Dilated cardiomyopathy
Peer reviewed by Dr Colin Tidy, MRCGPLast updated by Dr Doug McKechnie, MRCGPLast updated 19 Jan 2023
Meets Patient’s editorial guidelines
- DownloadDownload
- Share
- Language
- Discussion
Dilated cardiomyopathy is a condition where the heart muscle becomes stretched and thin. The heart becomes enlarged (dilates) and pumps blood less well. Symptoms vary according to severity and the treatment depends on the type of symptoms and whether any complications develop. Some forms of dilated cardiomyopathy run in families.
In this article:
Video picks for Heart disease
A normal heart

In dilated cardiomyopathy, the heart muscle becomes stretched and thin. The ventricles then enlarge (dilate) because their muscular walls have become weak and floppy. This means the heart does not pump blood as strongly as normal. These changes often start in the left ventricle (the part of the heart which pumps blood around most of the body), and can then later affect the right ventricle (which pumps blood to the lungs) and the atria (the parts of the heart that receive blood from the veins).
Dilated cardiomyopathy is uncommon, but it is the most common type of cardiomyopathy. One estimate is that between 1 in every 2,500, to 1 in every 1,250 people have it; however, this might be an under-estimate, as it can take some time before it's diagnosed, and some people may have the early stages of the condition without any symptoms. It can affect children and adults. It is most common in middle-aged men.
What causes dilated cardiomyopathy?
For most people the cause is not known. This is sometimes called idiopathic dilated cardiomyopathy. Another possibility is that an unknown viral infection may be responsible. About one in four people with idiopathic dilated cardiomyopathy have a familial (hereditary) form. This means that several members of their family also have dilated cardiomyopathy. It is still not clear exactly how hereditary factors may work in this condition, but in some cases, specific gene problems have been identified.
There are many conditions which can cause damage or disease to heart muscle. Most are rare. They include:
Alcohol, drugs and other poisons
Up to 3 in 10 cases of dilated cardiomyopathy can be linked to alcohol. After years of heavy drinking, the cells of the heart muscle can become damaged and weakened. Also, heavy drinkers tend to eat poorly (see below). Some other chemicals, pesticides and recreational drugs (such as cocaine) have also been shown to weaken the heart muscle and cause dilated cardiomyopathy.
Poor diet
Being deficient in certain vitamins and minerals, especially vitamin B1 (thiamine), can weaken the heart muscle and lead to dilated cardiomyopathy. This is more common in poorer countries and also in people with heavy alcohol use, who tend to have problems with malnourishment.
Inflammation of the heart muscle (myocarditis)
This is a rare condition which can be caused by various infections. Some people with myocarditis develop dilated cardiomyopathy as a complication.
Pregnancy and childbirth
Heart muscle inflammation leading to dilated cardiomyopathy occurs very rarely. It is not known how or why pregnancy triggers this to occur. This is called peripartum cardiomyopathy.
Other diseases
The heart muscle can also be affected by other diseases which can affect various parts of the body. A dilated cardiomyopathy may then develop in addition to other symptoms of the disease. For example, dilated cardiomyopathy sometimes occurs with the following conditions:
Amyloidosis.
Some forms of muscular dystrophy.
Vasculitis.
Dilated cardiomyopathy symptoms
Back to contentsPeople with early dilated cardiomyopathy, causing mild enlargement of the heart, may not have any symptoms. However, if the heart becomes very dilated, symptoms will develop. Symptoms may develop gradually or quite quickly, depending on how quickly the disease progresses. Dilated cardiomyopathy may cause heart failure. The symptoms of heart failure include:
Shortness of breath
In mild cases, there might be breathlessness only on exertion - for example, people might feel more short of breath when running or walking up a hill, or find that they are limited by shortness of breath more than usual. With more severe heart failure, people can become short of breath whilst resting. Sometimes, people feel short of breath when lying flat, such as in bed, and have to sleep whilst propped up on several pillows.
Leg swelling
The build up (retention) of extra fluid in the body is called oedema. Oedema causes swelling. It usually mainly affects the legs, due to the effect of gravity. This tends to start with swelling of the feet at the end of the day. In time, the swelling may gradually affect the lower parts of the legs. It may go higher if it is not treated. For many people there is a gradual build-up of fluid. People with mild heart failure (or heart failure on treatment) may not have any fluid retention.
Tiredness
This can be very variable. Some people find that constant tiredness, fatigue, or exhaustion is the worst symptom they have.
