Coeliac disease
Peer reviewed by Dr Krishna Vakharia, MRCGPLast updated by Dr Colin Tidy, MRCGPLast updated 24 May 2023
Meets Patient’s editorial guidelines
- DownloadDownload
- Share
- Language
- Discussion
In this series:Gastrointestinal malabsorptionDermatitis herpetiformis
Coeliac disease (also spelled celiac disease) mainly affects the part of the gut called the small intestine. It can occur at any age. Coeliac disease is caused by a reaction of the gut to gluten. (For this reason it is sometimes also called gluten-sensitive enteropathy). Gluten is part of certain foods - mainly foods made from wheat, barley and rye.
Various symptoms can develop including tummy (abdominal) pains, tiredness and weight loss. Symptoms go if you do not eat any foods that contain gluten.
In this article:
Continue reading below
What is coeliac disease?
Diagram naming the parts of the gut
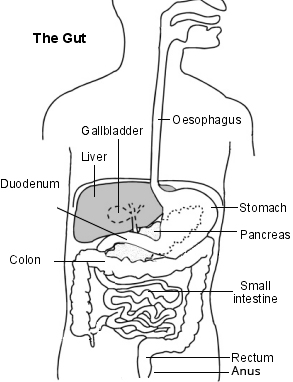
Coeliac disease is a condition that causes inflammation in the lining of part of the gut (the small intestine). The inflammation is triggered by eating foods that contain gluten.
Coeliac disease is not a food allergy or a food intolerance. It is an autoimmune disease. The immune system makes white blood cells (lymphocytes) and antibodies to protect against foreign objects such as bacteria, viruses and other germs.
In an autoimmune disease, the immune system mistakes part or parts of the body as foreign. Other autoimmune diseases include type 1 diabetes, rheumatoid arthritis and some thyroid disorders.
The lining of the small intestine contains millions of tiny tube-shaped structures called villi. These help food and nutrients to be digested more effectively into the body. But, in people with coeliac disease, the villi become flattened as a result of the inflammation. This means that food and nutrients are not so readily digested by the body.
Untreated coeliac disease can also affect other parts of the body, including the bones, the teeth and the brain and nervous system. Once it has developed, coeliac disease is a permanent condition.
How common is coeliac disease?
Coeliac disease affects about 1 in 100 people in the UK. However, many people with coeliac disease have not been diagnosed. It has been estimated that for every person diagnosed, 7-8 people remain undiagnosed.
Anyone, at any age, can develop coeliac disease. Although you aren't born with coeliac disease, it is a condition that used to be associated with young children.
However, it is now much more commonly diagnosed in adults. More than 7 in 10 people with coeliac disease are first diagnosed when aged over 20 years.
Continue reading below
Risk factors
Coeliac disease often runs in families. If you have a close family member who has coeliac disease (a brother, sister, parent or child) then you have a 1 in 10 chance of developing coeliac disease.
It is also more common in people who have other autoimmune diseases - for example:
And in some chromosome problems such as:
It is thought that there are about nine people with coeliac disease which has not been diagnosed (so they don't know that they have it), for every one person with it who knows that they have the disease.
Coeliac disease symptoms
The inflammation in the lining of the gut (small intestine) stops food from being properly absorbed. You then do not absorb nutrients very well into your body. A variety of symptoms may then develop, which may depend on how old you are and how long you have had the problem.
Symptoms in babies
Symptoms first develop soon after weaning when the baby starts eating solid foods containing gluten. Symptoms of coeliac disease in babies include:
The baby failing to grow or to gain weight.
Pale and bulky poo (faeces).
Smelly diarrhoea.
Swollen tummy (abdomen).
Being sick (vomiting).
Symptoms in older children
The symptoms of coeliac disease in older children may be similar to those in babies. Poor absorption of food may cause deficiencies of vitamins, iron and other nutrients. This may cause anaemia and other problems.
As the fat part of the diet is poorly absorbed, stools may be pale, smelly and difficult to flush away. Diarrhoea may develop. However, the symptoms may not be very typical or obvious. If the gut and bowel symptoms are only mild then the first thing that may be noticed is poor growth.
Delayed puberty can also be caused by untreated coeliac disease.
Symptoms in adults
Poor absorption of food may cause deficiencies of vitamins, iron and other nutrients and may make you feel tired and weak.
Common symptoms of coeliac disease in adults are:
Anaemia due to poor absorption of iron.
Abdominal pains which tend to come and go and excess wind, bloating and diarrhoea, which can be very similar to the symptoms of irritable bowel syndrome (IBS).
Mouth ulcers may occur and may keep coming back.
