Pigmented skin lesions
Peer reviewed by Dr Colin Tidy, MRCGPLast updated by Dr Sarah Jarvis MBE, FRCGPLast updated 25 Jan 2021
Meets Patient’s editorial guidelines
- DownloadDownload
- Share
- Language
- Discussion
Medical Professionals
Professional Reference articles are designed for health professionals to use. They are written by UK doctors and based on research evidence, UK and European Guidelines. You may find the Melanoma skin cancer article more useful, or one of our other health articles.
In this article:
Pigmented skin lesions can be considered as melanocytic neoplasms. The essential task is to exclude malignant melanoma. See also the separate Malignant Melanoma of Skin and Skin Biopsy Techniques in General Practice articles.
It is important to bear in mind that younger people in the UK are increasingly being affected by malignant melanoma, with over 900 diagnoses a year. This makes it the second most common cancer in those who are 25-49 years of age in the UK1 .
Continue reading below
Malignant melanoma
Image: a suspicious flat lesion, irregular in shape and pigmentation
Superficial spreading melanoma
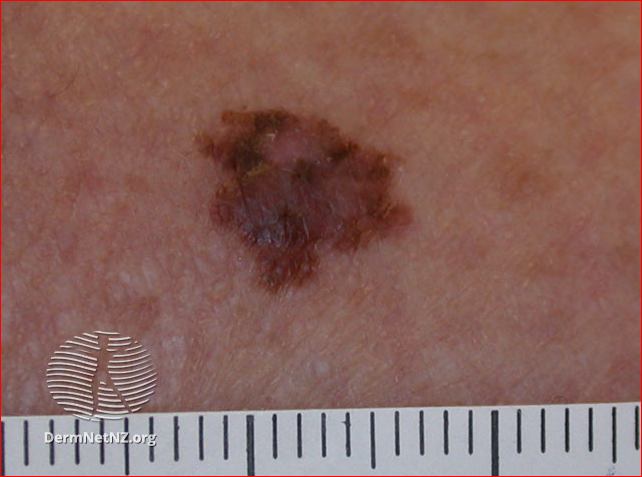
Superficial spreading melanoma image above:
DermNet New Zealand. This work is licensed under a
Creative Commons Attribution-NonCommercial-NoDerivs 3.0 New Zealand License.
Melanomas may have a variety of colours, including tan, dark brown, black, blue, red and, occasionally, light grey.
When assessing melanomas, factor in risk factors2 including:
Family history of melanoma.
Personal history of melanoma.
Immunosuppression.
Excessive UV exposure, including tanning beds.
7-point checklist
Use the 7-point weighted checklist for assessment of pigmented skin lesions3 :
Major features of lesions (two points each):
Change in size.
Irregular shape.
Irregular colour.
Minor features of lesions (one point each):
Largest diameter 7 mm or more.
Inflammation.
Oozing.
Change in sensation.
Lesions scoring three points or more in the 7-point checklist above are suspicious (if you strongly suspect cancer, any one feature is adequate to prompt urgent referral).
For low-suspicion lesions, undertake careful monitoring for change, using the 7-point checklist.
The National Institute for Health and Care Excellence (NICE) recommends ideally making measurements with photographs and a marker scale and/or ruler.
This guidance comes from the 2015 NICE guideline on detection of cancer. The guidance was updated in 2020, but there were no changes relevant to assessment and diagnosis of skin cancer3 .
ABCDE
An alternative aide-mémoire to the 7-point checklist described below is the 'ABCDE' list:
Asymmetry.
Border irregular.
Colour irregular.
Diameter greater than 7 mm.
Evolving.
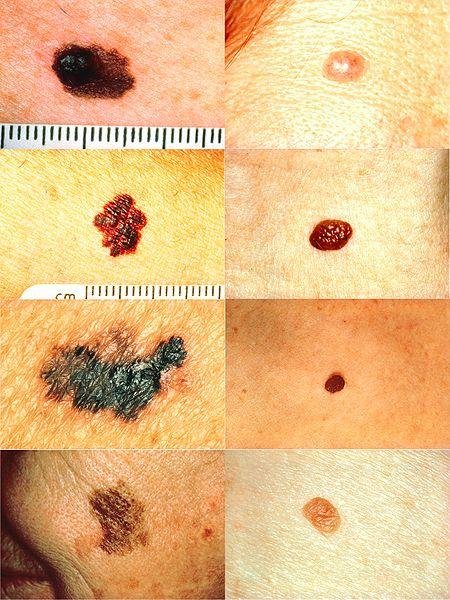
Melanoma vs normal mole
However, not all these features may be present and, if malignant melanoma cannot be excluded then excision biopsy is required4 .
Change in size: naevi may change in size over years but any change over weeks or months is suspicious.
Change in colour:
Melanomas often show irregular pigment in a lesion, with shades of black, brown, grey and pink. In nodular melanoma (see below) the lesion is often black throughout.
Rarely, a melanoma can present as a non-pigmented red nodule (amelanotic melanoma), which is more likely on the hands and feet.