Palpitations
A 'thumping heart' (palpitations) may sometimes occur. People may be aware that their heartbeat is fast and/or irregular. Some people develop chest pains. If the cardiomyopathy is a result of another cause (such as alcohol excess, myocarditis, etc) then they may also have various other symptoms.
Continue reading below
How is dilated cardiomyopathy diagnosed?
Back to contentsA doctor may suspect this condition because of:
The symptoms.
Findings on clinical examination - such as hearing signs of fluid in the lungs with a stethoscope, or finding swelling (oedema) in the legs.
Changes on a heart tracing (electrocardiogram, or ECG) - this is a tracing of the electrical activity of the heart.
Changes on a chest X-ray. This may show an enlarged heart, or fluid in the lungs.
Blood tests. Specifically, a blood test called NT-proBNP can be raised in heart failure.
Tests that can confirm the diagnosis of dilated cardiomyopathy include:
An ultrasound scan of the heart (echocardiogram). This test gives a lot of useful information - it can show an enlarged heart, determine how well the heart is pumping, and look for problems with the heart valves, amongst other things.
An MRI scan of the heart (cardiac MRI) might be offered by a specialist cardiologist, to look at the heart muscle in more detail.
Other tests might be requested to look for other causes of heart failure or dilated cardiomyopathy: for example, testing for iron levels (to look for haemochromatosis), or tests to look for problems with the blood supply to the heart (coronary artery disease). If no underlying cause is found then the diagnosis of idiopathic dilated cardiomyopathy is confirmed.
Other specialised tests might be recommended by cardiologists, depending on the situation.
There are genetic tests that look for a gene problem that could be causing dilated cardiomyopathy. These are increasingly being offered to people with dilated cardiomyopathy. These look for gene variants that we know are linked to dilated cardiomyopathy. It's likely that there are other genetic variants that cause dilated cardiomyopathy that we don't know about yet - and, therefore, can't test for - but this is an area where lots of research is happening, and we should know more and more as time goes on.
Family screening
People who have been diagnosed with idiopathic dilated cardiomyopathy should be asked about their family history of heart problems, to see if there is evidence of an inherited problem.
People who are a first-degree relative (mother, father, brother, sister, or child) of someone with idiopathic dilated cardiomyopathy may be advised to get tested for dilated cardiomyopathy by a cardiologist. This often involves a physical examination, blood tests, an electrocardiogram (ECG) and an echocardiogram.
If a genetic test has shown a specific gene problem in someone with dilated cardiomyopathy, their close relatives might be offered genetic testing to see if they also carry that gene. Genetic testing should only be done after a discussion with a specialist (called genetic counselling), so that people fully understand the benefits, limitations, and implications of testing before going ahead.
Dilated cardiomyopathy treatment
Back to contentsTreatment aims to ease symptoms if they occur, to prevent complications, and to slow or prevent the condition getting worse.. Treatment which may be suggested includes:
General lifestyle measures
Weight. Maintaining a healthy weight - such as reducing weight if living with overweight or obesity - can reduce the strain on the heart.
Alcohol. People with dilated cardiomyopathy might be advised not to drink alcohol, or only a small amount of alcohol, as it can have led to the heart muscle being weaker. If dilated cardiomyopathy is due to excess alcohol alone, then stopping drinking alcohol completely, before serious damage has occurred to the heart, can significantly improve the cardiomyopathy, and the heart may even completely recover.
Stop smoking. Smoking causes heart damage - including blockages in the arteries to the heart - which can make heart failure worse, and also cause heart attacks.
Medication
Various medicines are used to treat heart failure. These include:
A water tablet (diuretic), such as furosemide or bumetanide - occasionally combined with other different types of diuretic such as metolazone or bendroflumethiazide. These are really useful drugs that reduce fluid buildup in the body, and so can treat oedema (swelling) of the legs, and fluid in the lungs. However, research shows that they don't have an effect on people's risk of dying from heart failure in the long term - so, whilst these are very useful for treating symptoms of heart failure, other medicines should be used to improve the long-term prognosis for people with heart failure.
Other medicines improve symptoms of heart failure, but can also slow or sometimes stop the heart failure from getting worse. Research shows that these medicines help people with heart failure to live for longer. Heart failure specialists will therefore try to get people on the highest safe dose of these medicines that they can manage, depending on side-effects. These include:
Angiotensin-converting enzyme (ACE) inhibitors, such as lisinopril or ramipril. Most people with heart failure are prescribed an ACE inhibitor. There are several types and brands. These have lots of helpful effects on the heart and the kidneys, and reduce blood pressure.