Weight loss due to poor absorption of food. However, most adults with coeliac disease do not lose weight and are not underweight.
Some people also report headaches, feeling anxious and aching joints.
Occasionally, an itchy, blistering skin condition called dermatitis herpetiformis can occur in some people with coeliac disease. You can read more about this in the separate leaflet called Dermatitis Herpetiformis.
If the common symptoms described above develop, the diagnosis may be made quickly. However, common or typical symptoms do not always develop. Particularly in adults, the areas affected in the gut may be patchy.
Symptoms may then be mild, or not typical, and it may be a while before the diagnosis is made. The average time from first symptoms to diagnosis is 13 years in the UK.
Some people with coeliac disease do not have any gut symptoms at all. They are tested either because they are at a higher risk than normal of developing it or because they have developed a condition that could be a complication of the disease, such as osteoporosis or gluten ataxia (see later).
Note: if, from your symptoms, you suspect that you may have coeliac disease, see a doctor. Do not treat yourself by going on a gluten-free diet without a confirmed diagnosis. If you do go on a gluten-free diet before the diagnosis is confirmed then any tests, including the gastroscopy and biopsy described later, may even give negative results. So, get it checked out first - and then treat it if it is confirmed.
Continue reading below
What causes coeliac disease?
The cause is a sensitivity to gluten but why this develops isn't understood. Gluten occurs in common foods including wheat, barley and rye, and any foods made from these such as bread, pasta and biscuits and also beer. Some people with coeliac disease are also sensitive to oats.
People with coeliac disease make antibodies against gluten. Antibodies are proteins in the immune system that normally attack bacteria, viruses and other germs. In effect, the gut mistakes gluten as harmful and reacts against it as if it were fighting off a germ.
These antibodies lead to inflammation developing in the lining of the small intestine. They may also be the cause of some of the problems that a person with coeliac disease can have in other parts of their body, such as the balance centre of the brain (cerebellum).
Coeliac disease can develop in babies. Older children or adults who have not previously had problems may also become gluten-sensitive at some point in their lives and develop coeliac disease. It is not known why the immune system of some people becomes sensitive to gluten. There is no evidence that stress or the use of antibiotics triggers coeliac disease.
Some people who do not have coeliac disease also avoid gluten in their diet. This is because they have found that foods containing gluten make them feel generally unwell, possibly with bloating and tummy pain. They are 'gluten intolerant' but they do not develop inflammation in their gut. Sometimes this is called non-coeliac gluten sensitivity.
Diagnosing coeliac disease
If coeliac disease is suspected, a blood test will be advised by your doctor. This is done to look for certain antibodies that are present in the blood of a person with coeliac disease. If they are present then more tests will be needed.
It is vital that you are eating a diet containing gluten (wheat, barley and/or rye) for at least six weeks before the blood test is performed. If you have been avoiding gluten this may lead to your symptoms coming back for a while but it will increase the chances of getting the diagnosis right.
If the blood test is positive then you may be referred to a specialist who may arrange for you to have a gastroscopy and for a biopsy to be taken. A gastroscopy is a way to look inside the stomach and the upper part of the gut with a thin flexible tube (endoscope).
A biopsy is a procedure in which a small sample of tissue is taken. For coeliac disease testing, the biopsy is taken from the inside lining of the beginning of the gut (duodenum) during the gastroscopy. The sample is looked at with a microscope to see if the typical changes of coeliac disease are present.
If your doctor suspects that your child might have coeliac disease it may be possible for them to be diagnosed without needing to have a gastroscopy, but this will depend on the results of several blood tests.
Other tests may be done to find out how much the poor absorption of food and nutrients has affected you. For example, blood tests for anaemia and for the levels of vitamins, iron, protein, etc.
You may also be advised to have a special bone scan (a DXA scan) to see if your bones have become affected due to poor absorption of calcium and vitamin D. You might also be advised to have a magnetic resonance imaging (MRI) scan of your brain, if you have problems with your balance or coordination.
Traditionally, the diagnosis of coeliac disease has been a two-stage process, involving blood tests and an endoscopy plus biopsy. However, non-essential endoscopies were paused during the coronavirus pandemic, creating a huge backlog of people waiting for diagnosis.
Current advice from the British Society of Gastroenterology about the tests needed to diagnose coeliac disease are as follows.
Your GP can do the initial blood tests but a specialist needs to take the decision as to whether you still require an endoscopy and biopsy. Therefore, you may not need a biopsy.
Not everyone will be suitable for the no-biopsy approach. To qualify you need to be under the age of 55 with symptoms of coeliac disease and:
You don't need an endoscopy to rule out other conditions.