Change in outline: melanomas often show a geographical outline with a sharp cut-off from normal skin.
Itching may be a late sign and is often unreliable, as many benign naevi intermittently itch.
Bleeding is also a late sign and is often present in advanced melanoma.
Melanoma in women occurs more commonly on the extremities and in men on the trunk or head and neck but it can arise from any site on the skin surface.
Examination of suspicious lesions should include a thorough assessment for other suspicious skin lesions, palpation for regional lymph nodes and examination of the abdomen for enlarged liver and/or spleen.
Nodular melanoma
Important information |
|---|
Nodular melanoma tends to lack the typical ABCDE melanoma warning signs and therefore may be diagnosed late with a much worse prognosis. Nodular melanomas tend to occur on the heads and necks of elderly sun-damaged men5 . A nodular melanoma is usually uniform in colour with early ulceration and bleeding. |
Image: pigmented lesion on an exposed area. It looks highly suspicious - the patient should be referred urgently
Nodular melanoma on an ear
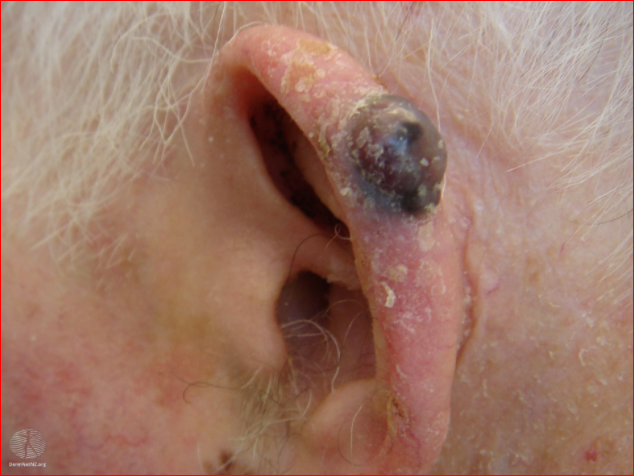
Nodular melanoma image above:
DermNet New Zealand. This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivs 3.0 New Zealand License.
Multiple cutaneous melanomas
It is estimated that approximately 7.4% of patients with melanoma develop multiple primary melanomas6 .
Subsequent melanomas may appear at the same time or up to decades after the first primary melanoma. In a 13-year follow-up study, 49% of subsequent melanomas were diagnosed within three years of the first6 .
The incidence of a second primary invasive melanoma has been shown to be increased in men and for initial melanoma thickness greater than 2 mm7 .
Lesions may be classified as synchronous if they present at the same time or within two months, or metachronous if the second melanoma presents later.
Other causes of pigmented skin lesions
Intradermal naevi
Also called common naevi. See also the separate Intradermal and Compound Naevi article.
Most adults will have approximately 30 moles which they have been acquiring from infancy. Naevi remain static whereas melanoma change in size, shape or colour over weeks or months. New common moles rarely develop after the age of 40 years and any that do are suspicious.
Typical features of common naevi are:
Symmetrical in area.
Even, brown colouring (light or dark).
Sharp margin.
<5 mm in diameter.
Profile varying from flat to pedunculated.
Anyone with >50 moles is at greatly increased risk of malignant melanoma, which may or may not arise from an existing mole. These patients need careful skin monitoring, including baseline skin photography. Any lesion that starts to change colour, bleed, itch, be painful or increase in size needs excisional biopsy.
Atypical moles
Also known as dysplastic naevi. They are found in approximately 1 in 12 white people and do not usually become evident until puberty. Unlike melanoma, atypical naevi are usually symmetrical and do not have a sharp edge with geographical border; asymmetry and sharp-edged borders are clear signs of malignant transformation8 . Atypical moles are easily mistaken for malignant melanoma because of their:
Lack of symmetry.
Lack of sharp margin.
Size >6 mm.
Variation in colour within the lesion.
Image: atypical naevus
Atypical naevus

Atypical naevus image above:
DermNet New Zealand. This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivs 3.0 New Zealand License.
Unlike common moles they continue to appear throughout life and occur in areas not often exposed to the sun - eg, buttocks. They are a strong, independent risk factor for malignant melanoma, conferring a 10-fold increased risk of malignant melanoma9 . This is especially the case when they are present in numbers (12% risk over ten years). Patients should be very careful with sunlight and undergo regular skin surveillance. Excision of dysplastic naevi is not performed routinely.
Congenital naevi
See the separate Congenital Pigmented Naevus article.
Very large congenital naevi are known as giant naevi. Patients with large congenital naevi have an increased risk of developing malignant melanoma, often by the age of 10 years. These appear either within the lesion or as CNS melanoma. Treatment is either excision or close monitoring. Laser treatment is also available10 .
Blue naevus
See the separate Blue Naevus article.
A blue naevus is a small blue or grey lesion, with an appearance similar to a mole. A newly occurring lesion may need excision biopsy to exclude nodular melanoma.