Angiotensin receptor blockers (ARBs), such as losartan or candesartan. These are used if people can't take ACE inhibitors due to side-effects (for example, a troublesome dry cough).
Beta-blockers, such as bisoprolol or carvedilol. Beta-blockers protect the heart muscle.
Spironolactone or eplerenone. These are called 'mineralocorticoid antagonists'. They block the effect of a hormone which normally causes salt and water retention, and can also have protective effects on the heart as well.
SGLT2 inhibitors, such as dapagliflozin or empagliflozin. These medicines were originally developed to treat diabetes (they cause more sugar to enter the urine and be removed from the body). However, it's recently been shown that they also work well in treating heart failure, even in people without diabetes.
Sacubitril/valsartan (Entresto®). This is a combination of an angiotensin receptor blocker (valsartan), and sacubitril, which increases the levels of several natural hormones that reduce fluid retention and strain on the heart. Currently, in the UK, national guidelines advise that this is used only for people who are taking an ACE inhibitor or ARB, beta blocker, and mineralocorticoid antagonist, and still have heart failure symptoms. However, it might well become more commonly-used in future.
There are other drugs that are sometimes used in specific situations for heart failure, such as ivabradine, digoxin, and nitrates/hydralazine.
Treatment of arrhythmias
People with dilated cardiomyopathy are more likely to develop heart rhythm problems (arrhythmias). There are various treatment options, depending on what the heart rhythm problem is.
An anticoagulant (blood thinner) may be advised if someone has atrial fibrillation or has a very enlarged (dilated) heart. When the heart beats irregularly, there is an increased risk of blood clots developing, which can cause strokes. Anticoagulant treatment reduces the risk of this happening.
Sometimes, anti-arrhythmic drugs such as amiodarone are used to treat or prevent arrhythmias.
Other treatments for arrhythmias include:
Cardioversion. This involves an electric shock to the heart (given whilst under anaesthetic) to try to put the heart back into a normal rhythm.
Artificial pacemakers are used in certain types of arrhythmia where the heart beats abnormally slowly (such as complete heart block) and in certain other situations. An artificial pacemaker is a small device which is inserted just under the skin on the upper chest. Wires from the pacemaker are passed through veins into the heart chambers. The pacemaker can then stimulate the heart to maintain a regular normal heartbeat.
Implantable cardioverter defibrillators (ICDs) are sometimes used in certain situations - especially if for people at risk of developing serious and life-threatening arrhythmias. They are small devices which are similar to pacemakers and are inserted under the skin in the upper chest. Wires are passed through a vein to the heart. The device monitors the heartbeat. If it detects an abnormal rhythm, the device can send a small electrical shock to the heart to change it back to normal. These can be life-saving.
Cardiac resynchronisation pacemakers. Some people with severe heart failure and heart rhythm problems have problems with how the electrical impulses are sent to the heart muscles, causing them to pump in an inefficient way. Cardiac resynchronisation uses a special type of pacemaker that stimulates the heart in both the left and right ventricles at the same time (pacemakers usually only stimulate the right ventricle or right atrium), to make it pump more efficiently. The procedure to insert these is longer and more difficult than with standard pacemakers. These can improve symptoms and lifespan for some people with heart failure.
Surgery
Surgery has also been used to improve how efficiently the heart pumps. This is a rapidly developing area and there are various procedures used.
One such treatment is a left ventricular assist device (LVAD). These help the heart to pump blood around the body. These are only done for a very small number of people in the UK, though they are done a bit more frequently in the USA. The main role in the UK is to treat people who are waiting for a heart transplant, to keep them well whilst waiting for a donor heart.
Heart transplant
In some cases the condition progresses and severe heart failure develops. If this cannot be treated by the methods mentioned here, the only option for treatment is a heart transplant. This may not be an option for some people - for example, people who would not survive transplant surgery. Heart transplantation also requires an organ donation from someone who has recently died, and some people may wait months or years before a heart is available.
Continue reading below
Complications
Back to contentsComplications occur in some cases and include the following:
Arrhythmias
An arrhythmia is an abnormal rate or rhythm of the heartbeat. There are various types of arrhythmia and some are more serious than others. An arrhythmia can come and go and can cause bouts of a 'thumping heart' (palpitations), dizziness and other symptoms. Some arrhythmias become permanent. An arrhythmia called atrial fibrillation is the most common one that develops in people with dilated cardiomyopathy. See separate leaflets called Abnormal Heart Rhythms (Arrhythmias) and Atrial Fibrillation.
