Visual problems
Blurred vision
Peer reviewed by Dr Hayley Willacy, FRCGP Last updated by Dr Philippa Vincent, MRCGPLast updated 8 Jan 2025
Meets Patient’s editorial guidelines
- DownloadDownload
- Share
In this series:Macular degenerationEye floaters, flashes and haloesRetinal vein occlusionVitreous haemorrhageGiant Cell ArteritisSquint in children
Most people are concerned when they develop problems affecting their eyes, particularly if this affects their ability to see clearly. This leaflet describes most eye conditions which can affect vision, either temporarily or permanently. It explains what symptoms might be expected and what can be done about them.
In this article:
Continue reading below
What is visual loss?
Visual loss can be partial (meaning the vision is impaired or hazy or that the visual field is reduced) or complete (meaning all or part of the vision in one or both eyes is too poor for useful function). It may occur with or without pain, suddenly or gradually. All of these aspects depend on the cause. Some, but not all, visual loss is permanent and some, but not all, can be prevented.
Patient picks for Visual problems

Eye health
How to live with severe eye floaters
Eye floaters are usually thought of as a nuisance rather than a chronic condition. But for some people they can significantly affect quality of life. So how do you learn to live with them - and what are the treatment options?
by Elizabeth Sulis Kim

Eye health
Amblyopia (lazy eye)
Amblyopia (often called a lazy eye) means that vision in one eye does not develop fully during early childhood. Amblyopia is usually a correctable problem if it is treated early. Late treatment can mean that the sight problem remains permanent. A squint (strabismus) is one of the most common causes of amblyopia. Treatment of amblyopia involves making the lazy eye work harder to see. This is usually done by blocking the vision in the good eye with a patch or by making the eyesight in the good eye blurry by using atropine eye drops.
by Dr Philippa Vincent, MRCGP
How do we see?
Visual problems can arise from problems affecting different parts of the eye. Generally speaking, the further towards the back of the eye that problems occur, the more likely they are to have a long-lasting or permanent effect on your eyesight.
When looking at an object, light from the object passes through the cornea, then the lens, then through the fluid inside the ball (globe) of the eye, until it hits the retina at the back of the eye.
Side View of the Eye
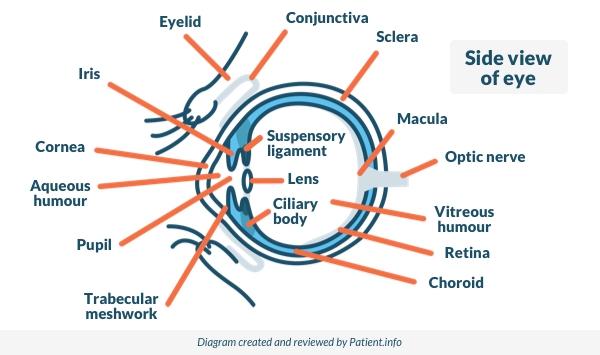
The lens of the eye acts like the lens in a camera. It helps to focus the light coming through the eye on to the retina, and in particular the macula. The macula is the part of the retina responsible for central vision - that is, the things being looked at directly. This is the part of the retina that is the most densely packed with rods and cones, which are the cells that help with "seeing".
Nerve signals pass from these "seeing" cells in the retina down nerve fibres in the optic nerve to the area of the brain responsible for putting together and interpreting these signals, enabling normal vision
For vision to be clear, the lens of the eye has to be clear (transparent).
Continue reading below
Causes of sudden painful visual impairment
There are several problems which can affect the surface of the eye and cause visual problems, although usually they mostly cause pain and redness without significant visual problems. However, if severe, they can cause permanent scarring of the clear window (cornea) which sits over the coloured part of the eye (the iris) and the pupil.
Conjunctivitis
Conjunctivitis is an inflammation or infection of the surface layer of the eye (the conjunctiva). Conjunctivitis does not normally affect the vision, other than to make things slightly blurry due to watering or discharge over the eyes. See the separate leaflets called Eye problems, Allergic conjunctivitis and Infective conjunctivitis for more details.