You have antibody levels (IgA tissue transglutaminase) at least 10 times the upper limit of normal.
You have a second positive antibody blood test (endomysial antibodies (EMA) or tissue transglutaminase if EMA isn't available).
Most children have been diagnosed without biopsies since 2013.
Accurate diagnosis requires people to stay on a gluten-containing diet until the results are obtained. The new recommendations are a real boon, as they will shorten the time people with suspected coeliac disease have to wait for confirmation. This means they will be able to start a gluten-free diet earlier and avoid lengthy periods of illness.
Who else should be tested for coeliac disease?
Coeliac disease tends to be under-diagnosed. There are certain groups of people who are much more likely to have coeliac disease than others. They should have a test for coeliac disease even if they have no or few symptoms. This includes people with:
Close relatives (parent, child, brother/sister) of a person with coeliac disease.
Autoimmune conditions such as autoimmune thyroid disease, primary biliary cholangitis or Sjögren's syndrome.
There are also other conditions that are linked with coeliac disease and may sometimes be caused by it. If you have one of the following conditions, your medical professional may suggest that you have the tests done to look for coeliac disease:
Unexplained peripheral neuropathy, which could be gluten neuropathy.
Persistent, unexplained abnormal liver function tests.
Unexplained ataxia, that could be gluten ataxia. (Ataxia is a rare brain condition which causes problems with balance and coordinating your movements.)
Unexplained recurrent miscarriage or sub-fertility in women.
Dental enamel weakness, as diagnosed by a dentist.
Sponsored
Coeliac disease test
A Coeliac Disease home-test kit includes genetic testing to identify if you carry the HLA-DQ risk marker.
Find out if you are at risk with this at-home saliva collection kit.
Coeliac disease treatment
Gluten-free diet
The only treatment for coeliac disease is a lifelong, strictly gluten-free diet.
Once you stop eating any foods that contain gluten, the symptoms usually go within a few weeks. Although for some people it can take six months to a year.
The main foods to stop are any that contain wheat, barley or rye. Many common foods contain these ingredients, such as:
Breads.
Pasta.
Cakes.
Pastries.
Some cereals.
Foods made from gluten-free, uncontaminated (not mixed with other types of cereals) oats are usually safe to eat. However, a few people with coeliac disease have symptoms if they eat even uncontaminated oats. Fish, meat, vegetables (including potatoes), rice, maize, corn, fruit and dairy products are fine.
You should get advice from a dietician. Coeliac UK is a charity based in the UK which provides lots of useful advice about which foods are suitable (see 'Further reading' section below). You can buy special gluten-free foods such as flour, pasta, bread and other foods. These are available from health food shops, by mail order, and via the internet and, in the UK, some may be available on prescription.
There are many diet sheets with food alternatives and recipes. Unfortunately, many processed foods, ready-made meals and fast foods contain gluten. Food labels should now always say whether or not the food contains gluten. In the UK you can also look for the symbol of an ear of wheat with a line through it, which manufacturers use to show that a food is gluten-free.
Avoiding gluten is for life. If you eat gluten again, symptoms will return. Even small amounts of gluten can sensitise the gut (small intestine) again. To avoid symptoms and complications (see below), you must be strict about avoiding all foods that contain gluten.
The goals of treatment are to relieve your symptoms and to prevent complications but also to ensure that you enjoy a good quality of life; the many foods that are allowed are varied and interesting. For more details, see the leaflet called Coeliac disease diet sheet.
Other treatments
In addition to avoiding gluten, you may be advised to take some vitamin, calcium and iron supplements, at least for the first six months following diagnosis. This is to replace any deficiencies and also to make sure you get enough of these whilst the gut lining is returning to normal.
Having coeliac disease can cause your spleen to work less effectively, making you more vulnerable to infection from certain germs. If your spleen is working less effectively, you may need to have several immunisations, including:
The Hib vaccine - which protects against blood poisoning, pneumonia and Hib meningitis.
The pneumococcal vaccine - which protects against infections caused by the germ (bacterium) Streptococcus pneumoniae.
Note: there are several enzyme supplements available to buy that claim to break down gluten so that it does not cause symptoms in coeliac disease. There is no evidence that they are effective and they may be dangerous, as any exposure to gluten can increase the risk of developing one of the complications of coeliac disease.
Complications of coeliac disease
Although there is no once-and-for-all cure for coeliac disease, the symptoms can be kept away by having a diet completely free from gluten. Also, having a gluten-free diet reduces the risk of developing complications in the future. Apart from the symptoms already discussed, untreated or inadequately treated coeliac disease may lead to the following:
Developing 'thinning' of the bones (osteoporosis) due to the nutritional deficiencies which occur with coeliac disease.