Blood clots
The blood flow through the heart is slower than normal, especially when the heart is very enlarged (dilated). This can lead to small blood clots developing within the chambers of the heart. These may travel in the bloodstream and get stuck in arteries of the body. This may lead to a stroke if a clot gets stuck in an artery in the brain, or to other problems. The risk of blood clots developing can be greatly reduced by taking an anticoagulant medicine (see above). An anticoagulant medicine reduces the ability of the blood to clot.
Sudden death
Sudden collapse and death without any warning occur rarely in people with dilated cardiomyopathy. This is probably due to a severe arrhythmia which may develop suddenly. Medication and/or an implantable cardioverter defibrillator (ICD) may reduce this risk.
Outlook
Back to contentsThe outlook with dilated cardiomyopathy varies and depends on the severity of the condition, and any other medical conditions a person has. However, the outlook for many people with dilated cardiomyopathy has improved a lot over a period of twenty years. This is due to new medical and surgical treatments.
In some people with dilated cardiomyopathy their heart starts pumping more efficiently again. This is seen after some of the treatments mentioned above.
Patient picks for Heart disease

Heart health and blood vessels
Acute coronary syndrome
The term 'acute coronary syndrome' (ACS) covers a range of disorders, including a heart attack (myocardial infarction) and unstable angina, that are caused by a sudden reduction of blood flow to part of the heart muscle. This is usually caused by a blood clot.
by Dr Rosalyn Adleman, MRCGP
Heart health and blood vessels
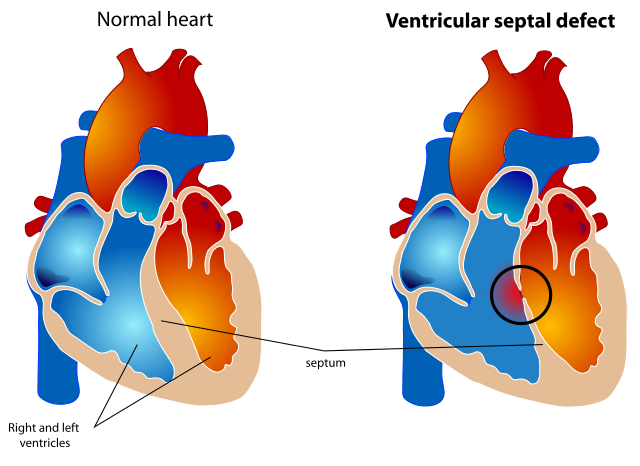
Ventricular septal defect
Ventricular septal defect (VSD) is a gap or defect in the septum between the heart's two lower chambers (ventricles). The septum is a wall that separates the heart's right and left side of the heart. Septal defects are sometimes called a 'hole' in the heart. It is the most common heart problem that babies are born with. Many defects in the ventricular septum close themselves and cause no problems. Otherwise, medicines or surgery can help. Most babies born with a defect in the septum have normal survival.
by Dr Hayley Willacy, FRCGP
Further reading and references
- Sanbe A; Dilated cardiomyopathy: a disease of the myocardium. Biol Pharm Bull. 2013;36(1):18-22.
- Implantable cardioverter defibrillators and cardiac resynchronisation therapy for arrhythmias and heart failure; NICE Technology Appraisal Guidance, June 2014
- Hershberger RE, Morales A; Dilated Cardiomyopathy Overview. GeneReviews®. University of Washington, Seattle. Updated September 2015.
- Guzzo-Merello G, Cobo-Marcos M, Gallego-Delgado M, et al; Alcoholic cardiomyopathy. World J Cardiol. 2014 Aug 26;6(8):771-81. doi: 10.4330/wjc.v6.i8.771.
- Chronic heart failure in adults - diagnosis and management; NICE Guidance (Sept 2018)
Continue reading below
Article history
The information on this page is written and peer reviewed by qualified clinicians.
Next review due: 18 Jan 2028
19 Jan 2023 | Latest version

Ask, share, connect.
Browse discussions, ask questions, and share experiences across hundreds of health topics.

Feeling unwell?
Assess your symptoms online for free
Sign up to the Patient newsletter
Your weekly dose of clear, trustworthy health advice - written to help you feel informed, confident and in control.
By subscribing you accept our Privacy Policy. You can unsubscribe at any time. We never sell your data.