Foreign bodies - something in your eye
When a foreign body gets into the eye then the eye will water, the blinking reflex will be activated and the eye will be very irritable. Foreign bodies on the surface of the eye don't normally cause visual problems but they can do so in certain circumstances:
Active chemicals, such as strong acid, alkali or plaster dust, may damage the surface of the eye and cause scarring.
Penetrating injuries to the eye can affect vision. It's not easy for anything to penetrate its globe - but high-speed fragments from drilling or grinding can do so.
See the separate leaflet called Eye problems for more details.
Corneal scratches
The cornea is very, very sensitive and if it is scraped it hurts. Eyes are red and watery, vision is blurry and it may feel as though there is a foreign body in the eye.
The layers of clear cells that form the cornea can spread to fill in a shallow scratch over about 24 hours and they usually heal quickly. (Often the eye needs to be padded shut for this to happen, so that healing is undisturbed.)
Deeper scratches, such as can be formed by contact lenses which are not well looked-after or cleaned, can leave a permanent scar which can permanently affect vision. See the separate leaflet called Eye problems.
Corneal infection
Inflammation of the cornea is called keratitis. Infective keratitis may be caused by various organisms including bacteria and viruses, the latter being the most common cause. The cold sore virus and the chickenpox/shingles virus are common culprits. Bacteria usually only infect the cornea once the surface is damaged, such as following corneal abrasion or prolonged contact lens wear.
Conditions which reduce immunity also increase the risk of infective keratitis; this includes HIV/AIDS, immunosuppressive medication and some inflammatory autoimmune diseases.
Corneal infections can temporarily reduce visual clarity. In some cases they can thin the cornea or lead to corneal scarring. Generally speaking, the deeper the corneal infection, the more severe the symptoms and complications.
Corneal infection is caused by the cold sore (herpes simplex) virus and this can cause an ulcer on the surface of the eye. This causes redness, soreness and blurred vision. The pain can be very intense but the diagnosis can only be made by a clinician putting a stain in the eye in order to see the ulcer. The treatment of this type of ulcer is with antiviral eye drops; vision is not usually permanently affected.
Arc eye, snow blindness and photokeratitis
Photokeratitis is sunburn of the cornea. This is usually noticed several hours after exposure to the sun. Eyes are watery and feel gritty. Treatment is symptomatic. Cool, wet compresses and anti-inflammatory eye drops can be soothing. Eye protection, such as eye patches and sunglasses, is helpful. Avoidance of light for two to three days is usually needed to settle things down.
Snow blindness is common in mountaineers and skiers who forget their sunglasses. The brightness of white snow reflecting the sunlight is one factor. Another is the thinner atmosphere up at altitude which reduces protection from the sun's rays.
Arc eye is a similar condition from exposure to the bright light of an arc lamp; for this reason operators of these tools normally wear dark goggles.
Optic neuritis
Optic neuritis is uncomfortable and can be painful (particularly on eve movements). It can cause visual loss. This is sudden and may be partial or complete.
Patients sometimes describe their vision as disturbed or blackened. It can also cause loss of colour vision whilst vision is maintained. Optic neuritis is caused by inflammation of the optic nerve in the eye and it can involve one or both eyes. It can be a recurrent condition and there may be no underlying reason for it.
It can be a feature of multiple sclerosis (MS). Around 1 in 4 patients with optic neuritis who test negative for MS will go on to develop MS later.
MS is one possible cause, so people who have had more than one attack of optic neuritis will normally be offered testing to rule out MS. Other possible causes include Lyme disease, ulcerative colitis, and systemic lupus erythematosus (SLE - often just called lupus).
Optic neuritis usually resolves slowly by itself over a period of weeks or months, although vision may never return completely to normal.
Ophthalmic shingles
This condition occurs when shingles affects the eye and eye area. Shingles is known for causing a painful one-sided blistering rash on the body and, if this is on the face, it can affect the eye. When it does so, the eyelid and surface of the eye become very inflamed and blistered, and the eye is watery and red. Sometimes the internal structures of the eye are also affected - this is called uveitis.
