sort. They are killed by temperatures of 60°C and above.
This means that Legionnaires' disease can be caught from:
Piped water, especially hot water, in large buildings where long runs of pipe work can be a source of the bacteria.
Circulating water droplets in air-conditioning and cooling systems, cooling towers and evaporative condensers.
Whirlpool spas (jacuzzis), other warm-water baths and shower heads.
Decorative fountains.
Nebulisers and humidifiers (including some types of breathing equipment) if topped up with contaminated tap water.
Potting compost.
Plastics factories.
In all of the above it is particularly likely to breed if the temperature is right and the water is still.
You become infected with legionella by breathing in (inhaling) water droplets (aerosol) that are contaminated by many legionella bacteria.
An outbreak can affect many people in the same hospital, hotel, office complex or other large building, around the same time. However, they do not infect each other - they all acquire the disease from the same place.
It cannot be acquired by drinking infected water, only by inhaling droplets which allow the bacteria to reach the lungs directly.
Individual (sporadic) cases
Individual cases occur from time to time. Where only one person is infected then the source of the bacteria is often not found. There have been individual cases thought to have been caused by walking past offices with infected air-conditioning systems. About 2 in 100 cases of pneumonia that occur in previously well people are thought to be due to legionella bacteria.
Risk factors for developing Legionnaires' disease
Back to contentsAnyone can develop Legionnaires' disease. However, you are more likely to develop Legionnaires' disease (and pneumonia caused by other bacteria) if you are already in poor health.
Some long-term health conditions reduce your body's natural immune responses and ability to fight infection. This makes you more at risk of Legionnaires' disease, and more at risk of a serious illness if you contract Legionnaires' disease.
Conditions which lower your resistance in this way include:
Chronic lung disease. This includes asthma and especially chronic obstructive pulmonary disease (COPD).
Other long-term conditions affecting your major organs, such as chronic kidney disease and heart disease.
Alcohol or drug dependence.
Cancer - especially lung cancer or leukaemia.
Human immunodeficiency virus (HIV) infection or acquired immune deficiency syndrome (AIDs).
The effect of medicines which affect the immune system, including:
Long-term steroid medication.
Chemotherapy for cancer.
Immunosuppressant medication, such as azathioprine, mycophenolate, ciclosporin, tacrolimus, rituximab and interferon. Immunosuppressant medication is used in the treatment of:
Joint (rheumatological) conditions.
Inflammatory diseases such as Crohn's disease.
Organ transplants.
You are also more at risk of contracting Legionnaires' disease if you are a smoker and if you are aged over 50 years.
Continue reading below
How is Legionnaires' disease diagnosed?
Back to contentsX-ray
A chest X-ray can confirm that you have lung infection (pneumonia). However, pneumonia is common and there are many germs (bacteria) and other types of germs that can cause pneumonia. (Legionnaires' disease is an uncommon cause of pneumonia.)
Blood and phlegm tests
If Legionnaires' disease or other unusual causes of pneumonia are suspected, blood tests and phlegm (sputum) tests are then done to try to identify the bacterium or other germ that is causing the pneumonia. These include blood cultures in which laboratory scientists try to make the legionella bacteria grow and multiply, so that it can be identified under a microscope.
Other blood tests can look for antibodies against legionella bacteria. Antibodies are proteins made by the immune system, which fight infection.
Urine test
In addition, a urine test can confirm most (but not all) cases of legionella infection. The test, called the legionella urinary antigen test, detects a particular protein that is part of the legionella bacterium. These proteins can be found in the urine even several months after you have been treated for Legionnaires' disease.
Lumbar puncture
Sometimes a lumbar puncture (sometimes called a spinal tap) is performed to help diagnosis. Here, a sample of the fluid (cerebrospinal fluid, or CSF) which surrounds the spine, is removed from the lower back, using a needle and some local anaesthetic to numb the area.
This fluid flows around the brain and spinal cord to protect and nourish the nerve tissues. It can be tested to see if the legionella bacteria have infected the surface of the brain (causing legionella meningitis).
This test is generally only done if you have symptoms that suggest meningitis. See separate leaflet called Lumbar puncture for more details.
What is the treatment for Legionnaires' disease?
Back to contentsMost patients with Legionnaires' disease are admitted to hospital.
Antibiotics are started as soon as possible. Usually they are given intravenously (IV), which means into a vein, rather than by mouth (orally).
The usual antibiotic to treat Legionnaires' disease (or suspected Legionnaires' disease) is erythromycin. But other antibiotics are often used - for example, azithromycin, clarithromycin, doxycycline. Ciprofloxacin and levofloxacin antibiotics might be used if there is no alternative, but should not be the first choice due to concerns about side-effects. Sometimes a combination of antibiotics is used, especially if it is not yet certain whether the infection is due to legionella or to other germs (bacteria). Treatment with antibiotics lasts from a week to three weeks, depending on how unwell you are and how quickly you recover.
Oxygen is commonly given. This is because pneumonia inflames the lungs and makes them work less well. This can cause oxygen levels to drop. Breathing in extra oxygen makes it easier for the lungs to do their job.
IV fluids are often given to keep you well hydrated. If you are very unwell, especially with a breathing problem such as lung infection (pneumonia), you are likely to be unable to drink enough fluids.
Intensive care with supportive treatments, such as assisted ventilation, may be needed if the pneumonia is severe. Assisted ventilation is used to support breathing temporarily when the effort needed to breath effectively with infected lungs becomes too tiring. When this happens oxygen levels may fall, even if you are breathing in added oxygen through a mask.
What is the outlook (prognosis)?
Back to contentsLegionnaires' disease is a serious illness. Even if you were previously fit and well, you have about a 1 in 10 chance of dying if you get Legionnaires' disease. If you were previously unwell, (for example, if you already have a lung disorder) then you have a higher risk of dying if you have Legionnaires' disease.
Possible complications of Legionnaires' disease include:
Respiratory failure. This means the lung infection (pneumonia) has affected the lungs to such a degree that they cannot supply your body with oxygen without added help. In these situations you will need help with breathing, and supplemental oxygen. You might need to be treated in a high-dependency or intensive care unit. It is possible that you might need to be put to sleep (anaesthetised) and have a breathing tube inserted (be intubated), to help you through the worst period.
Acute kidney injury. Severe infection can stop the kidneys from working. The kidneys usually filter and clean the blood. When there is renal failure, there is a toxic build-up of waste products in the blood. During an acute infection, the blood can be cleaned constantly by flowing through a haemofiltration machine which does the kidneys' job for you.
Severe sepsis (overwhelming infection) leading to shock. In severe cases infection can overwhelm the body and affect all parts of it, causing several organs to fail. Sepsis can also affect the blood clotting, leading to bleeding, and it makes the blood pressure fall. Severe sepsis and septic shock are dangerous conditions with a high risk of fatality.
The outlook for Legionnaires' disease is best if the illness is diagnosed as early as possible, and you are treated with antibiotics immediately.
After recovery from Legionnaires' disease, you may get symptoms such as tiredness, poor concentration, cough or mild shortness of breath. These may take several months to settle.
What is Pontiac fever?
Back to contentsPontiac fever is a milder illness caused by legionella germs (bacteria). It causes a flu-like illness which lasts just a few days.
Symptoms of Pontiac fever
Back to contentsSymptoms include:
High temperature (fever).
Shivers.
Headache.
Muscle aches.
Tiredness.
A dry cough.
However, the infection does not affect the lungs and therefore does not cause pneumonia. Usually, no treatment is needed other than paracetamol or ibuprofen to ease fever and muscle aches.
It is not clear why some people infected with legionella bacteria get Legionnaires' disease (with pneumonia) and some people get the milder Pontiac fever.
It is also thought that some people who are infected with legionella bacteria do not become ill at all (a subclinical infection).
Can infection with legionella germs (bacteria) be prevented?
Back to contentsAs mentioned, the main cause of outbreaks of Legionnaires' disease is from contaminated water sources. In the UK, and in many other countries, there are regulations on how to maintain water supplies and air-conditioning systems used in large buildings.
This mainly involves keeping the water temperature at less than 20°C or more than 60°C. The water supply should also be kept clean and kept moving so that it doesn't stagnate. All of this reduces the chance of legionella bacteria breeding. However, it is very difficult to destroy (eradicate) this bacterium completely.
If you are an employer or a landlord, you have a legal duty to ensure all water systems in your premises are properly maintained.
If you have a home humidifier or spa, follow the manufacturer's advice about maintenance and cleaning.
About 3 in 10 cases of Legionnaires' disease diagnosed in the UK are contracted abroad, usually due to poorly maintained water storage and air-conditioning systems in hotels. Always mention any recent foreign travel if you are unwell and see your doctor.
At present, there is no vaccine that can protect against legionella bacteria.
Dr Mary Lowth is an author or the original author of this leaflet.
Patient picks for Chest and lung infections