Image: blue naevus
Blue naevus
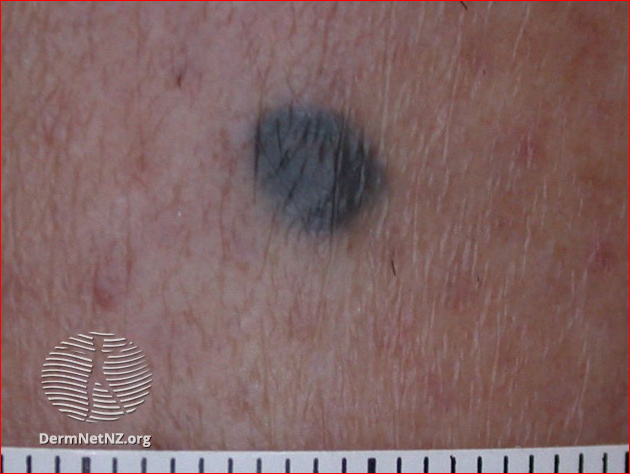
Blue naevus image above:
DermNet New Zealand. This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivs 3.0 New Zealand License.
Spitz naevus
Spitz naevi usually affect the face or limbs of young children. They initially grow rapidly but may then remain static for years. They often disappear spontaneously after a period of time11 .
Epidermal naevus
See the separate Epidermal Naevus and its Syndromes article.
Epidermal naevi may be congenital lesions or develop during the early years of life. They tend to grow during childhood and then stabilise during the teenage years. They may be localised to a small area or occur in more diffuse forms.
Epidermal naevus syndromes are a heterogeneous group of disorders characterised by the presence of one or more congenital hamartomatous ectodermal naevi of the skin with other organ involvement, including brain, eye and the skeleton.
Becker's naevus: this is a form of epidermal naevus (birthmark). It usually appears around puberty as a hyperpigmented patch, most often found on the upper trunk or shoulders.
Halo naevus
See the separate Halo Naevus article.
Usually, these consist of a central uniformly pigmented naevus, usually round or oval in shape, with a surrounding area of depigmentation of uniform width from the naevus's edge.
Junctional naevus
See the separate Junctional Naevus article.
Junctional naevi are often quite darkly pigmented and are macular or very thinly papular with only minimal elevation above the level of the skin.
They are an acquired lesion and as they age they can change their characteristics to that of compound naevi.
Compound naevus
See the separate Intradermal and Compound Naevi article.
Compound naevi arise from a flat (junctional) naevus that exists earlier in life. Pigmentation may be uneven within the naevus but is usually symmetrically distributed.
They are usually of a round/oval shape and roughly 2-7 mm in diameter. They may exist with a variable degree of pigmentation and even be the same colour as the surrounding skin.
Sebaceous naevus
See the separate Sebaceous Naevus article.
Usually a single hairless patch (round or linear) is noted on the scalp at birth or shortly afterwards. The classic appearance is velvety tan or yellow-orange.
Seborrhoeic wart
See the separate Seborrhoeic Wart article.
A flat-topped or warty-looking lesion that appears to be stuck on to the skin. They are usually pigmented, sometimes deeply. They may even be black.
Further reading and references
- Melanoma: assessment and management; NICE Guidance (July 2015 - last updated July 2022)
- Melanoma and pigmented lesions; NICE CKS, July 2022 (UK access only)
- Suspected cancer: recognition and referral; NICE guideline (2015 - last updated May 2025)
- Melanoma tests; Cancer Research UK
- Chamberlain A, Ng J; Cutaneous melanoma--atypical variants and presentations. Aust Fam Physician. 2009 Jul;38(7):476-82.
- Claeson M et al. Multiple Primary Melanomas: A Common Occurrence in Western Sweden. Acta Derm Venereol 2017; 97. Epub ahead of print Dec 13, 2016
- McCaul KA, Fritschi L, Baade P, et al; The incidence of second primary invasive melanoma in Queensland, 1982-2003. Cancer Causes Control. 2008 Jun;19(5):451-8. Epub 2008 Jan 1.
- Bataille V, de Vries E; Melanoma--Part 1: epidemiology, risk factors, and prevention. BMJ. 2008 Nov 20;337:a2249. doi: 10.1136/bmj.a2249.
- Goldstein A, Tucker M. Dysplastic Nevi and Melanoma. Cancer Epidemiol Biomarkers Prev. 2013 Apr; 22(4): 528–532.
- Dave R, Mahaffey PJ; Combined early treatment of congenital melanocytic naevus with carbon dioxide and NdYag lasers. Br J Plast Surg. 2004 Dec;57(8):720-4.
- Skin lesions, tumours and cancers; DermNet NZ
Continue reading below
Article history
The information on this page is written and peer reviewed by qualified clinicians.
Next review due: 24 Jan 2026
25 Jan 2021 | Latest version

Ask, share, connect.
Browse discussions, ask questions, and share experiences across hundreds of health topics.

Feeling unwell?
Assess your symptoms online for free