Shingles of the eye can cause visual problems. If the condition is not treated promptly and well then permanent scarring can occur inside the eye. In addition, there is a small risk of sudden-onset (acute) glaucoma after a bad attack of ocular shingles.
Acute glaucoma
Acute glaucoma is a sudden rise in the pressure inside the eye. This causes severe pain, often bad enough to cause vomiting, with redness, watering and blurred vision. People often describe seeing rainbows around lights. The front of the eye can look cloudy and the pupil can look misshapen. The eye is said to feel as hard as a stone to touch.
Acute glaucoma is an emergency. If it is not treated then the pressure on the nerves at the back of the eye can damage them beyond recovery and the vision can be permanently lost. See the separate leaflet called Acute angle-closure glaucoma for more details.
Uveitis
Uveitis is a general term for inflammation of any or all of the structures in the eye. This means anything from the coloured part of the eye (the iris) backwards as far as the retina, including the rich layer of blood vessels which supplies the retina with nutrients. Uveitis causes a painful red eye. Vision is affected to differing degrees, depending on how far back the inflammation goes and how severe it is.
Anterior uveitis, involving mainly the iris, is the least serious. However, all types of uveitis can cause scar formation inside the eye and damage to the retina, with loss of vision. Many conditions can cause uveitis, including infection, injury and autoimmune diseases such as ankylosing spondylitis, although sometimes the cause is unknown. See the separate leaflet called Uveitis for more details.
Toxocara
Ocular toxocariasis is a rare infection in humans but it can cause permanent damage to the retina and loss of vision. Toxocara canis - also called dog roundworm - is a dog parasite which is widespread throughout the world. It usually causes no particular symptoms in dogs, but it can be spread fairly easily to humans, who usually catch it through contact with the stools (faeces) of infected dogs.
Toxocariasis is one of the reasons for strong public health campaigns for dog owners to clear up their dog waste. It is possible, although unusual, to be infected simply by stroking an infected dog's fur, as the parasite eggs can be in the fur. Once we ingest them the worm develops in the liver, the lungs and the back of the eye.
Toxocara eye infection usually occurs in children. The eye is usually red and painful with reduced vision, intolerance of light, and dark spots called 'floaters'. Patients are treated with medication to kill the worm plus anti-inflammatories for the eye, since much of the damage is caused by the inflammatory reaction to the worm. Some permanent damage to an area of the vision usually results.
Occasionally, old toxocara scars of undiagnosed past infection are found in the eye by chance.
Endophthalmitis
Endophthalmitis is a term for a catastrophic eye infection - that is, bacterial infection of the globe of the eye internally, usually following perforating injury or after surgery. It is essentially an extreme form of uveitis and it needs urgent treatment if vision is to be saved.
Causes of sudden painless visual impairment
Sudden loss of vision is always frightening, perhaps even more so when it is painless, as there is then no obvious cause. The cause of sudden painless visual loss is usually to do with the retina or with the blood vessels that serve it. Either they block, cutting off its blood supply, or they bleed, blocking the ability of the retina to 'see out' of the pupil.
Brain causes can also produce painless visual loss, including migraines, strokes and, very rarely, brain tumours.
Retinal detachment
The retina is the light-sensitive membrane at the back of the eye. It is attached in place by the network of blood vessels that feed it. In retinal detachment, the retina pulls away from its fixings and, in the process, becomes detached from its blood supply. When this happens the retinal cells die quickly and vision is lost.
The most common symptom is a shadow spreading across the vision of one eye. People say it is like a grey curtain coming down. See the separate leaflet called Retinal detachment for more details.
Blockage of blood vessels at the back of the eye (retinal vein and artery occlusion)
The retinal artery supplies the retina with oxygen; the retina is demanding and needs a good supply. If the retinal artery or one of its smaller branches blocks then the area of the retina it supplies quickly stops working. The main cause of arterial blockage (occlusion) is partial blockage of larger arteries by cholesterol and fats (a condition known as atherosclerosis). See the separate leaflet called Retinal artery occlusion for more details.
If a vein rather than an artery is blocked, the vision is lost more slowly and sometimes laser treatment can be used to prevent things becoming worse. See the separate leaflet called Retinal vein occlusion for more details.