Chest and lungs
Chest infection
A chest infection is an infection that affects your lower large airways (bronchi) and your lungs. Pneumonia and bronchitis are the most common chest infections. Bronchitis is usually caused by a viral infection, with between 1% and 10% of cases being caused by bacteria. Pneumonia is usually due to bacterial infection. Pneumonia may be serious and need hospital admission.
by Dr Colin Tidy, MRCGP

Chest and lungs
SARS and MERS virus
Severe acute respiratory syndrome (SARS) and Middle East respiratory syndrome (MERS) are viral infections. Both infections can cause very serious illnesses that particularly affect the lungs. SARS caused many infections, especially in Asia, in 2002-2004 but was not heard of for some time. A SARS-CoV-2 (COVID-19) outbreak emerged in Wuhan, China in December 2019. This spread rapidly and was declared a global pandemic in 2020. MERS was first recognised in the Middle East in 2012. Most of the initial infections were in the Middle East. However, by February 2018, the World Health Organization (WHO) had reported cases in many other countries.
by Dr Hayley Willacy, FRCGP
Further reading and references
- Legionnaires' disease: guidance, data and analysis; Public Health England
- Guidelines for the management of community acquired pneumonia in adults; British Thoracic Society (2009), Thorax Vol 64 Sup III
- Guidelines for the management of community acquired pneumonia in children; British Thoracic Society (2011), Thorax Vol 66 Sup 2
- UKHSA Legionnaires' disease: national surveillance scheme
- Fluoroquinolone antibiotics: must now only be prescribed when other commonly recommended antibiotics are inappropriate; Medicines & Healthcare products Regulatory Agency, GOV.UK (January 2024)
Continue reading below
Article history
The information on this page is written and peer reviewed by qualified clinicians.
Next review due: 5 Aug 2027
6 Aug 2024 | Latest version

Ask, share, connect.
Browse discussions, ask questions, and share experiences across hundreds of health topics.

Feeling unwell?
Assess your symptoms online for free
Sign up to the Patient newsletter
Your weekly dose of clear, trustworthy health advice - written to help you feel informed, confident and in control.
By subscribing you accept our Privacy Policy. You can unsubscribe at any time. We never sell your data.