Having a baby that has a low birth weight or is born prematurely if you become pregnant.
Weaknesses in the enamel coating of teeth.
Developing a type of cancer (called lymphoma) of the gut in later life. This is rare.
Apart from the complications listed above, people with coeliac disease also have an increased risk of developing other immune-related diseases (autoimmune diseases) such as the following:
A common mistake is to eat small amounts of food which contain gluten. This may be unintentional. However, some people wrongly think that a small amount won't matter. It does. A well-known example is thinking that the small amount of bread in a communion wafer will not matter. Even this small amount of gluten is sufficient to cause symptoms and to maintain the increased risks associated with coeliac disease detailed above.
Some people with coeliac disease may not realise they are taking small amounts of gluten. They may feel well, or ignore mild symptoms such as bloating or mild diarrhoea. Again, the increased risks (osteoporosis, etc) still remain if any gluten is eaten.
If you do not eat any gluten, then coeliac disease is not a serious condition and you can expect to be free of symptoms and to have a normal healthy lifespan. The increased risk of developing other autoimmune disorders reduces. Eating a gluten-free diet also reduces the risk of developing lymphoma.
Gluten-related neurological conditions
Some rare conditions of the brain and nervous system are slightly more common in people with coeliac disease, such as the following:
Gluten ataxia - a brain disorder that causes clumsiness and problems with balance and coordinating movements.
Gluten neuropathy - a peripheral neuropathy that causes areas of numbness.
Gluten encephalopathy - a brain disorder which affects the way the whole of the brain works causing headaches, unclear thinking and memory problems.
These conditions may be more likely to develop in people who don't follow a strict gluten-free diet but this is an area of current research.
Follow-up
Once you have been diagnosed with coeliac disease, you are likely to have regular follow-up appointments. This may initially be after three and six months to ensure that you are making satisfactory progress and managing your gluten-free diet. Depending on your age and other factors, you may be monitored to see if you have developed 'thinning' of the bones (osteoporosis). A review once a year with your doctor is recommended.
You can expect to live a life free of the symptoms of coeliac disease if you totally avoid gluten.
Patient picks for Bowel problems

Digestive health
Inflammatory bowel disease
Inflammatory Bowel Disease (IBD) is a term used to describe people who either have either of the two main types of IBD (Crohn's disease and ulcerative colitis). Both these conditions can cause inflammation of the colon and rectum (large bowel or large intestine) with similar symptoms, such as bloody diarrhoea, tummy (abdominal) pain, weight loss and poor appetite.
by Dr Colin Tidy, MRCGP

Digestive health
Crohn's disease
Crohn's disease is a condition that causes inflammation of the wall of the gut (gastrointestinal tract). Any part of the gut can be affected.
by Dr Toni Hazell, MRCGP
Further reading and references
- Coeliac Disease - Prescribable Product List; Coeliac UK.
- Guideline for the diagnosis and management of coeliac disease in children; British Society of Paediatric Gastroenterology, Hepatology and Nutrition with Coeliac UK (June 2013)
- Ludvigsson JF, Bai JC, Biagi F, et al; Diagnosis and management of adult coeliac disease: guidelines from the British Society of Gastroenterology. Gut. 2014 Aug;63(8):1210-28. doi: 10.1136/gutjnl-2013-306578. Epub 2014 Jun 10.
- Coeliac disease: recognition, assessment and management; NICE Guidance (September 2015)
- Laurikka P, Nurminen S, Kivela L, et al; Extraintestinal Manifestations of Celiac Disease: Early Detection for Better Long-Term Outcomes. Nutrients. 2018 Aug 3;10(8). pii: nu10081015. doi: 10.3390/nu10081015.
- Konig J, Brummer RJ; Is an enzyme supplement for celiac disease finally on the cards? Expert Rev Gastroenterol Hepatol. 2018 Jun;12(6):531-533. doi: 10.1080/17474124.2018.1473762. Epub 2018 May 11.
- Coeliac disease; NICE CKS, May 2020 (UK access only)
Continue reading below
Article history
The information on this page is written and peer reviewed by qualified clinicians.
Next review due: 22 May 2028
24 May 2023 | Latest version

Ask, share, connect.
Browse discussions, ask questions, and share experiences across hundreds of health topics.

Feeling unwell?
Assess your symptoms online for free
Sign up to the Patient newsletter
Your weekly dose of clear, trustworthy health advice - written to help you feel informed, confident and in control.
By subscribing you accept our Privacy Policy. You can unsubscribe at any time. We never sell your data.