Vitreous haemorrhage
This condition of sudden visual worsening or loss is caused by bleeding inside the eye. The jelly-like substance that fills the eye is called vitreous humour. When bleeding occurs into it light can no longer get through, so the vision in the affected eye goes totally dark.
In itself, vitreous haemorrhage is not serious, as the blood is eventually reabsorbed. This can take weeks or even months; eventually, however, the vision clears. However, it is a sign that the retina at the back of the eye is not healthy. See the separate leaflet called Vitreous haemorrhage for more details.
Giant cell arteritis (GCA)
This condition is usually seen in patients over 50 years of age, most of whom over 70. It is caused by inflammation of medium-sized blood vessels in the head and neck. When this affects the temporal artery, which supplies the optic nerve with nutrients, the artery can become blocked and the nerve stops working. See the separate leaflet called Giant cell arteritis for more details.
Migraine
Migraine can cause a temporary loss or alteration of vision which is referred to as an 'aura'. Usually patients experience a one-sided area of distorted or absent vision which affects both eyes but on the same side.
Visual symptoms in migraine do not usually last more than an hour. Patients may see wavy lines or blurred colours; one-sided headache may follow the visual symptoms. See the separate leaflet called Migraine for more details.
Stroke
It is uncommon for a stroke to cause severe sight impairment, as strokes do not commonly affect the part of the brain with which we see. However, if the back of the brain is affected by a stroke (which is a blood clot in the brain), temporary or permanent loss of vision may occur. The same symptoms can also follow severe head injury if the back of the brain is damaged.
Chorioretinitis
Chorioretinitis is infection or inflammation of the choroid and retina. The choroid is the pigmented, highly vascular layer of the globe of the eye, whose main function is to nourish the outer layers of the retina. Permanent damage to an area of the choroid will impair the blood supply to the underlying retina. The effect on vision depends on the location and size of the damaged area.
Chorioretinitis is usually caused by infection. Most cases occur in babies or in the womb (uterus) and most cases are caused by toxoplasmosis or cytomegalovirus (CMV). Toxoplasmosis is an important cause of chorioretinitis. It is an infection caused by a parasite called toxoplasma.
Cats are the main source of toxoplasmosis. You can catch it by coming into contact with cat droppings or infected meat. It can also be passed from mother to baby in the womb. See the separate leaflet called Toxoplasmosis for more details.
CMV is a virus which can affect the retina, causing retinitis. CMV is most dangerous to those with a weakened immune system (such as patients with HIV/AIDS) and causes blurred vision, floaters and areas of visual loss.
Toxocariasis is caused by dog (and occasionally cat) roundworm. Humans can become infected by ingestion of eggs in contaminated soil. In most cases the infection is eliminated and most people have no further symptoms. However, it can occasionally spread into other tissues, including the eye. Here it can scar the retina and cause decreased vision, squint, seeing floaters or 'bubbles', retinal detachment, optic neuritis and scarring.
Chorioretinitis in adults can have a number of other causes, including:
Intravenous drug use.
Some autoimmune conditions.
Continue reading below
Gradual visual loss
Pterygium
A pterygium is a raised, yellowish thickening on the white part of the eye (the sclera). It can grow and occasionally spread over the clear window of the eye (the cornea), so that it very occasionally obstructs vision. See the separate leaflet called Eye problems for more details.
Cataract
A cataract is a clouding of the lens of the eye. Vision becomes blurred, often misty. Early or slight cataracts may not cause symptoms and they generally become worse only slowly. Gradually, as they become more severe, they may cause people to be dazzled by lights (such as car headlamps) and colour vision may become washed out or faded. See the separate leaflet called Cataracts for more details.
Refractive error
Refractive error causes blurring, rather than loss of vision. This type of visual loss is very common and it occurs both in children and in adults. It is due to error in the optical power or focusing of the eye. It includes:
Long-sightedness (when distance vision tends to be preserved but near focus is blurred).
Short-sightedness (when near focus tends to be preserved but distance vision is blurred).
Astigmatism (when a distortion in the shape of the surface of the eye distorts the vision).
When the flexibility of the lens declines due to age, leading to a need for glasses for near vision (reading), the condition is known as presbyopia.
Severe refractive errors can mean patients lack useful vision unless corrected with spectacles or contact lenses. Some refractive errors can be corrected with laser treatment to the front of the eye.
Glaucoma
Acute glaucoma causes sudden painful loss of vision. See the separate leaflet for details.
Chronic glaucoma, which is much more common, is different. It is silent and symptomless until vision is damaged. Chronic glaucoma results from gradual increase in the fluid pressure in the eye and is often inherited.
Chronic glaucoma causes gradual but worsening damage to the optic nerve and a gradual loss of vision that occurs a bit at a time. People may notice very little at first, as central vision is not affected at first. By the time central vision is lost it is too late to improve it. Opticians can do tests to look for early signs of glaucoma that would not otherwise be picked up. See the separate leaflet called Chronic open-angle glaucoma for more details.
Macular degeneration (MD)
The macula is the spot on the back of the eye which sees the things that are looked at directly. Macular degeneration occurs when this area of the retina degenerates and loses function. This results in gradual loss of central vision, although the vision around the edge (peripheral vision) is not lost. See the separate leaflet called Age-related macular degeneration for more details.
Diabetic retinopathy
This is damage to the retina caused by the complications of diabetes, particularly where the diabetes has been present for more than ten years and where control has not been good. Most patients who have had diabetes for more than ten years have some degree of diabetic retinopathy but in the majority it is mild. See the separate leaflet called Diabetic retinopathy for more details.
Retinitis pigmentosa (RP)
'Retinitis pigmentosa' is the term for several inherited diseases which cause a gradual deterioration of the light-sensitive cells of the retina. Both rod (black/white, night vision and movement sensors) and cone (colour sensors) photoreceptors can be affected. Rod photoreceptor malfunction is the most commonly encountered problem in RP.
Symptoms often start in childhood with difficulty seeing in the dark. Peripheral vision is commonly lost first, although central vision can also be lost later. This eventually leads to impaired sight. Most types of RP become apparent between the ages of 10 and 30. There is currently no treatment which stops the progress of the condition, although complete loss of vision is uncommon.
Retinal dystrophy
Retinal dystrophies are a group of inherited (genetic) disorders which result in changes to the retina which may affect vision. They are fairly rare conditions. The most common and best known example is RP (see above). Unlike RP, most retinal dystrophies tend particularly to affect the macula - the part of the retina where the centre of our vision is formed. They tend, therefore, to cause gradual loss of vision and of perception of colour before the age of 20 years.
Rarer cause of visual loss
There are many rarer causes of visual loss, some caused by infections (such as fungi), inflammation (such as sarcoidosis) or damage to the optic nerve by medicines, street drugs or chemicals, including meths (methanol). Severe thyroid eye disease related to hyperthyroidism can affect vision through pressure on the optic nerve. There are also a number of inherited rare causes of gradual visual loss, including RP (see above) and albinism.
Brain or eye tumour
Brain or eye tumours are rarely the cause of loss of vision. Gradual loss of vision can be a symptom of a growing tumour. However, gradual loss of vision is very common but brain and eye tumours are very, very rarely the cause.
Summary
The eye is a clever magnifying device that takes light from the world around us and makes an image of our surroundings on a light-sensitive membrane that is then sent to the brain. Essentially, the eye functions like a camera, in which the retina is the film. What happens beyond that is to do with the developing. Any damage to the component parts or blockage to the route of light can affect vision.
Visual problems are always taken seriously. It requires investigation and diagnosis. It is best to see an optician about gradual worsening of visual problems but to attend an emergency department with any sudden or severe visual loss.
Dr Mary Lowth is an author or the original author of this leaflet.
Further reading and references
- Snellen Chart; Living Well with Low Vision
Article history
The information on this page is written and peer reviewed by qualified clinicians.
Next review due: 7 Jan 2028
8 Jan 2025 | Latest version

Ask, share, connect.
Browse discussions, ask questions, and share experiences across hundreds of health topics.

Feeling unwell?
Assess your symptoms online for free